Information in this Academic Highlights section of The Journal of Clinical Psychiatry was presented at the panel discussion “Racial and Ethnic Disparities in Mental Health and Clinical Trials: What Can Be Done to Enhance Diversity and Eliminate Disparities?” held on June 1, 2022, at the American Society of Clinical Psychopharmacology Annual Meeting in Scottsdale, Arizona. The panelists were Inez Ruiz-White, PhD; John Kraus, MD; Luke Kramer, BA; Lionel Philips, MBA; and Francisco Moreno, MD.
J Clin Psychiatry 2023;84(4):23ah14887
Author affiliations are listed at the end of this article.
Historically, in the United States, scientific racism has been used to justify differential treatment of Black, Indigenous, People of Color (BIPOC) populations compared with the White population.1–4 Discrimination toward BIPOC populations by the medical community5,6 has contributed to racial and ethnic disparities in health care that persist to this day.6
At the 2022 American Society of Clinical Psychopharmacology Annual Meeting, a panel of 5 experts from the areas of academia, advocacy, and clinical research discussed racial and ethnic disparities in mental health care. This Academic Highlights summarizes and expands on that discussion by tracing the history of scientific racism from the colonization of the US to present-day health inequities, illustrating the ongoing problem of low diversity in clinical trials, and outlining solutions through community engagement.
Although the references we reviewed used a variety of different terms to describe races and ethnicities, for consistency we chose the following: American Indian/Alaska Native (AI/AN), Asian, Black, Hispanic/Latino (H/L), and White. We acknowledge that there are many terms in use related to race and ethnicity but have adhered to the US Census Bureau terminology where possible. In a few instances the terminology was adjusted based on the reference, such as using “Native American” rather than AI/AN regarding land seizure by colonizers before Alaska became part of the US.
ROOTS OF RACIAL AND ETHNIC DISPARITIES: HISTORIC INEQUITIES
US Colonialism and Slavery
The US was ostensibly founded on principles of equality and liberty, yet inequities in physical and mental health care for BIPOC populations compared with the White population are embedded in the fabric of the nation.5,6 The social construct of race was used to justify the White European colonization of the Americas and the Atlantic slave trade in the 16th century.7–12 More than 12 million African people were enslaved, with approximately 33% dying during the forced transit to the West and another 10%–30% dying in their first 3 years in slavery due to harsh living conditions and lack of medical care.5,13,14 On US plantations, enslaved Africans endured malnourishment, forced labor, family separation, physical punishment, rape, excessive salt loss from sweating and diarrheal diseases, suicide, inferior medical treatment, and medical experimentation.6,13–16 Simultaneously, 2.5 to 5 million Native Americans were enslaved in the Americas in what historian Andrés Reséndez describes as a “parallel system of bondage as degrading and vast as African slavery.”17(p1)
Racism was enshrined in the US Constitution in 1788 with the “Three-Fifths Clause,” which determined a state’s congressional representation by counting White people each as a whole person, counting enslaved Black people as three-fifths of a person, and not counting Native Americans at all.18 The US also enacted the Indian Civilization Act of 1819, which began 150 years of forcing Native children from their homes and systematically suppressing their culture in residential facilities where widespread abuse occurred.19,20 This treatment of BIPOC populations was condoned by the scientific community.
