Abstract
About 30%-50% of patients experience inadequate response to antidepressant therapy, and treatment choices for these patients include augmenting the antidepressant with another therapy, increasing the dose, switching to a different antidepressant, or combining antidepressants. Clinicians should tailor treatment strategies based on patients’ response, tolerability, and disease severity. In this activity, augmentation and adjunctive strategies involving atypical antipsychotics, as well as off-label options including buspirone, stimulants, thyroid hormone, and lithium, are reviewed.
This activity is the third of four included in the series “Inadequate Response to Antidepressant Treatment in Major Depressive Disorder”:
- Recognizing Inadequate Response in Patients With Major Depressive Disorder
- Implementing Measurement-Based Care to Determine and Treat Inadequate Response
- Overcoming Challenges to Treat Inadequate Response in Major Depressive Disorder
Financial support was provided by Otsuka Pharmaceutical Development & Commercialization, Inc., and Lundbeck, Inc.
Department of Psychiatry, Northwestern University, Feinberg School of Medicine, Chicago, Illinois (Dr Rafeyan); Massachusetts General Hospital Clinical Trials Network and Institute, Boston, Massachusetts (Dr Papakostas); Departments of Psychiatry and Family Medicine, University of Tennessee College of Medicine, Memphis, Tennessee (Dr Jackson); and University of Texas Southwestern Medical Center, Dallas, Texas (Dr Trivedi)
Financial disclosure
Dr Papakostas has been a consultant for AlphaSigma, Cala Health, Alkermes, Johnson & Johnson, and Otsuka and has received honoraria from Acadia, AlphaSigma, Alkermes, and Hypera S.A. Dr Jackson has been a consultant and speakers/advisory board member for and received honoraria from Allergan, Genentech, Otsuka, and Sunovion. Dr Rafeyan has received grant/research support from Eli Lilly, Sepracor, and Janssen and has been a speakers/advisory board member for AstraZeneca, Allergan, Alkermes, Eli Lilly, Janssen, Intra Cellular Therapies, Pfizer, Abbott, Otsuka, Lundbeck, Takeda, Teva, and Sunovion. Dr Trivedi has been a consultant or advisory board member for Allergan, Alto Neuroscience, Applied Clinical Intelligence, Axsome Therapeutics, Boehringer Ingelheim, Engage Health Media, GreenLight VitalSign6, Janssen, Lundbeck Research USA, Navitor, Otsuka, Perception Neuroscience, Pharmerit International, SAGE Therapeutics, and Signant Health; has received grant/research support from the National Institute of Mental Health, National Institute on Drug Abuse, Patient-Centered Outcomes Research Institute, and Cancer Prevention Research Institute of Texas; and has received editorial compensation from the American Psychiatric Association (Deputy Editor, American Journal of Psychiatry) and Oxford University Press.
This eReport is derived from the expert roundtable meeting “Inadequate Response to Antidepressant Treatment in Major Depressive Disorder,” which was held October 5, 2019.
This evidence-based peer-reviewed eReport was prepared by Healthcare Global Village, Inc. Financial support for preparation and dissemination of this eReport was provided by Otsuka Pharmaceutical Development & Commercialization, Inc., and Lundbeck, Inc., for educational purposes. The faculty acknowledges Evonne Krell for editorial assistance in developing the eReport. The opinions expressed herein are those of the faculty and do not necessarily reflect the views of Healthcare Global Village, Inc., the publisher, or the commercial supporters.
To cite: Rafeyan R, Papakostas GI, Jackson WC, et al. Inadequate response to treatment in major depressive disorder: augmentation and adjunctive strategies. J Clin Psychiatry. 2020;81(3):OT19037BR3.
To share: https://doi.org/10.4088/JCP.OT19037BR3
Meet the faculty
Introduction
At a roundtable meeting, an expert panel discussed how to determine where patients are on the response continuum and how to treat inadequate response. Their discussion is interspersed in video clips throughout this activity, which reviews the evidence on the available augmentation and adjunctive therapies in major depressive disorder (MDD).
