ABSTRACT
Objective: To assess the efficacy of cariprazine, a dopamine D3–preferring D3/D2 and serotonin 5-HT1A receptor partial agonist, as adjunctive treatment for patients with major depressive disorder (MDD) and inadequate response to ongoing antidepressant therapy (ADT).
Methods: This randomized, double-blind, placebo-controlled study was conducted from November 2018 to September 2021. Adults with MDD per DSM-5 criteria were randomized (1:1:1) to cariprazine 1.5 mg/d or 3 mg/d plus ADT, or placebo plus ADT. The primary and secondary endpoints were change from baseline to week 6 in Montgomery-Asberg Depression Rating Scale (MADRS) total score and Clinical Global Impressions–Severity of Illness (CGI-S) score, respectively.
Results: A total of 249 placebo-, 250 cariprazine 1.5 mg/d–, and 251 cariprazine 3 mg/d–treated patients were included in the modified intent-to-treat population. At week 6, the least squares mean change in MADRS total score was −13.8 for cariprazine 1.5 mg/d, −14.8 for cariprazine 3 mg/d, and −13.4 for placebo; differences versus placebo were not statistically significant. Mean change from baseline in CGI-S scores at week 6 was not significant for cariprazine versus placebo, although a trend toward significance was observed for 3 mg/d (P = .0573 [not adjusted for multiplicity]). Common treatment-emergent adverse events (≥ 5% either cariprazine group and twice placebo) were akathisia and insomnia.
Conclusions: There were no statistically significant differences for cariprazine 1.5 or 3 mg/d versus placebo on the primary or secondary outcomes. Cariprazine was generally well tolerated, and no new safety concerns were detected.
Clinical Trials Registration: ClinicalTrials.gov identifier NCT03739203
J Clin Psychiatry 2023;84(5):22m14643
Author affiliations are listed at the end of this article.
Major depressive disorder (MDD) is a burdensome psychiatric disorder and a leading cause of disability and mortality worldwide.1–3 Unfortunately, a significant proportion of people with MDD do not achieve adequate response to antidepressant treatment (ADT).4–6 For example, in the largest real-world effectiveness trial evaluating treatment in patients with MDD (ie, Sequenced Treatment Alternatives to Relieve Depression [STAR*D]), only one-third of patients achieved remission with initial ADT, with decreasing rates with each successive monotherapy ADT.5 Inadequate treatment response and residual symptoms are associated with worse clinical outcomes (eg, higher rates of relapse), higher medical costs, and increased health care resource utilization.7,8
Meta-analyses support the adjunctive use of atypical antipsychotics in cases of inadequate response to ADT.9–13 Cariprazine (approved December 2022), aripiprazole, quetiapine extended-release (XR), and brexpiprazole are currently approved for adjunctive treatment of MDD. Cariprazine, a dopamine D3–preferring D3/D2 receptor partial agonist and a serotonin 5-HT1A receptor partial agonist, is also US Food and Drug Administration (FDA)–approved for the treatment of adults with schizophrenia and manic, mixed, or depressive episodes of bipolar I disorder. Its unique pharmacology, as well as evidence of antidepressant-like activity in animal models,14–16 suggested that cariprazine may be efficacious as adjunctive treatment in MDD.
Cariprazine has demonstrated efficacy as adjunctive therapy to an antidepressant in one 8-week flexible-dose study17 and a recent fixed-dose study in patients with inadequate response to ADT alone.18 Two earlier flexible-dose studies,19,20 in which adjunctive cariprazine was not significantly different from placebo on the primary outcome across a range of dose groups, were also published. Results of an additional phase 3 fixed-dose study evaluating cariprazine 1.5 and 3 mg/d plus ADT in patients with MDD and inadequate response to ADT are reported here.
METHODS
This study (ClinicalTrials.gov identifier NCT03739203) was conducted at 107 sites in the United States, Canada, Poland, Serbia, Slovakia, Czech Republic, and Finland from November 2018 to September 2021. The protocol was approved by an independent ethics committee (IEC)/institutional review board (IRB). The study was conducted in compliance with the International Conference on Good Clinical Practice Guideline and the Declaration of Helsinki; all patients provided written informed consent.
