Abstract
Schizophrenia is a major mental illness that is managed with long-term antipsychotic medication as a standard of care. Antipsychotic medications, however, are associated with many subjective and objective adverse effects. These adverse effects have driven the study of risk-mitigation strategies such as targeted intermittent therapy and dose reduction and drug discontinuation. Randomized controlled trials (RCTs) of these strategies have been synthesized in meta-analysis; both strategies have been associated with no functional benefits and with an increased risk of relapse. The RCTs, however, have been criticized because, in many, patients were abruptly switched to the target dose or too rapidly tapered, thereby predisposing the RCT to failure of the intervention. Two important RCTs examined gradual individualized dose reduction and discontinuation. One, conducted in first-episode psychosis patients who were free from positive symptoms for 6 months, found that, at 18-month follow-up, dose reduction was associated with a higher risk of relapse (number needed to harm [NNH] = 5) and with no functional benefits. However, after return to routine clinical care, at a 7-year follow-up, the dose reduction group had better functional outcomes and similar clinical outcomes relative to the maintenance treatment group. The other RCT, conducted in patients with relapsing psychosis, found that, at a 2-year follow-up, dose reduction was associated with a higher risk of relapse (NNH = 5) and with no improvements in social, cognitive, quality of life, satisfaction, and other domains. Many large nationwide observational studies have found that antipsychotic discontinuation by patients with first-episode psychosis and schizophrenia is associated with increased relapse, rehospitalization, suicide mortality, cardiovascular mortality, and all-cause mortality. There is also the ethical matter that attempts to identify the few who may benefit from antipsychotic dose reduction and discontinuation may compromise the health and stability of the many who require long-term maintenance treatment.
J Clin Psychiatry 2024;85(2):24f15363
Author affiliations are listed at the end of this article.
Schizophrenia is a major mental illness with risk factors that include vulnerability genes; exposures to antenatal, perinatal, postnatal, and early childhood brain insults; exposures to adversities during childhood; exposure to cannabis during adolescence; and others. Schizophrenia is characterized by widespread anatomical and neurohistological structural brain abnormalities, multisystem disturbances in neurochemical and neurohormonal signaling, functional alterations in brain circuits, neuroinflammation, changes in the gut-brain axis, and others. The clinical features of schizophrenia include delusions, hallucinations, thought disorder, mood disturbance, behavior disturbance, negative symptoms, cognitive impairment, social dysfunction, and others. The disorder is markedly heterogeneous, perhaps comprising a mixed group of syndromes, and is commonly studied along with other nonaffective psychotic disorders. The lifetime prevalence of schizophrenia is about 0.5%–1.0%, depending on how it is diagnosed and what population is surveyed.1,2
Treatment of Schizophrenia
Although schizophrenia may be characterized by neurodevelopmental features and by a prodrome of variable duration, it is the occurrence of a psychosis syndrome that defines the onset of the disorder as well as the occurrence of relapse in those who improve with treatment. Since 1952, the pharmacologic treatment of the psychosis syndrome of schizophrenia has invoked the use of dopamine D2 receptor blocking agents. These were initially neuroleptic drugs such as chlorpromazine and haloperidol, later atypical antipsychotic drugs such as risperidone and olanzapine, and more recently, third generation antipsychotic drugs such as aripiprazole and cariprazine.
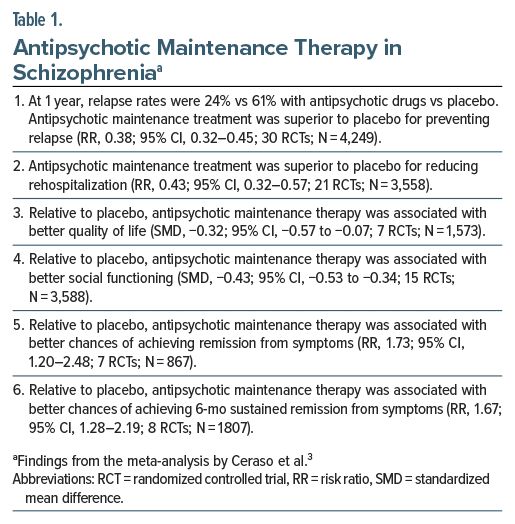
Schizophrenia patients who recover with antipsychotic drug treatment, as a standard of care, continue the treatment to guard against the risk of relapse into psychosis. In this regard, a Cochrane systematic review and meta-analysis of randomized controlled trials (RCTs)3 found that, in patients with schizophrenia, maintenance therapy with antipsychotic drugs was superior to maintenance therapy with placebo for preventing relapse at 1 year, reducing hospitalization rates, achieving remission from symptoms, achieving sustained remission from symptoms, improving quality of life, and improving social functioning (Table 1).