Despite the number of effective treatments for MDD, about 30%–50% of patients experience inadequate response to antidepressant therapy, even when taken at an adequate dosage and for an adequate duration.1 Augmenting the antidepressant with another therapy is one treatment strategy for inadequate response and treatment-resistant depression (TRD); other strategies include increasing the antidepressant dose, switching to a different antidepressant, or combining antidepressants.1 Primary care clinicians may be more likely to switch agents, while mental health clinicians are more likely to augment or combine agents.2
Video 1. Dr Rafeyan Answers Why Clinicians Switch Antidepressants Before Considering Augmentation Strategies
Reference: Philip et al.3
Switching vs Augmenting
The decision to switch or augment an inadequate existing treatment can be difficult. Typically, switching to a new agent is appropriate if a patient has difficulty tolerating a medication or if an adequate dose and duration produce inadequate or no response. However, clinicians must be aware that patients who switch could be left with significant residual symptoms and impaired functioning throughout multiple treatment trials before remission is achieved. In these cases, augmentation therapy with an agent that has a different mechanism of action may be preferred to accelerate response to antidepressant therapy and alleviate troublesome residual symptoms.4 Augmentation strategies also appear to be more beneficial than switching within or between classes of antidepressants.3
Factors Involved in the Consideration of Adjunctive Treatment
The following sections of this report will review use of atypical antipsychotics as well as off-label options including buspirone, stimulants, thyroid hormone, and lithium. When reviewing the evidence on various augmentation options, trial design and sample size are important factors to keep in mind. Clinicians must also consider individual patients’ severity and duration of illness and previous treatment response when selecting an agent (AV 1).
AV 1. What Primary Factor Makes You Consider an Adjunctive Treatment in a Patient Presenting With Major Depressive Disorder Who Has Had an Adequate Trial of an Antidepressant (AD) But Is Still Experiencing Depressive Symptoms?
Data expressed as percentages of respondents.
Video 2. The Panel Reviews the Poll Question Results on Factors Involved in the Consideration of Adjunctive Treatment
References: Kurian et al,4 Nemeroff,5 Jackson and Endow-Eyer.6
Buspirone
Buspirone. The addition of buspirone to a selective serotonin reuptake inhibitor (SSRI) may result in an enhanced serotonergic effect and improvement of depressive symptoms, as was the case in SSRI nonresponders in the Sequenced Treatment Alternatives to Relieve Depression trial.2 In a review,1 2 double-blind randomized controlled trials (RCTs) of buspirone augmentation were identified. Landen and colleagues7 studied 117 patients with MDD who had no improvement (based on Clinical Global Impression–Improvement scale [CGI-I] rating of worse/no improvement) after at least 4 weeks’ prior SSRI treatment (citalopram 40 mg/d or paroxetine 30 mg/d). In the 4 weeks of augmentation with buspirone (10–60 mg/d) or placebo, the difference in response rates was not statistically significant (50.9% vs 46.7%, respectively), possibly due to the unusually high response rate.7 The second RCT8 studied patients who had not responded to SSRI treatment (N=102) of at least 6 weeks. Patients were augmented with either buspirone (10–30 mg/d) or placebo for 6 weeks, and the treatment groups did not show statistically significant differences in mean change from baseline in Montgomery-Asberg Depression Rating Scale (MADRS) total score and response rate.
Methylphenidate and Modafinil
Methylphenidate. For methylphenidate augmentation, 2 studies failed to show statistically significant improvement over placebo.1 A study9 of patients (N=30) who had failed more than 1 antidepressant after more than 6 weeks of therapy found that 40% of the patients treated with methylphenidate XR (18–54 mg/d) augmentation achieved a response compared with 23.3% of the patients treated with placebo augmentation, which was not a statistically significant difference. Similarly, another study10 of methylphenidate augmentation versus placebo reported that there was no statistical difference in the change from baseline in the MADRS score between the 2 groups (p=.74).
Modafinil. Modafinil is a stimulant indicated for improving wakefulness in individuals with narcolepsy, obstructive sleep apnea, and shift work sleep disorder. It has been studied as an adjunct to antidepressants and has less misuse potential than methylphenidate. While some early studies did not demonstrate efficacy of modafinil augmentation compared with placebo, other trials have found decreased depression and fatigue and improved cognition in patients receiving modafinil augmentation.11 Further, a pooled analysis12 found that modafinil augmentation rapidly (within 1 week) and significantly improved overall clinical condition (CGI-I), depressive symptoms (17-item Hamilton Depression Rating Scale), wakefulness, and fatigue (p<.01 for all) compared with placebo. These improvements combined with its tolerability make modafinil a useful adjunctive treatment option, especially for patients experiencing excessive sleepiness and fatigue.