Study Design
In this phase 3, multicenter, randomized, double-blind, placebo-controlled, parallel-group study of adjunctive cariprazine in adults with MDD, there was a 14-day screening/washout period, followed by a 6-week double-blind treatment period and a 4-week safety follow-up. During screening, patients withdrew from prohibited medications (up to an additional 7 days was allowed if needed) and they continued taking ongoing ADT at the same dose to which they were having an inadequate response; patients taking more than 1 ADT were required to discontinue all but 1 ADT prior to baseline. Eligible patients were randomized (1:1:1) to once-daily cariprazine 1.5 mg/d plus ADT, cariprazine 3 mg/d plus ADT, or placebo plus ADT; ADT was continued at the baseline dose. All patients randomized to cariprazine initiated treatment at 1.5 mg/d; patients randomized to 3 mg/d uptitrated at week 2 and maintained the 3-mg/d dose through week 6. Eligible patients were randomly assigned to double-blind treatment by an automated interactive web response system; study treatments were dispensed in identical blister cards to maintain masking throughout the study.
Patients
Male or female patients (aged 18–65 years, inclusive) met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5),21 criteria for MDD based on the Structured Clinical Interview for DSM-5 (SCID-5).22 The current major depressive episode (MDE) was ≥ 8 weeks’ and < 24 months’ duration. Included patients were required to have inadequate response (< 50% improvement) to 1 to 3 ADTs of adequate dose and duration (ie, continuous ADT for 6 weeks, with dose above the minimum labeled dose for ≥ 3 of the 6 weeks) in the current MDE, as measured by the modified Antidepressant Treatment Response Questionnaire (ATRQ).23 Clinical inclusion criteria required a 17-item Hamilton Depression Rating Scale (HDRS17)24 total score ≥ 22 and Item 1 (apparent sadness) score ≥ 2.
Patients were excluded for inadequate response to > 3 ADTs during the current MDE, current psychiatric diagnosis other than MDD, history of manic/hypomanic episodes, Young Mania Rating Scale (YMRS)25 score ≥ 12, substance-related disorders (past 3 months), and suicide risk or attempt (past year). Any concurrent medical condition that might confound study results was exclusionary. Eligibility criteria were confirmed by an independent SAFER interview.26 Psychotropic medications were prohibited, except for allowed rescue medications: zolpidem, zaleplon, eszopiclone, zopiclone, chloral hydrate, or suvorexant (for insomnia); benztropine, biperiden, diphenhydramine, trihexyphenidyl, or propranolol (for extrapyramidal symptoms [EPS]); and lorazepam up to 2 mg/d or equivalent benzodiazepine (for agitation, restlessness, or hostility).
Outcome Measures
The primary efficacy assessment was the Montgomery-Asberg Depression Rating Scale (MADRS),27 which was administered at each visit (weeks 0 [baseline], 1, 2, 4, 6). Other efficacy measures included the Clinical Global Impressions–Severity of Illness scale (CGI-S) and CGI-Improvement
scale (CGI-I)28 (each visit), HDRS17 (weeks 0, 6), and Hamilton Anxiety Rating Scale (HARS)29 (weeks 0, 4, 6).
Safety assessments included adverse events (AEs) and vital signs (every visit); physical examinations, clinical laboratory tests, electrocardiograms (ECGs; weeks 0 and 6); and EPS scales (Abnormal Involuntary Movement Scale [AIMS],30 Barnes Akathisia Rating Scale [BARS],31 and Simpson-Angus Scale [SAS]32; weeks 0–6). Other safety evaluations included the YMRS (treatment-emergent mania; weeks 0, 6) and Columbia–Suicide Severity Rating Scale (C-SSRS)33 (every visit).
Statistical Analysis
Efficacy analyses were based on the modified intent-to-treat (mITT) population (patients who received ≥ 1 dose of study drug and had ≥ 1 postbaseline assessment of MADRS total score). The primary and secondary efficacy parameters were change from baseline to week 6 in MADRS total score and CGI-S score, respectively. Primary efficacy was analyzed using a mixed-effects model for repeated measures (MMRM) with treatment group, country, ADT failure category, visit, and treatment group–by-visit interaction as fixed effects and baseline MADRS total score and score-by-visit interaction as covariates. An unstructured covariance matrix was used to model the covariance of within-patient MADRS scores, and the Kenward-Roger approximation34 was used to estimate denominator degrees of freedom. Sensitivity analyses for the primary endpoint were performed using the pattern mixture model to impute missing postbaseline scores and a copy-reference approach. CGI-S score change from baseline was analyzed using an MMRM similar to the primary efficacy analysis.