However, antipsychotic treatment, including maintenance antipsychotic treatment, is associated with well-known subjective and objective adverse effects. These may include a sense of being chemically straitjacketed and a decreased ability to experience pleasure, increased sleep and appetite, weight gain and components of the metabolic syndrome, early- and late-onset movement disorders, and many other common and uncommon conditions. Antipsychotic (especially neuroleptic) drugs may also increase the negative symptom and cognitive impairment burden that patients experience as part of their illness, potentially compromising quality of life and personal, social, and occupational functioning.3–6
Risk-Mitigation Strategies
Many indirect and direct risk-mitigation approaches have been suggested to reduce antipsychotic-related adverse effects and address unmet needs in schizophrenia.7 Among the direct approaches, since the late 1970s, 2 important treatment strategies have been examined. One is targeted intermittent therapy, and the other is antipsychotic drug dose reduction with or without drug discontinuation.8
Targeted intermittent therapy implicitly assumes that patients who recover from a psychotic episode enter a quiescent phase and therefore do not need to continue antipsychotic medications indefinitely. This approach involves tapering and withdrawing antipsychotic medication when the patient is stable, closely monitoring the patient during follow-up, and resuming treatment to prevent relapse if warning signs and symptoms suggest that relapse is imminent. Dose reduction strategies implicitly assume that patients require lower doses to remain well and be protected against relapse relative to the doses required to recover from psychosis; doses can be raised, again, if patients worsen. Proponents of both strategies expect that the risk of relapse (associated with the implementation of these strategies) will be low, that adverse consequences related to relapse will be low, and that periods of lower or no dosing will be associated with lower adverse effect burden, better quality of life, and better social, personal, and occupational functioning.
The rest of this article will examine how successful these strategies have been, with particular emphasis on 2 important dose reduction and drug discontinuation studies in the field.
Targeted Intermittent Therapy
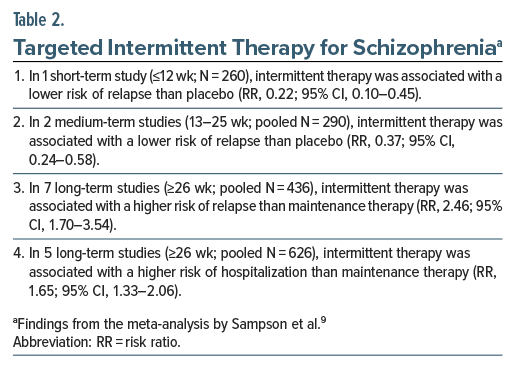
A Cochrane systematic review and meta-analysis of RCTs of targeted intermittent antipsychotic treatment for patients with schizophrenia identified 17 relevant studies with a pooled sample of 2,252 patients.9 Study sample sizes ranged from 29 to 375. Patients were followed for 6 weeks to 2 years. Important findings from the study are presented in Table 2. In summary, whereas short-term RCTs found that intermittent therapy, relative to placebo, protected against relapse, long-term RCTs found that intermittent therapy, relative to continuous therapy, was associated with higher risks of both relapse and hospitalization. The advantage of continuous over intermittent therapy was demonstrated in a later meta analysis, as well.10
Dose Reduction
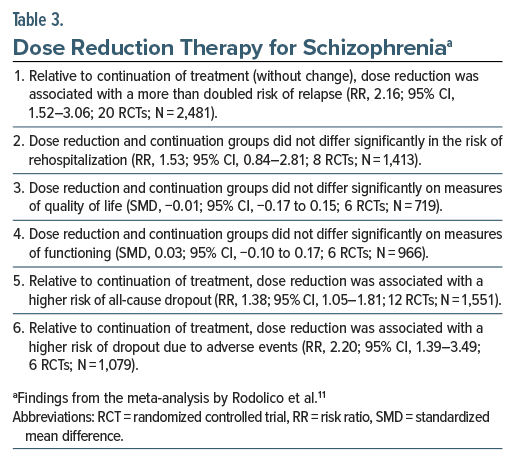
A Cochrane systematic review and meta-analysis of RCTs of antipsychotic dose reduction for patients with schizophrenia identified 22 relevant studies with a pooled sample of 2,635 patients.11 Study sample size ranged from 18 to 466 (median, 60), and study duration ranged from 12 weeks to 2 years (median, 37 weeks). Three studies planned drug discontinuation; the rest planned dose reduction (median, by 66%). About half of the studies abruptly switched patients to the target dose; the rest tapered the dose across 2–16 weeks. Patients in the studies were young (mean, 38.4 years).