Lithium and Thyroid Hormone
Lithium and thyroid hormone are sometimes used on an off-label basis and are 2 of the most studied augmentation strategies in depression, but much of the data come from studies with tricyclic antidepressants (TCAs) rather than SSRIs or serotonin-norepinephrine reuptake inhibitors (SNRIs).3
Thyroid hormone. Thyroid hormone, triiodothyronine (T3) and occasionally thyroxine (T4), is a commonly used augmentation strategy due to its favorable tolerability and side effect profile.3 Meta-analyses of multiple studies, mostly poorly designed and underpowered, have found the use of T3 augmentation to be associated with a significant increase in the likelihood of response and in the speed of response to antidepressants. Only a small subsample of these patients met criteria for TRD.5 A study by Joffe and colleagues13 analyzed lithium, liothyronine, and placebo augmentation in patients who had previously failed to respond to 5 weeks of TCA therapy. For the liothyronine group, 59% (10/17) of patients responded to treatment as compared to 19% (3/16) of patients in the placebo group (p=.018).
Lithium. Lithium augmentation is another well-studied intervention in MDD, but the results are not conclusive. One review1 included 6 relatively small studies evaluating augmentation with lithium. Study samples ranged from 34 to 62 randomized patients, and the double-blind phases with augmentation ranged from 7 days to 9 weeks. Half of the studies showed positive results for lithium augmentation, while the remaining studies did not find significant differences from placebo.
A recent meta-analysis14 including 10 RCTs showed a statistically significant effect on the response rate of lithium augmentation versus placebo with an odds ratio of 3.11, but 5 of the pooled studies did not show a significant difference between lithium augmentation and placebo. The lithium augmentation group had a mean response rate of 41.2% compared to 14.4% in the placebo group.
It has been suggested that lithium has anti-suicide properties, but the evidence for this is limited, being based on just a few studies in unipolar depression.6 One review15 of lithium’s effect in patients with unipolar, bipolar, and schizoaffective disorder reported that lithium was more effective than placebo in reducing the number of suicides and deaths from any cause but showed less clear benefits in preventing deliberate self-harm versus placebo. Limitations of this review include small study sample sizes and few overall suicide and deliberate self-harm events.
Atypical Antipsychotics
Augmentation with atypical antipsychotics to improve antidepressant response has received considerable attention in the last few years, as these agents act on a wide range of receptor targets.3 Aripiprazole was the first second-generation antipsychotic (SGA) to receive US Food and Drug Administration (FDA) approval as an augmentation agent for the treatment of MDD, followed by quetiapine XR and the olanzapine plus fluoxetine combination (OFC). In July 2015, brexpiprazole also received FDA approval for the treatment of MDD as an augmentation to antidepressant treatment.16 Other SGAs have had mixed results in MDD and remain off-label for use as augmenting agents to antidepressant treatment (AV 2).16
AV 2. Levels of Evidence for Atypical Antipsychotics Used in MDD
Data from Wang et al.16
Aripiprazole. Aripiprazole has demonstrated clinical benefits in numerous open label and randomized controlled trial studies.16 A review1 of 3 double-blind randomized trials of low-dose aripiprazole (2–20 mg) augmentation of antidepressants (SSRIs or SNRI) showed consistent results of significant increases in response rate versus placebo (Study 117: 33.7% vs 23.8%, p=.027; Study 218: 32.4% vs 17.4%, p<.001; and Study 319: 46.6% vs 26.6%, p<.001).