The truncated Hochberg procedure with truncation parameter of 0.9 (primary endpoint) and the regular Hochberg procedure (secondary endpoint) were used to control the overall type I error rate at a .05 level (2 sided) for multiple comparisons of 2 active doses with placebo for the primary endpoint and the key secondary endpoint. No multiple comparison testing of the key secondary endpoint was performed for claims of statistical significance unless the primary efficacy endpoint was statistically significant for at least 1 cariprazine dose versus placebo (P < .05). By-visit changes from baseline were analyzed by MMRM and an analysis of covariance (ANCOVA) model with last observation carried forward (LOCF) imputed for MADRS total, CGI-S, HARS total, and HDRS17 total scores with treatment group, country, and ADT failure category as factors and baseline value as covariate. MADRS response (≥ 50% reduction from baseline) and remission (total score ≤ 10) were analyzed using logistic regression with LOCF imputation. Assuming an effect size of 0.286 and a dropout rate of 15% at week 6, it was determined that a sample size of 250 participants per arm provided approximately 90% statistical power to show that at least 1 cariprazine dose was significant versus placebo in the primary endpoint.
Safety assessments were based on the safety population (randomized patients who received ≥ 1 dose of study drug) and analyzed descriptively. Scale-derived treatment-emergent parkinsonism (SAS score ≤ 3 [baseline] and > 3 [postbaseline]), akathisia (BARS score ≤ 2 [baseline] and > 2 [postbaseline]), and mania (YMRS total score ≥ 16 [postbaseline]) were assessed.
RESULTS
Patient Characteristics and Disposition
There were 750 patients in the mITT population (placebo = 249, cariprazine 1.5 mg/d + ADT = 250; cariprazine 3 mg/d + ADT = 251) (Figure 1). Approximately 92% of patients completed the study; completion rates were similar across groups (Figure 1). Baseline demographic and disease characteristics were generally similar across groups (Table 1). Mean baseline MADRS total (range, 32.0–33.0) and CGI-S (range, 4.6–4.7) scores indicated a moderately to severely ill population; mean duration of the current MDE ranged from 6 to 7 months.
Efficacy Outcomes
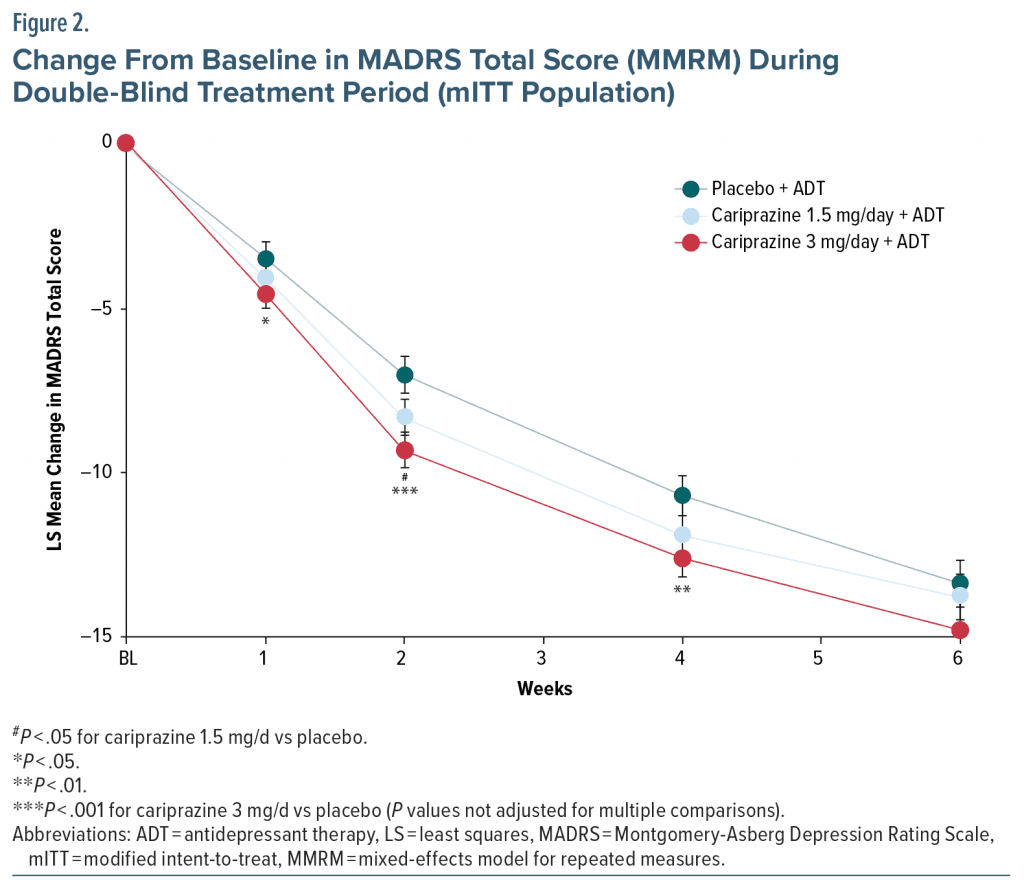
At week 6, the least squares (LS) mean change from baseline in MADRS total score (primary efficacy) was −13.8 for cariprazine 1.5 mg/d, −14.8 for cariprazine 3 mg/d, and −13.4 for placebo; LS mean differences (LSMDs) versus placebo were not statistically significant for either cariprazine dose (Figure 2, Table 2). At several earlier time points, LSMDs with 95% confidence intervals (95% CIs) favored cariprazine over placebo, but the differences were not adjusted for multiple comparisons and were therefore not statistically significant (Figure 2). Results of the sensitivity analysis were consistent with the primary results.