Important findings from the meta-analysis are presented in Table 3. In summary, relative to continued treatment (without change), dose reduction was associated with an increased risk of relapse (but not rehospitalization) and an increased risk of all-cause dropout as well as dropout due to adverse events. Dose reduction was not associated with better quality of life or functioning, defeating the purpose of this dosing strategy.
Targeted Intermittent and Dose Reduction Strategies: Limitations of the Findings
On the surface, it would seem that the RCT data clearly favor maintenance antipsychotic therapy with unchanged dosing. However, critics argue that many of the RCTs were inherently biased against the targeted intermittent and dose reduction approaches because patients were either abruptly switched to the target dose or too rapidly tapered. Thus, relapse may have occurred because patients did not have sufficient time to biologically adapt to the medication changes. Instead, had dose taper been gradual to very gradual, there would have been ample opportunity to discover in which patients dose reduction was feasible and to what extent, and in which patients treatment discontinuation could be considered.
Separately, many studies did not have a follow-up that was sufficiently long for adequate evaluation of the strategies. Other limitations have also been described.12 In this context, the Netherlands and England studies by Wunderink et al13,14 and Moncrieff et al15 assume importance.
The Netherlands RCT: 18-Month Follow-Up
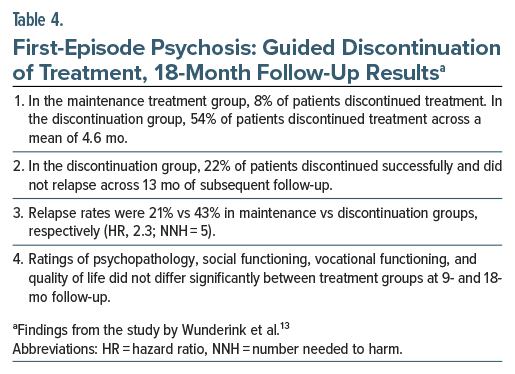
Wunderink et al13 described a 7-center RCT conducted on 131 young adults with first-episode psychosis (schizophrenia or related disorders), all of whom had been free from positive symptoms for at least 6 months. The mean age of the sample was 26 years. The sample was 70% male. These patients were randomized into maintenance treatment and guided discontinuation groups. Patients in the former group were maintained on a stable, low dose of (mostly) second-generation antipsychotic drugs. Patients in the latter group were very gradually tapered off their antipsychotic medication at a rate that depended on symptom severity and patient preference; if positive symptoms or warning signs of relapse emerged, medication could be resumed or dosing increased. Patients were followed for 18 months. Raters but not patients nor treating physicians were blinded to treatment strategy.
Important findings from the RCT13 are presented in Table 4. In summary, 22% of patients in the guided discontinuation group could stop treatment and remain well thereafter. However, overall, guided discontinuation was associated with a more than doubled risk of relapse across 18 months [number needed to harm (NNH) = 5] with no advantage for social functioning, vocational functioning, and quality of life. That is, at 18 months, guided discontinuation of antipsychotic medication in patients with first-episode psychosis was associated with evidence of risk but not of benefit.
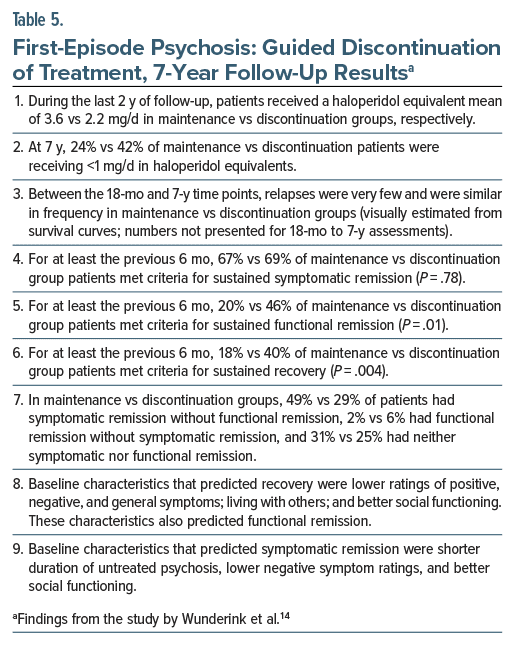
The Netherlands RCT: 7-Year Follow-Up
After the 18-month follow-up, patients were treated at the discretion of the clinical team. At 7 years, 103 patients were available for follow-up assessments. These patients were similar in key baseline characteristics to the patients who could not be reassessed. There were 51 and 52 patients in maintenance and discontinuation groups, respectively; the 2 groups were similar in key baseline characteristics.