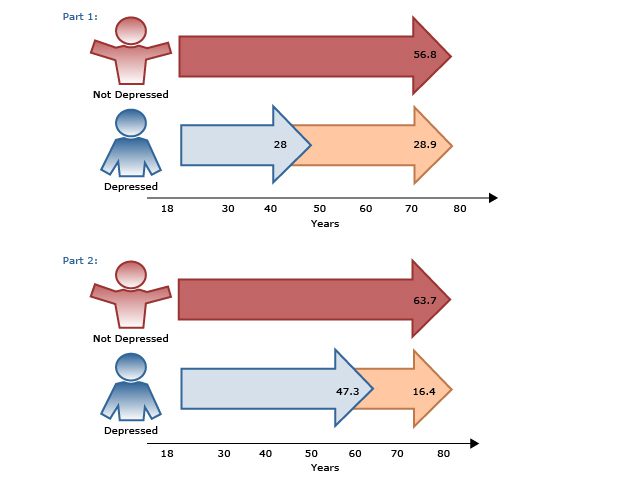
A study20 comparing aripiprazole augmentation versus antidepressant switching found that augmentation was the more beneficial next step in patients with inadequate response to initial antidepressant treatment for at least 6 weeks; tolerability was comparable between the 2 strategies. Another study21 in patients with MDD who were unresponsive to at least 1 antidepressant of adequate dose and duration compared 3 interventions: (1) switch to bupropion, (2) augment current treatment with bupropion, and (3) augment with aripiprazole. At 12 weeks, remission rates were highest for the augment-aripiprazole group (n=146) at 28.9% compared to the switch group (n=114) and augment-bupropion group (n=136) (22.3% and 26.9%, respectively). Response was also greater for the augment-aripiprazole group (74.3%) than for the switch (62.4%) or augment-bupropion (65.6%) groups.
Quetiapine. Quetiapine has been studied both as an augmentation to antidepressants and as monotherapy in MDD, and it received FDA approval as adjunctive therapy to antidepressants in 2009. In terms of augmentation therapy, 6 quetiapine augmentation RCTs were conducted for the treatment of MDD,16 with only 1 failing to show superior efficacy over placebo, and the quetiapine dosages used in that study were lower than the others (mean dose: 47 mg/d). In 1 of the studies, quetiapine plus cognitive-behavioral therapy (CBT) demonstrated a significant reduction in primary efficacy measures compared with CBT and placebo.22
One review1 of 3 studies of quetiapine augmentation to antidepressants included 2 multicenter 6-week trials and 1 smaller (N=36) 8-week study. Both of the 6-week trials showed an increase in response rates for quetiapine augmentation compared with placebo, and the smaller study found a statistically significant improved response in the quetiapine (200–400 mg/d) group versus placebo (67% vs 27%; p=.015) in patients who had failed treatment with an SSRI or SNRI.
Olanzapine. The OFC has been evaluated for TRD in 2 positive and 3 negative controlled trials.3 OFC was no more effective than fluoxetine or olanzapine monotherapy in 2 of the negative trials. In the third, it was no more effective than fluoxetine or venlafaxine but superior to olanzapine monotherapy.3
A positive effect for OFC was shown in an 8-week randomized, double-blind trial by Shelton et al23 in which olanzapine was titrated weekly (between 4–20 mg/d) based on response and tolerability in 28 patients with TRD. One of 2 studies by Thase and colleagues24 showed a statistically significant difference in the OFC group compared to fluoxetine and olanzapine monotherapies (p=.039 and p<.001, respectively) in patients with MDD who had experienced nonresponse to at least 1 antidepressant trial. Response rates were 44.3% for the OFC group compared to 29.7% and 16.7% in the fluoxetine and olanzapine monotherapy groups.24
In a study by Brunner and colleagues25 that evaluated relapse prevention in TRD patients, OFC was compared with fluoxetine monotherapy in patients who failed to show a satisfactory response to >2 different antidepressants for >6 weeks. The relapse time was significantly longer in the OFC group than in the fluoxetine group (p<.001). Relapse rates were also lower for OFC than fluoxetine (15.8% vs 31.8%, p<.001). However, more patients in the OFC group experienced clinically significant (>7%) weight gain (11.8%) than those taking fluoxetine alone (2.3%; p<.001).25
Brexpiprazole. Brexpiprazole, the most recent SGA to receive FDA approval as adjunctive therapy in MDD, is a dopamine D2 receptor partial agonist. Numerous studies investigating brexpiprazole in the treatment of depression have been completed and are still ongoing.16 A pooled analysis26 of 4 studies of adjunctive brexpiprazole (1–3 mg/d) versus placebo in outpatients with MDD and inadequate response to antidepressants (N=1,853) showed greater improvement in MADRS total score for adjunctive brexpiprazole (2–3 mg/d) than placebo (p<.0001).
