ABSTRACT
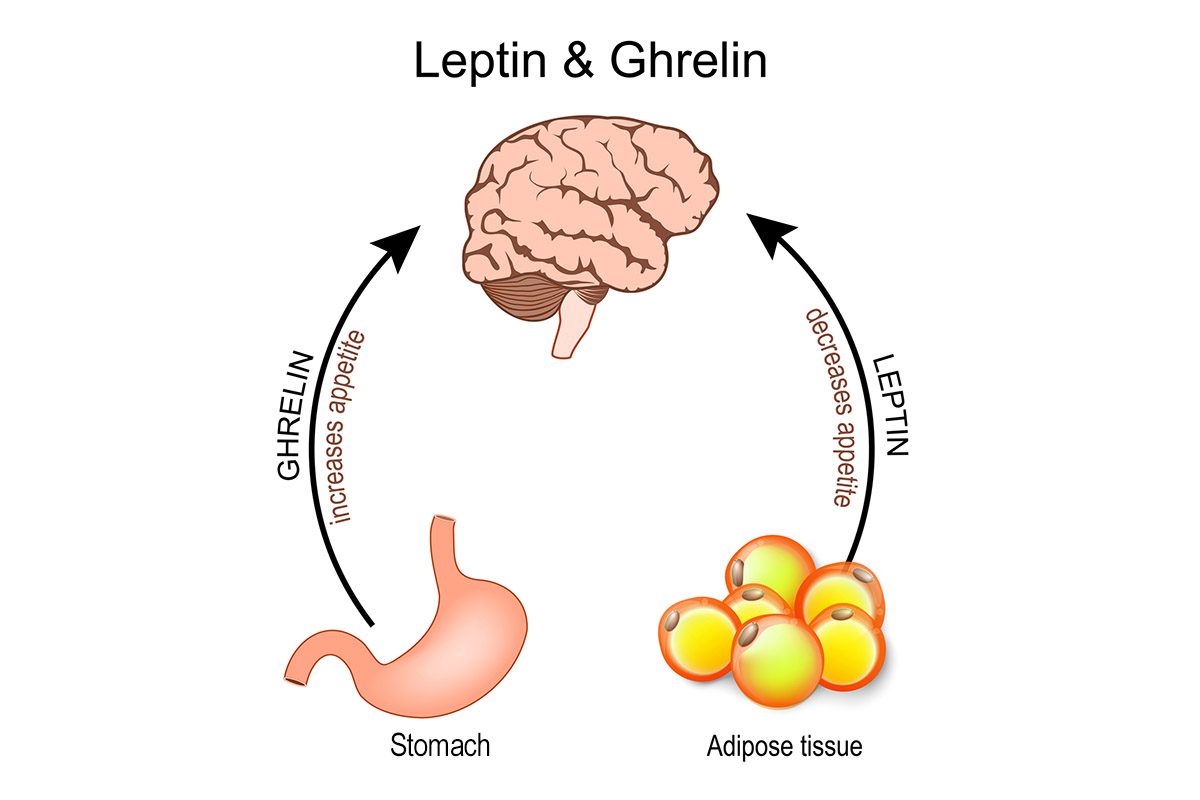
Objective: Avoidant/restrictive food intake disorder (ARFID) is characterized by food avoidance or dietary restriction not primarily motivated by body weight/shape concerns. Individuals with ARFID can report early satiation, post-prandial fullness, and high intermeal satiety, but whether these symptoms are related to differences in the biology underlying appetite regulation is unknown. In male and female children and adolescents, we hypothesized that fasting levels of cholecystokinin (CCK), a satiety hormone, would be elevated in participants with ARFID (full or subthreshold) versus healthy controls (HCs). Within the ARFID group, we also explored the relations of CCK with weight status, subjective appetite ratings, and ARFID severity and phenotypes.
Methods: A total of 125 participants (83 with full/subthreshold ARFID (per DSM-5) and 42 HCs, aged 10.2–23.7 years; 61% female; July 2014–December 2019) underwent fasting blood draws for CCK, completed self-report measures assessing subjective state and trait appetite ratings, and completed a semistructured interview assessing ARFID severity.
Results: Fasting CCK was higher in those with full/subthreshold ARFID versus HCs with a large effect (F1 = 25.0, P < .001, ηp2 = 0.17), controlling for age, sex, and body mass index (BMI) percentile. Within the ARFID group, CCK was not significantly related to BMI percentile, subjective appetite ratings, or ARFID characteristic measures.
Conclusions: CCK may contribute to etiology and/or maintenance of ARFID, as children and adolescents with heterogeneous presentations of avoidant/restrictive eating appear to show elevated fasting levels compared to healthy youth. Further research is needed to understand relations between CCK and appetite, weight, and eating behavior in ARFID.
Continue Reading...