Symptomatic remission was defined as a score of 3 (indicating “mild”) or lower during the past 6 months on all relevant items of the Positive and Negative Syndrome Scale. Functional remission was defined as a rating of minimal or no disability during the past 6 months in each of the 7 domains of the Groningen Social Disability Schedule (self-care, housekeeping, family relationships, partner relationships, relationships with peers, community integration, and vocational functioning). Recovery was defined as symptomatic and functional remission for at least the past 6 months. Ratings were made by unblinded assessors.
Important findings from the study14 are presented in Table 5. In summary, relative to patients in the maintenance group, patients in the discontinuation group used lower medication doses and, importantly, were more likely to meet the 6-month criteria for functional remission and recovery. The 2 groups did not differ in symptomatic remission and in relapse rates.
Comments on the Netherlands Study
The 7-year follow-up findings of Wunderink et al14 are counterintuitive and startling; they suggest that, in patients with first-episode psychosis who achieve 6 months of sustained symptomatic remission, as against continuing a stable dose of maintenance antipsychotic medication, it could be desirable to gradually taper and either maintain treatment with low doses of antipsychotic medication or withdraw treatment altogether. There are at least 3 important caveats here. One is that the findings need to be replicated with ratings obtained by blinded assessors. Another is that, as italicized above, the findings apply only to patients with first-episode psychosis who achieve 6 months of sustained symptomatic remission. A third is that the findings apply only to patients who have a higher level of functioning, are more adherent to therapy, and are easier to engage because these baseline characteristics distinguished eligible patients who consented to participate in the RCT vs those who did not.
A limitation of the guided antipsychotic discontinuation approach is that the 18-month relapse rates were doubled and that there were no 18-month functional advantages associated with the strategy.13 So, from an ethical perspective, it is debatable whether worsening 18-month clinical outcomes in some patients is an acceptable price to pay for improving 7-year functional outcomes in others. It must be remembered here that relapse is associated with indices of stress and distress in personal and family spaces, with potential for harm in personal, social, and vocational domains, and with risk of stepladder deterioration in the course of the illness.
On a sobering note, a nationwide, 20-year follow-up study of 8,719 first-episode schizophrenia patients found that discontinuation of antipsychotic medication anytime during follow-up was associated with an increased hazard of both rehospitalization and death.16 Of note, the prognosis for first-episode patients may not be as rosy as it appeared in the Netherlands study. For example, a systematic review and meta-analysis of 12 studies (pooled N = 11,958) found that the rate of treatment-resistant schizophrenia was 22.8% (95% CI, 19.1–27.0%) in first-episode psychosis cohorts.17 This whittles down the population for which guided discontinuation of treatment may be considered.
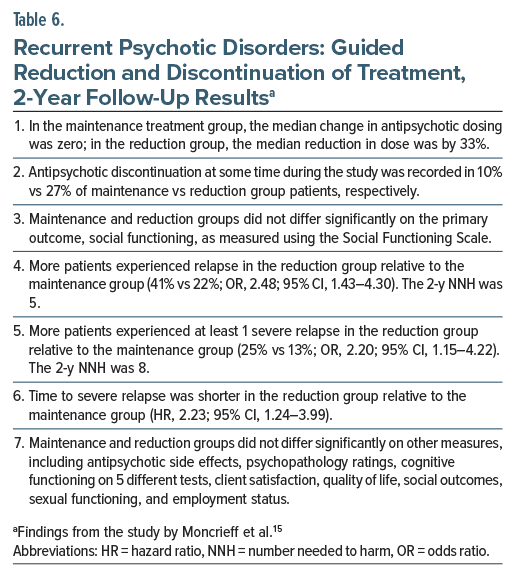
The England Study
In a large, 2-year RCT, Moncrieff et al15 recruited 253 adults with schizophrenia (69%) or other nonaffective psychotic disorder (31%) from 19 centers in England. All patients had had several previous episodes of illness (median, 3 previous hospitalizations). The mean age of the sample was 46 years. The sample was 66% male. Nearly 70% of the sample was white. Only 30% of the sample was employed. Nearly 70% of the patients had been in contact with mental health services for >10 years. The median antipsychotic dose at baseline was 300 mg/d in chlorpromazine equivalents.