Meta-analyses confirm that augmenting antidepressants with atypical antipsychotics is more effective than placebo for response (57% vs 35% pooled response rate)27 and remission (odds ratio 2.00).28 It must be noted, however, that atypical antipsychotic augmentation was also associated with higher withdrawals due to adverse events.1 Side effects for these medications include weight gain and metabolic syndrome (with olanzapine and quetiapine) and neuromotor side effects (eg, akathisia [aripiprazole] extrapyramidal symptoms [EPS], tardive dyskinesia).3 The risks and benefits of these agents must be communicated to patients so they understand how they can help and what adverse effects to watch for.
 Patient Perspectives
Patient Perspectives
In interviews conducted by the Depression and Bipolar Support Alliance (oral communication, December 2019), two patients explained that side effects are an important factor in their willingness to try adjunctive therapy:
“It would strongly depend on side effects and how bad I was doing at the time.”
“I tend to read the medication first and try to understand it and see what the side effects are and also compare it to the current medications I’m taking. If I feel the side effects are too strong, or they’re going to cause something that I don’t want to deal with, then I won’t be willing to try it out. If the side effects are not as bad, and I feel that it’ll probably work together with what I’m currently taking, and that I’ll be able to finish it, then of course I’ll be willing to give it a try.”
Video 3. Drs Rafeyan and Jackson Talk About Educating Patients on the Benefits and Risks Associated With Atypical Antipsychotics
Conclusion
The strategies for addressing inadequate response in MDD include switching antidepressants, combining antidepressants, optimizing the dose, and augmenting the current antidepressant. In many cases, augmentation strategies can accelerate response to antidepressant therapy and alleviate troublesome symptoms faster than several different antidepressant monotherapy trials. The results of trials with augmentation of antidepressants with off-label buspirone and methylphenidate do not show statistical significance, but modafinil may help patients experiencing sleepiness or fatigue. Positive placebo-controlled studies of lithium and thyroid augmentation, mostly with TCAs, were identified, although results are inconsistent. Atypical antipsychotics show significantly higher response rates compared to an antidepressant alone, and early augmentation can have a significant effect on symptoms and improvement. Patients should receive education on the benefits and risks associated with adjunctive atypical antipsychotics to improve their adherence to an additional medication.
 Clinical Points
Clinical Points
- Tailor treatment strategies to augment, combine, or switch medications based on patients’ response, tolerability, and disease severity.
- Consider augmentation strategies early in patients experiencing partial or no response to antidepressant treatment.
- Educate patients on the benefits and risks of atypical antipsychotic medications.
© Copyright 2020 Physicians Postgraduate Press, Inc.
References (28)

- Fleurence R, Williamson R, Jing Y, et al. A systematic review of augmentation strategies for patients with major depressive disorder. Psychopharmacol Bull. 2009;42(3):57–90. PubMed
- Barowsky J, Schwartz TL. An evidence-based approach to augmentation and combination strategies for treatment-resistant depression. Psychiatry (Edgmont). 2006;3(7):42–61. PubMed
- Philip NS, Carpenter LL, Tyrka AR, et al. Pharmacologic approaches to treatment resistant depression: a re-examination for the modern era. Expert Opin Pharmacother. 2010;11(5):709–722. PubMed CrossRef
- Kurian BT, Greer TL, Trivedi MH. Strategies to enhance the therapeutic efficacy of antidepressants: targeting residual symptoms. Expert Rev Neurother. 2009;9(7):975–984. PubMed CrossRef
- Nemeroff CB. Prevalence and management of treatment-resistant depression. J Clin Psychiatry. 2007;68(suppl 8):17–25. Pubmed
- Jackson E, Endow-Eyer RA. A review of the evidence supporting the use of lithium augmentation therapy for the reduction of suicidal behavior in patients with unipolar depression: revisiting an overlooked benefit of an older medication. Ment Health Clin. 2014;4(5):221–225. CrossRef