Because neither dose of cariprazine was significantly different from placebo on the primary endpoint, no testing of the key secondary endpoint was performed for claims of statistical significance. At week 6, LSMDs in mean change from baseline in CGI-S scores were not statistically significant for cariprazine versus placebo, although a trend toward significance was observed for 3 mg/d (−0.2 [−0.43 to 0.01], P = .0573 [not adjusted for multiplicity]) (Table 2). At week 6, no significant differences were observed for cariprazine versus placebo on additional efficacy outcomes (eg, HDRS17, HARS, CGI-I), rates of MADRS response and remission, or CGI-I response (not adjusted for multiplicity).
Safety Outcomes
Mean (SD) duration of double-blind treatment was 40.9 (7.0) days in the placebo group, 41.2 (6.2) days in the cariprazine 1.5 mg/d group, and 40.1 (8.5) days in the cariprazine 3 mg/d group.
Adverse events. During double-blind treatment, the most common treatment-emergent adverse events (TEAEs) (≥ 5% and twice placebo) were akathisia and insomnia (Table 3). Most TEAEs (> 92% in all groups) were mild or moderate in severity; < 1% of patients in any group experienced a serious TEAE, and none were related to treatment. Discontinuation due to TEAEs occurred more frequently with cariprazine than with placebo, with akathisia the only TEAE that led to discontinuation for > 1 patient in any group (1.5 mg/d = 2 [0.8%]; 3 mg/d = 6 [2.4%]; placebo = 2 [0.8%]). Treatment-emergent mania (YMRS total score = 20) was reported 1 placebo patient (end of treatment visit) and no cariprazine patients. No deaths occurred during double-blind treatment; 1 death in the placebo-plus-ADT group occurred during safety follow-up (cause unknown, considered not related to treatment).
Extrapyramidal symptoms. The incidence of EPS-related TEAEs excluding akathisia/restlessness was generally similar across treatment groups; akathisia/restlessness was higher in both cariprazine groups versus placebo (Table 3). All EPS-related TEAEs were mild or moderate in severity. Scale-derived treatment-emergent akathisia (BARS baseline score ≤ 2 and postbaseline score > 2) was reported in 13 (5.2%) placebo-, 27 (10.8%) cariprazine 1.5 mg/d–, and 30 (12.0%) cariprazine 3 mg/d–treated patients. Scale-derived parkinsonism (SAS baseline score ≤ 3 and postbaseline score > 3) was reported in 3 (1.2%) placebo-, 4 (1.6%) cariprazine 1.5 mg/d–, and 4 (1.6%) cariprazine 3 mg/d–treated patients. Rescue medication use was greater with cariprazine (3 mg/d = 10.0%; 1.5 mg/d = 9.6%) than with placebo (3.6%); benzodiazepine use was low (≤ 2%) across groups.