These patients were randomized to continue on maintenance antipsychotic medication with minor modifications, if necessary, or to gradually taper and discontinue medication at individualized rates, across 12–18 months, based on shared decision-making; doses could be maintained or increased to manage emergent illness symptoms. Raters were blinded to treatment assignment, but patients and clinicians were not. Other pharmacologic and psychological treatments were permitted, as required. Ten patients dropped out in the maintenance group and 11 in the dose reduction group.
Important findings from the study15 are presented in Table 6. In summary, in patients with a history of repeatedly relapsing psychosis, individualized antipsychotic dose reduction and discontinuation was associated with a higher risk of relapse (NNH = 5) and serious relapse (NNH = 8) and with no benefits related to social functioning, cognitive functioning, occupational functioning, sexual functioning, quality of life, patient satisfaction, and antipsychotic adverse effect burden.
Comments on the England Study
As earlier observed, schizophrenia is a heterogeneous group of disorders, and it is possible that a small proportion of affected patients may recover completely and stay well with low doses of antipsychotic medication, or even with no antipsychotic medication. Others may do well despite varying periods off medication. As an example, in a small cohort of 139 young psychotic patients who were followed for 20 years in the Chicago Follow-up Study, about 30%–40% of patients at each of 6 follow-up occasions were observed to be off antipsychotic medication. These patients were less likely to have psychotic symptoms and more likely to experience recovery. However, it appeared that these patients were a self-selected subgroup with better prognostic characteristics, including better premorbid achievement, greater resilience, better cognition, and less anxiety.18 The Chicago Study numbers are probably optimistic; most patients with schizophrenia will require prolonged treatment with good medication adherence, perhaps best delivered with long-acting injectable antipsychotics.19
In this context, a matter of much importance is that antipsychotic discontinuation in patients with schizophrenia has consistently been associated with an increased risk of mortality. As an example, in a 20-year follow-up of a nationwide cohort of 62,250 patients with schizophrenia, the cumulative mortality rate was highest at 46% with no antipsychotic use, intermediate at 25% with any antipsychotic use, and lowest at 16% with clozapine use. Relative to nonuse, antipsychotic use was associated with lower suicide mortality (hazard ratio [HR], 0.52; 95% CI, 0.43–0.62), lower cardiovascular mortality (HR, 0.62; 95% CI, 0.57–0.67), and lower all-cause mortality (HR, 0.48; 95% CI, 0.46–0.51).20 Other studies have also found increased mortality in schizophrenia associated with nonuse of antipsychotic drugs.16,21,22
Parting Notes
Long-term maintenance medication is used in other major mental illnesses as well, including recurrent major depressive disorder and bipolar disorder. The antidepressants, mood stabilizers, atypical antipsychotics, and other medications used in these disorders are also associated with immediate- and delayed-onset adverse effects, some of which are potentially serious. Yet, it is schizophrenia that has been the predominant target of dose taper and drug discontinuation research. If we understand that the potential benefits of maintenance treatment outweigh the potential risks in recurrent major depressive disorder and bipolar disorder, it may be prudent to accept that the potential benefits outweigh the potential risks in schizophrenia, as well.
Considered from one angle, temporary functional gains associated with antipsychotic taper and discontinuation in schizophrenia should not be prioritized over the twin advantages of long-term clinical stability3,9,11 and lower risk of suicide, cardiovascular, and all-cause mortality16,20–22 associated with maintenance treatment. Considered from another angle, the health and stability of the majority should not be sacrificed at the altar of discovering the minority for whom lower dosing or no medication is feasible. It goes without saying, however, that all treatment decisions need to be based on a shared decision-making process. Finally, if taper and discontinuation are ever chosen, then a very gradual taper, across years, has been suggested, with fractional decreases as doses become lower.23
Article Information
Published Online: May 15, 2024. https://doi.org/10.4088/JCP.24f15363
© 2024 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Antipsychotic medication continuation vs taper and discontinuation in patients with schizophrenia and other nonaffective psychotic disorders.
J Clin Psychiatry. 2024;85(2):24f15363.
Author Affiliation: Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Financial disclosure and more about Dr Andrade.