Members enjoy unlimited free PDF downloads as part of their subscription! Subscribe today for instant access to this article and our entire library in your preferred format. Alternatively, you can purchase the PDF of this article individually.
References (22)

- Thomas JJ, Lawson EA, Micali N, et al. Avoidant/restrictive food intake disorder: a three-dimensional model of neurobiology with implications for etiology and treatment. Curr Psychiatry Rep. 2017;19(8):54. PubMed CrossRef
- Schorr M, Miller KK. The endocrine manifestations of anorexia nervosa: mechanisms and management. Nat Rev Endocrinol. 2017;13(3):174–186. PubMed CrossRef
- Bailer UF, Kaye WH. A review of neuropeptide and neuroendocrine dysregulation in anorexia and bulimia nervosa. Curr Drug Targets CNS Neurol Disord. 2003;2(1):53–59. PubMed CrossRef
- Woods SC, May-Zhang AA, Begg DP. How and why do gastrointestinal peptides influence food intake? Physiol Behav. 2018;193(Pt B):218–222. PubMed CrossRef
- Kaye WH, Wierenga CE, Bailer UF, et al. Nothing tastes as good as skinny feels: the neurobiology of anorexia nervosa. Trends Neurosci. 2013;36(2):110–120. PubMed CrossRef
- Becker KR, Mancuso C, Dreier MJ, et al. Ghrelin and PYY in low-weight females with avoidant/restrictive food intake disorder compared to anorexia nervosa and healthy controls. Psychoneuroendocrinology. 2021;129:105243. PubMed CrossRef
- Harshman SG, Jo J, Kuhnle M, et al. A moving target: how we define avoidant/restrictive food intake disorder can double its prevalence. J Clin Psychiatry. 2021;82(5):20m13831. PubMed CrossRef
- Sysko R, Glasofer DR, Hildebrandt T, et al. The eating disorder assessment for DSM-5 (EDA-5): development and validation of a structured interview for feeding and eating disorders. Int J Eat Disord. 2015;48(5):452–463. PubMed CrossRef
- Kaufman J, Birmaher B, Axelson D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children. KSADS-PL; 2013.
- Fairburn CG, Beglin SJ. Eating Disorder Examination Questionnaire (6.0). In: Fairburn CG, ed. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008.
- Bryant-Waugh R, Micali N, Cooke L, et al. Development of the Pica, ARFID, and Rumination Disorder Interview, a multi-informant, semi-structured interview of feeding disorders across the lifespan: a pilot study for ages 10-22. Int J Eat Disord. 2019;52(4):378–387. PubMed CrossRef
- Ackerman KE, Slusarz K, Guereca G, et al. Higher ghrelin and lower leptin secretion are associated with lower LH secretion in young amenorrheic athletes compared with eumenorrheic athletes and controls. Am J Physiol Endocrinol Metab. 2012;302(7):E800–E806. PubMed CrossRef
- Hunot C, Fildes A, Croker H, et al. Appetitive traits and relationships with BMI in adults: development of the Adult Eating Behaviour Questionnaire. Appetite. 2016;105:356–363. PubMed CrossRef
- Murray HB, Bailey AP, Keshishian AC, et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995–2002.e1. PubMed
- Burton Murray H, Jehangir A, Silvernale CJ, et al. Avoidant/restrictive food intake disorder symptoms are frequent in patients presenting for symptoms of gastroparesis. Neurogastroenterol Motil. 2020;32(12):e13931. PubMed CrossRef
- Pilichiewicz AN, Feltrin KL, Horowitz M, et al. Functional dyspepsia is associated with a greater symptomatic response to fat but not carbohydrate, increased fasting and postprandial CCK, and diminished PYY. Am J Gastroenterol. 2008;103(10):2613–2623. PubMed CrossRef
- Culbert KM, Racine SE, Klump KL. Hormonal factors and disturbances in eating disorders. Curr Psychiatry Rep. 2016;18(7):65. PubMed CrossRef
- Van den Houte K, Scarpellini E, Verbeure W, et al. The role of GI peptides in functional dyspepsia and gastroparesis: a systematic review. Front Psychiatry. 2020;11:172. PubMed CrossRef
- Crow S. Investigational drugs for eating disorders. Expert Opin Investig Drugs. 1997;6(4):427–436. PubMed CrossRef
- Lutter M. Emerging treatments in eating disorders. Neurotherapeutics. 2017;14(3):614–622. PubMed CrossRef
- Khalsa SS, Adolphs R, Cameron OG, et al; Interoception Summit 2016 participants. Interoception and mental health: a roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(6):501–513. PubMed
- Thomas JJ, Eddy K. Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder: Children, Adolescents, and Adults. Cambridge, UK: Cambridge University Press; 2019.
Please sign in or purchase this PDF for $40.
Save
Cite
Already a member? Login