Laboratory parameters, vital signs, and electrocardiogram assessments. The incidence of treatment-emergent changes from baseline in metabolic parameters was generally similar across treatment groups (Supplementary Tables 1 and 2). No patients met Hy’s Law criteria (alanine aminotransferase [ALT] or aspartate aminotransferase [AST] ≥ 3 times the upper limit of the normal range [ULN] and total bilirubin ≥ 2 times ULN and alkaline phosphatase < 2 times ULN). Small mean changes from baseline in serum cholesterol and fasting glucose values were observed in all 3 treatment groups; mean changes from baseline in serum insulin and triglyceride values were greater with cariprazine than with placebo, but high interpatient variability was observed in all treatment groups. Mean change from baseline in weight was < 1 kg in all groups (placebo = 0.20 kg; cariprazine 1.5 mg/d = 0.68 kg, cariprazine 3 mg/d = 0.66 kg). Weight increase ≥ 7% from baseline was most frequent with cariprazine 3 mg/d, but low across groups in general (placebo = 0.8%, cariprazine 1.5 mg/d = 0.4%, cariprazine 3 mg/d = 2.0%). There were no clinically important mean changes from baseline in blood pressure, pulse rate, or incidence of orthostatic hypotension across groups. No patient in any treatment group had corrected QT interval by Fredericia (QTcF) increase > 60 msec from baseline or QTcF interval > 500 msec; 5 patients (1.5 mg/d = 1; 3 mg/d = 2; placebo = 2) had shifts from normal baseline to clinically significant abnormal ECG at the end of treatment.
Suicidality. During double-blind treatment, similar percentages of C-SSRS–rated suicidal ideation were reported across groups (1.5 mg/d = 5.2%; 3 mg/d = 7.6%; placebo = 6.4%); most events were in the least serious category (“wish to be dead”), and no suicidal behavior or completed suicide occurred. During safety follow-up, the incidence of suicidal ideation was higher in the cariprazine 1.5 mg/d group (5.4%) than in 3 mg/d and placebo groups (2.1% both); 1 patient in the 1.5 mg/d group had a suicide attempt (reported as an SAE) that was considered possibly related to treatment.
DISCUSSION
In this phase 3 clinical trial in patients with MDD, differences in mean change from baseline in MADRS total score, the primary efficacy endpoint, were not statistically significant for either adjunctive cariprazine dose at week 6. Improvement in MDD severity was suggested by a lower CGI-S score for cariprazine 3 mg/d versus placebo, with differences trending toward significance at week 6 (P = .0573). MADRS response was achieved by 46% and 48% of cariprazine 1.5 mg/d and 3 mg/d patients, respectively, with high placebo response (41%) potentially affecting the ability to achieve a cariprazine-placebo difference.
Although no statistically significant differences versus placebo were observed, a trend for early effects was observed for cariprazine on several outcome measures. In earlier weeks of the study, LSMDs in change from baseline in MADRS total score favored cariprazine 3 mg/d (weeks 1, 2, and 4) and cariprazine 1.5 mg/d (week 2) versus placebo, but the differences were not adjusted for multiple comparisons and were therefore not statistically significant. The 2-point difference in MADRS total score mean change in favor of cariprazine 3 mg/d versus placebo at weeks 2 and 4 suggested that improvement in depressive symptoms was clinically relevant at these time points.35 Rates of MADRS response and remission also suggested reduction in depressive symptoms, although placebo response was high.
Interestingly, a dose response in favor of cariprazine 3 mg/d was observed on several outcomes in this study, which was consistent with a previous positive flexible-dose cariprazine adjunctive treatment trial in MDD.17 In that previous study, change from baseline to week 8 in MADRS total score was significantly greater for cariprazine 2.0–4.5 mg/d versus placebo (LSMD = −2.2; adjusted P = .0114) but not for cariprazine 1.0–2.0 mg/d (LSMD = −0.9; adjusted P = .2404); the mean daily dose in the effective cariprazine treatment arm was ~3 mg/d, which supports a potential treatment effect for this daily dose. Furthermore, a positive fixed-dose trial in patients with MDD18 found a statistically significant difference in change from baseline to week 6 in MADRS total score (primary efficacy parameter) for cariprazine 1.5 mg/d versus placebo, but not for cariprazine 3 mg/d, with a trend toward early effects again noted; a significantly higher percentage of cariprazine 1.5 mg/d patients than placebo-treated patients also achieved MADRS response (≥ 50% MADRS total score reduction) at week 6. Collectively, these results suggest that adjunctive cariprazine 1.5 and 3 mg/d can be an effective treatment for depressive symptoms in patients with MDD and inadequate response to ongoing ADT; some patients may benefit from the higher dose in the recommended dose range. Of additional interest, the efficacy of cariprazine 1.5 and 3 mg/d has also been demonstrated in 3 randomized clinical trials in bipolar I depression.36–38
Although not significantly different from placebo, the magnitude of MADRS total score reduction at week 6 for both doses of cariprazine plus ADT (1.5 mg/d = −13.8; 3 mg/d = −14.8) in the current study was comparable to what was observed in the positive, fixed-dose study of adjunctive cariprazine in MDD (1.5 mg/d = −14.1; 3 mg/d = −13.1).18 Higher placebo response in the current study compared with the positive study (−13.4 vs −11.5) may have contributed to the lack of statistically significant differences. Further, since our trial was conducted during the COVID-19 pandemic, a time of significant social isolation for many individuals, it is possible that study participation and in-person interactions with study personnel may have had nonspecific therapeutic benefits, which also could have inflated placebo response.