- Landén M, Björling G, Agren H, et al. A randomized, double-blind, placebo-controlled trial of buspirone in combination with an SSRI in patients with treatment-refractory depression. J Clin Psychiatry. 1998;59(12):664–668. Pubmed CrossRef
- Appelberg BG, Syvälahti EK, Koskinen TE, et al. Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study. J Clin Psychiatry. 2001;62(6):448–452. Pubmed CrossRef
- Patkar AA, Masand PS, Pae C-U, et al. A randomized, double-blind, placebo-controlled trial of augmentation with an extended release formulation of methylphenidate in outpatients with treatment-resistant depression. J Clin Psychopharmacol. 2006;26(6):653–656. Pubmed CrossRef
- Ravindran AV, Kennedy SH, O’Donovan MC, et al. Osmotic-release oral system methylphenidate augmentation of antidepressant monotherapy in major depressive disorder: results of a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2008;69(1):87–94. Pubmed
- Pary R, Scarff JR, Jijakli A, et al. A review of psychostimulants for adults with depression. Fed Pract. 2015;32(suppl 3):30S–37S. Pubmed
- Fava M, Thase ME, DeBattista C, et al. Modafinil augmentation of selective serotonin reuptake inhibitor therapy in MDD partial responders with persistent fatigue and sleepiness. Ann Clin Psychiatry. 2007;19(3):153–159. Pubmed CrossRef
- Joffe RT, Singer W, Levitt AJ, et al. A placebo-controlled comparison of lithium and triiodothyronine augmentation of tricyclic antidepressants in unipolar refractory depression. Arch Gen Psychiatry. 1993;50(5):387–393. Pubmed CrossRef
- Bauer M, Adli M, Bschor T, et al. Lithium’s emerging role in the treatment of refractory major depressive episodes: augmentation of antidepressants. Neuropsychobiology. 2010;62(1):36–42. Pubmed CrossRef
- Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346(jun27 4):f3646–f3646. Pubmed CrossRef
- Wang S-M, Han C, Lee S-J, et al. Second generation antipsychotics in the treatment of major depressive disorder: an update. Chonnam Med J. 2016;52(3):159–172. Pubmed CrossRef
- Berman RM, Marcus RN, Swanink R, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2007;68(6):843–853. Pubmed CrossRef
- Marcus RN, McQuade RD, Carson WH, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28(2):156–165. Pubmed CrossRef
- Berman RM, Fava M, Thase ME, et al. Aripiprazole augmentation in major depressive disorder: a double-blind, placebo-controlled study in patients with inadequate response to antidepressants. CNS Spectr. 2009;14(4):197–206. Pubmed CrossRef
- Han C, Wang S-M, Kwak K-P, et al. Aripiprazole augmentation versus antidepressant switching for patients with major depressive disorder: A 6-week, randomized, rater-blinded, prospective study. J Psychiatr Res. 2015;66-67:84–94. Pubmed CrossRef
- Mohamed S, Johnson GR, Chen P, et al; and the VAST-D Investigators. Effect of antidepressant switching vs augmentation on remission among patients with major depressive disorder unresponsive to antidepressant treatment: the VAST-D randomized clinical trial. JAMA. 2017;318(2):132–145. Pubmed CrossRef
- Chaput Y, Magnan A, Gendron A. The co-administration of quetiapine or placebo to cognitive-behavior therapy in treatment refractory depression: a preliminary trial. BMC Psychiatry. 2008;8(1):73. Pubmed CrossRef
- Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158(1):131–134. Pubmed CrossRef
- Thase ME, Corya SA, Osuntokun O, et al. A randomized, double-blind comparison of olanzapine/fluoxetine combination, olanzapine, and fluoxetine in treatment-resistant major depressive disorder. J Clin Psychiatry. 2007;68(2):224–236. Pubmed CrossRef
- Brunner E, Tohen M, Osuntokun O, et al. Efficacy and safety of olanzapine/fluoxetine combination vs fluoxetine monotherapy following successful combination therapy of treatment-resistant major depressive disorder. Neuropsychopharmacology. 2014;39(11):2549–2559. Pubmed CrossRef
- Thase ME, Zhang P, Weiss C, et al. Efficacy and safety of brexpiprazole as adjunctive treatment in major depressive disorder: overview of four short-term studies. Expert Opin Pharmacother. 2019;20(15):1907–1916. Pubmed CrossRef
- Papakostas GI, Shelton RC, Smith J, Fava M. Augmentation of antidepressants with atypical antipsychotic medications for treatment-resistant major depressive disorder: a meta-analysis. J Clin Psychiatry. 2007;68(6):826–831. Pubmed CrossRef
- Nelson JC, Papakostas GI. Atypical antipsychotic augmentation in major depressive disorder: a meta-analysis of placebo-controlled randomized trials. Am J Psychiatry. 2009;166(9):980–991. Pubmed CrossRef
Save
Cite