References (23)

- Nasrallah HA. Re-inventing the schizophrenia syndrome: the elusive “theory of everything.” Schizophr Res. 2022;242:106–108. PubMed CrossRef
- Jauhar S, Johnstone M, McKenna PJ. Schizophrenia. Lancet. 2022;399(10323):473–486. PubMed CrossRef
- Ceraso A, Lin JJ, Schneider-Thoma J, et al. Maintenance treatment with antipsychotic drugs in schizophrenia: a Cochrane systematic review and meta analysis. Schizophr Bull. 2022;48(4):738–740. PubMed CrossRef
- Stroup TS, Gray N. Management of common adverse effects of antipsychotic medications. World Psychiatry. 2018;17(3):341–356. PubMed CrossRef
- Schneider-Thoma J, Chalkou K, Dörries C, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta analysis. Lancet. 2022;399(10327):824–836. PubMed CrossRef
- Sabé M, Pallis K, Solmi M, et al. Comparative effects of 11 antipsychotics on weight gain and metabolic function in patients with acute schizophrenia: a dose-response meta-analysis. J Clin Psychiatry. 2023;84(2):22r14490. PubMed
- Harvey PD, Kane JM. Addressing patients’ unmet needs to improve outcomes in schizophrenia. J Clin Psychiatry. 2021;82(3):IC20018AH3C. PubMed CrossRef
- Schooler NR. Maintenance medication for schizophrenia: strategies for dose reduction. Schizophr Bull. 1991;17(2):311–324. PubMed CrossRef
- Sampson S, Joshi K, Mansour M, et al. Intermittent drug techniques for schizophrenia. Schizophr Bull. 2013;39(5):960–961. PubMed CrossRef
- De Hert M, Sermon J, Geerts P, et al. The use of continuous treatment versus placebo or intermittent treatment strategies in stabilized patients with schizophrenia: a systematic review and meta-analysis of randomized controlled trials with first- and second-generation antipsychotics. CNS Drugs. 2015;29(8):637–658. PubMed CrossRef
- Rodolico A, Siafis S, Bighelli I, et al. Antipsychotic dose reduction compared to dose continuation for people with schizophrenia. Cochrane Database Syst Rev. 2022;11(11):CD014384. PubMed CrossRef
- Davidson M, Carpenter WT Jr. Targeted treatment of schizophrenia symptoms as they manifest, or continuous treatment to reduce the risk of psychosis recurrence. Schizophr Bull. 2024;50(1):14–21. PubMed
- Wunderink L, Nienhuis FJ, Sytema S, et al. Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry. 2007;68(5):654–661. PubMed CrossRef
- Wunderink L, Nieboer RM, Wiersma D, et al. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–920. PubMed CrossRef
- Moncrieff J, Crellin N, Stansfeld J, et al. Antipsychotic dose reduction and discontinuation versus maintenance treatment in people with schizophrenia and other recurrent psychotic disorders in England (the RADAR trial): an open, parallel-group, randomised controlled trial. Lancet Psychiatry. 2023;10(11):848–859. PubMed
- Tiihonen J, Tanskanen A, Taipale H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am J Psychiatry. 2018;175(8):765–773. PubMed CrossRef
- Siskind D, Orr S, Sinha S, et al. Rates of treatment-resistant schizophrenia from first-episode cohorts: systematic review and meta-analysis. Br J Psychiatry. 2022;220(3):115–120. PubMed CrossRef
- Harrow M, Jobe TH, Faull RN. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol Med. 2012;42(10):2145–2155. PubMed CrossRef
- Fang SC, Huang CY, Shao YHJ. Long-term outcomes of early use of long acting injectable antipsychotics in schizophrenia. J Clin Psychiatry. 2022;83(4):21r14153. PubMed CrossRef
- Taipale H, Tanskanen A, Mehtälä J, et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry. 2020;19(1):61–68. PubMed CrossRef
- Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr Res. 2018;197:274–280. PubMed CrossRef
- Strømme MF, Mellesdal LS, Bartz-Johannesen C, et al. Mortality and non-use of antipsychotic drugs after acute admission in schizophrenia: a prospective total cohort study. Schizophr Res. 2021;235:29–35. PubMed
- Horowitz MA, Murray RM, Taylor D. Tapering Antipsychotic Treatment.. JAMA Psychiatry. 2021;78(2):125–126. PubMed
This PDF is free for all visitors!
Save
Cite