Cariprazine 1.5 mg/d and 3 mg/d as adjunctive treatment to ADT was generally safe and well tolerated. AEs reported in ≥ 5% of participants in either cariprazine plus ADT dose group and at least 2 times the rate of placebo plus ADT were akathisia and insomnia; the incidence of EPS-related AEs (excluding akathisia and restlessness) were similar across treatment groups. Akathisia was the only TEAE that led to discontinuation of more than 1 patient in any treatment group. C-SSRS data indicated no increased risk of suicidal ideation or behavior with cariprazine plus ADT compared with placebo plus ADT, and there were no clinically relevant changes from baseline in laboratory test results, laboratory parameters, or body weight. The safety and tolerability of cariprazine in this study were consistent with the known safety profile of cariprazine in long-term adjunctive use in MDD39 and across its indications.40–42
Limitations of this study include short duration and lack of an active comparator. Patients had prior ADT treatment failure and were required to meet strict inclusion/exclusion criteria (eg, current MDE duration ≥ 8 weeks and < 24 months, inadequate response to 1 to 3 ADTs), which may limit generalizability to other patient populations. Although included patients had inadequate response to ongoing ADT at baseline, continued use of ADT may have contributed to reduction of depressive symptoms during the trial. In psychiatric clinical trials, high placebo response and poor signal detection have been associated with several factors, including the number of study sites, number of treatment arms, and number of study visits. As such, it is possible that factors in addition to those already discussed may have influenced our ability to detect a treatment effect. Lastly, although trends toward early improvement with cariprazine were observed on several efficacy measures, the effect of cariprazine at early visits was not a primary or secondary outcome; differences versus placebo were not corrected for multiple comparisons and were therefore not statistically significant.
Although there were no statistically significant differences for adjunctive cariprazine plus ADT versus placebo plus ADT on the primary efficacy outcome, some positive trends for cariprazine plus ADT in patients with MDD and inadequate response to antidepressant monotherapy were seen in this failed study. Cariprazine was generally safe and well tolerated, with no new safety concerns identified. Two positive studies support the adjunctive use of cariprazine with ADT for the treatment of depressive symptoms in patients with MDD, and some outcomes from this trial further inform its potential use in MDD.
Article Information
Published Online: August 16, 2023. https://doi.org/10.4088/JCP.22m14643
© 2023 Physicians Postgraduate Press, Inc.
Submitted: August 26, 2022; accepted June 15, 2023.
To Cite: Riesenberg R, Yeung PP, Rekeda L, et al. Cariprazine for the adjunctive treatment of major depressive disorder in patients with inadequate response to antidepressant therapy: results of a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2023;84(5):22m14643.
Author Affiliations: Atlanta Center for Medical Research, Atlanta, Georgia (Riesenberg); AbbVie, Madison, New Jersey (Yeung, Rekeda, Kerolous); Massachusetts General Hospital, Boston, Massachusetts (Sachs, Fava); Signant Health, Blue Bell, Pennsylvania (Sachs).
Corresponding Author: Paul P. Yeung, MD, MPH, PO Box 1276, Southeastern, PA 19399-1276 ([email protected]).
Relevant Financial Relationshipps: Dr Riesenberg was an investigator on this study and received financial support from AbbVie, which funded the study. Dr Yeung was an employee of AbbVie at the time of the study and may hold stock. Drs Rekeda and Kerolous are employees of AbbVie and may hold stock. Dr Sachs is a full-time employee of Signant Health; has been a consultant to Abbott Laboratories, Allergan, Astellas, AstraZeneca, Blackthorn, Bristol-Myers Squibb, Intra-Cellular Therapies, Otsuka, Pfizer, Sunovion, Takeda, Wyeth, and Repligen; and has served on speakers or advisory boards for Abbott Laboratories, Allergan, Astellas, Sanofi, Pfizer, Sunovion, and Takeda. Dr Fava’s disclosures can be viewed online at https://mghcme.org/app/uploads/2022/04/MF-Disclosures-Lifetime-updated-April-2022.pdf.
Funding/Support: This research was funded by AbbVie.
Role of the Funders/Sponsors: AbbVie participated in the study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the publication. All authors had access to relevant data and participated in the drafting, review, and approval of this publication. No honoraria or payments were made for authorship.
Previous Presentation: Poster presented at the American Society of Clinical Psychopharmacology annual meeting; Scottsdale, Arizona; June 1, 2022.
Acknowledgments: AbbVie and the authors thank the patients, study sites, and investigators who participated in this clinical trial. AbbVie and the authors thank Willie Earley, MD, formerly of AbbVie, for his contributions to the study, including analysis and interpretation of the data. Dr Earley was an employee of AbbVie during the study and may hold stock. Medical writing support was provided by Carol Brown, MS, of Prescott Medical Communications Group, Chicago, IL, and funded by AbbVie.
Additional Information: Data reported in this article are available within the article. Additional data from the NCT03739203 study may be requested at https://www.abbvieclinicaltrials.com/hcp/data-sharing/.
Supplementary Material: Available at Psychiatrist.com.
CLINICAL POINTS
- Many patients have incomplete response to standard antidepressant monotherapy for major depressive disorder (MDD); treatment with an adjunctive atypical antipsychotic is a viable option for these patients.
- In this MDD trial, no significant differences in efficacy were observed for cariprazine plus an ongoing antidepressant versus placebo.
- In 2 previous positive trials, adjunctive cariprazine was effective in reducing depressive symptoms in patients with MDD.
References (42)

- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. PubMed CrossRef
- Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. PubMed CrossRef
- Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–162. PubMed CrossRef
- Pigott HE, Leventhal AM, Alter GS, et al. Efficacy and effectiveness of antidepressants: current status of research. Psychother Psychosom. 2010;79(5):267–279. PubMed CrossRef
- Rush AJ. Limitations in efficacy of antidepressant monotherapy. J Clin Psychiatry. 2007;68(suppl 10):8–10. PubMed
- Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–1917. PubMed CrossRef
- Papakostas GI. Identifying patients with depression who require a change in treatment and implementing that change. J Clin Psychiatry. 2016;77(suppl 1):16–21. PubMed CrossRef
- Mrazek DA, Hornberger JC, Altar CA, et al. A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996-2013. Psychiatr Serv. 2014;65(8):977–987. PubMed CrossRef
- Mishra A, Sarangi SC, Maiti R, et al. Efficacy and safety of adjunctive serotonin-dopamine activity modulators in major depression: a meta-analysis of randomized controlled trials. J Clin Pharmacol. 2022;62(6):721–732. PubMed CrossRef
- Nelson JC, Papakostas GI. Atypical antipsychotic augmentation in major depressive disorder: a meta-analysis of placebo-controlled randomized trials. Am J Psychiatry. 2009;166(9):980–991. PubMed CrossRef
- Papakostas GI, Shelton RC, Smith J, et al. Augmentation of antidepressants with atypical antipsychotic medications for treatment-resistant major depressive disorder: a meta-analysis. J Clin Psychiatry. 2007;68(6):826–831. PubMed CrossRef
- Spielmans GI, Berman MI, Linardatos E, et al. Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes. Focus Am Psychiatr Publ. 2016;14(2):244–265. PubMed CrossRef
- Zhou X, Keitner GI, Qin B, et al. Atypical antipsychotic augmentation for treatment-resistant depression: a systematic review and network meta-analysis. Int J Neuropsychopharmacol. 2015;18(11):pyv060. PubMed CrossRef
- Duric V, Banasr M, Franklin T, et al. Cariprazine exhibits anxiolytic and dopamine D3 receptor-dependent antidepressant effects in the chronic stress model. Int J Neuropsychopharmacol. 2017;20(10):788–796. PubMed CrossRef
- Zimnisky R, Chang G, Gyertyán I, et al. Cariprazine, a dopamine D(3)-receptor-preferring partial agonist, blocks phencyclidine-induced impairments of working memory, attention set-shifting, and recognition memory in the mouse. Psychopharmacology (Berl). 2013;226(1):91–100. PubMed CrossRef
- Papp M, Gruca P, Lasoń-Tyburkiewicz M, et al. Attenuation of anhedonia by cariprazine in the chronic mild stress model of depression. Behav Pharmacol. 2014;25(5–6):567–574. PubMed CrossRef
- Durgam S, Earley W, Guo H, et al. Efficacy and safety of adjunctive cariprazine in inadequate responders to antidepressants: a randomized, double-blind, placebo-controlled study in adult patients with major depressive disorder. J Clin Psychiatry. 2016;77(3):371–378. PubMed CrossRef
- Sachs GS, Yeung PP, Rekeda L, et al. Adjunctive cariprazine for the treatment of patients with major depressive disorder: a randomized, double-blind, placebo-controlled phase 3 study. Am J Psychiatry. 2023;180(3):241–251. PubMed CrossRef
- Earley WR, Guo H, Németh G, et al. Cariprazine augmentation to antidepressant therapy in major depressive disorder: results of a randomized, double-blind, placebo-controlled trial. Psychopharmacol Bull. 2018;48(4):62–80. PubMed
- Fava M, Durgam S, Earley W, et al. Efficacy of adjunctive low-dose cariprazine in major depressive disorder: a randomized, double-blind, placebo-controlled trial. Int Clin Psychopharmacol. 2018;33(6):312–321. PubMed CrossRef
- APA. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
- First MB, Williams JBW, Karg RS, et al. Structured Clinical Interview for DSM-V, Clinical Trials Version (SCID-5-CT). New York, NY: Biometrics Research, New York State Psychiatric Institute; 2014.
- Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53(8):649–659. PubMed CrossRef
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. PubMed CrossRef
- Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133(5):429–435. PubMed CrossRef
- Desseilles M, Witte J, Chang TE, et al. Massachusetts General Hospital SAFER criteria for clinical trials and research. Harv Rev Psychiatry. 2013;21(5):269–274. PubMed CrossRef
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382–389. PubMed CrossRef
- Guy W. The Clinical Global Impression Severity and Improvement Scales. ECDEU Assessment Manual for Psychopharmacology. DHEW Publication No 76-338. Rockville, MD: US Department of Health, Education and Welfare publication (ADM); National Institute of Mental Health; 1976.
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. PubMed CrossRef
- Guy W. The Abnormal Involuntary Movement Scale. ECDEU Assessment Manual for Psychopharmacology. DHEW Publication No 76-338. Rockville, MD: National Institute of Mental Health.
- Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154(5):672–676. PubMed CrossRef
- Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand suppl. 1970;45(S212):11–19. PubMed CrossRef
- Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. PubMed CrossRef
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53(3):983–997. PubMed CrossRef
- Montgomery SA, Möller HJ. Is the significant superiority of escitalopram compared with other antidepressants clinically relevant? Int Clin Psychopharmacol. 2009;24(3):111–118. PubMed CrossRef
- Durgam S, Earley W, Lipschitz A, et al. An 8-week randomized, double-blind, placebo-controlled evaluation of the safety and efficacy of cariprazine in patients with bipolar I depression. Am J Psychiatry. 2016;173(3):271–281. PubMed CrossRef
- Earley W, Burgess MV, Rekeda L, et al. Cariprazine treatment of bipolar depression: a randomized double-blind placebo-controlled phase 3 study. Am J Psychiatry. 2019;176(6):439–448. PubMed CrossRef
- Earley WR, Burgess MV, Khan B, et al. Efficacy and safety of cariprazine in bipolar I depression: a double-blind, placebo-controlled phase 3 study. Bipolar Disord. 2020;22(4):372–384. PubMed CrossRef
- Vieta E, Earley WR, Burgess MV, et al. Long-term safety and tolerability of cariprazine as adjunctive therapy in major depressive disorder. Int Clin Psychopharmacol. 2019;34(2):76–83. PubMed CrossRef
- Earley W, Durgam S, Lu K, et al. Tolerability of cariprazine in the treatment of acute bipolar I mania: a pooled post hoc analysis of 3 phase II/III studies. J Affect Disord. 2017;215:205–212. PubMed CrossRef
- Earley W, Durgam S, Lu K, et al. Safety and tolerability of cariprazine in patients with acute exacerbation of schizophrenia: a pooled analysis of four phase II/III randomized, double-blind, placebo-controlled studies. Int Clin Psychopharmacol. 2017;32(6):319–328. PubMed CrossRef
- Earley WR, Burgess M, Rekeda L, et al. A pooled post hoc analysis evaluating the safety and tolerability of cariprazine in bipolar depression. J Affect Disord. 2020;263:386–395. PubMed CrossRef
This PDF is free for all visitors!
Save
Cite