Scientific Racism in the 1800s in the US
Scientific racism—a pseudoscience purporting without evidence that perceived human physical and behavioral differences are due to race4—was used to justify the enslavement, segregation, land seizure, and genocide of BIPOC populations.2,4,21 Scientific racism was taught in medical schools, while science journals described experiments of burning and starving enslaved people, and pervasive scientific racism led to unethical medical studies and differential treatment by the biomedical community.5,6
In the 1830s and 1840s, physicians such as Samuel Morton and Charles Caldwell measured skulls from Native Americans and concluded that stealing their land was warranted because they were “slow” and that enslaving Africans was acceptable because their skulls demonstrated “tamable-ness.”4 Physician Samuel Cartwright argued that slavery was the natural state of Black people, and in 1851 he described 2 alleged mental illnesses, drapetomania and dysaesthesia aethiopica, as “diseases” that caused enslaved people to run away, perform subpar work, and not feel pain from physical punishment.22,23 He suggested liberty was the cause of these diseases and proposed whipping and other forms of cruelty as treatments.23
Racism was not only prevalent in scientific literature but also codified into health care institutions. The first psychiatric facility was founded in 1773, and its superintendent implied that enslaved people were acceptable forms of payment in exchange for receiving treatment.24 The American Psychiatric Association, founded in 1844, has recently acknowledged that since its creation, practitioners (including American Psychiatric Association members) have discriminated against, abused, experimented on, and victimized BIPOC communities in the name of science.24,25 Until 2015, its logo featured the face of Benjamin Rush, known as the “Father of American Psychiatry,”1,26,27 who believed that healthy skin was light colored and black skin was a form of leprosy that could be acquired through birth or interracial marriage.26,27 White physicians regularly conducted painful experiments on enslaved people in front of audiences, wrote about the enslaved people they used for experimentation in dehumanizing ways, performed gruesome and unethical surgeries, practiced on their corpses,28 and used psychiatry to validate slavery with false claims such as that insanity rates increased the further north that Black people lived (where slavery was less prevalent or absent).27,29
Scientific Racism in the 1900s to Today in the US
Although slavery was abolished in 1865, the Black Codes and Jim Crow system legalized discrimination and continued to limit Black people’s freedom9,30 and their access to health care long after. In 1900, the average life expectancy for White Americans was 49.6 years and 30–32 years for Black Americans.5 Certain demographic data are not available from this period due to lack of tracking. For example, the US Census Bureau reported that the population in 1900 was 87.9% White, 11.6% Black, 0.3% AI/AN, and 0.2% Asian and Pacific Islander, while Hispanic people were not systematically counted until the 1970 census,31,32 limiting discussion of racial and ethnic disparities in the early 20th century. Despite the absence of this historical data, there is ample evidence of scientific racism during this time. Psychiatrist James Woods Babcock contended that emancipation removed all “healthy” restraints from Black people, causing a rapid increase in rates of insanity.9,27 The first president of the American Psychological Association, G. Stanley Hall, published a textbook in 1904 describing AI/AN and African people as akin to impulsive, immature children.9 A subsequent president, Robert Yerkes, organized an effort to test the intelligence of 1.7 million army recruits and published his conclusion that recruited people of color had a “striking inferiority in intelligence.”33 Carl Jung, the founder of analytic psychiatry, worried that the mental and moral problem of “racial infection” would occur wherever White people were outnumbered by BIPOC populations, whom he described as “primitive.”9
These racist beliefs fed into the eugenics movement that began in the late 19th century, and eventually 31 US states passed sterilization laws.34 Between 1930 and 1960, an estimated 60,000 individuals (people of color, those with mental illness, and those with disabilities) in the US were forcibly sterilized to purportedly improve the genetic composition of the human race.5,27,29,34,35 The sterilization rate of women of childbearing age in Puerto Rico in the 1960s rose to over 35%—more than 10 times the rate as the rest of the US34,36—and the phrase “Mississippi appendectomy” was coined to describe the common practice of sterilizing hospitalized Black women.5,29 North Carolina sterilized Black women at > 3 times the rate of White women and > 12 times the rate of White men.37 Of those sterilized in federally financed programs in 1970, 43% were Black Americans, and in the 1970s 40% of AI/AN women were sterilized.34
The treatment of marginalized communities in the health care system paralleled that in the US biomedical research community, which conducted numerous unethical science experiments in the twentieth century. One such experiment was the government’s testing of mustard gas in the 1940s on 60,000 Americans to determine whether Black, Japanese American, or Puerto Rican soldiers differed in susceptibility to the gas compared to White soldiers.38 Scientific belief in biological racial differences drove these painful experiments, which many of the soldiers participated in because they were ordered to, or because they thought it was their patriotic duty.38 Many soldiers experienced long-term health issues after these experiments, such as problems with their eyes and lungs.38 Some of the Japanese American soldiers had been drafted directly from the US government’s internment camps.39 An infamous example of scientific ethical misconduct targeting BIPOC communities is the US Public Health Service’s Syphilis Study at Tuskegee, an experiment that ran from the 1930s–1970s by investigating syphilis in hundreds of poor Black men without informed consent, while withholding medication from them for nearly 30 years after penicillin had become standard treatment.29,40,41
In 1951 Henrietta Lacks, a poor Black mother farming the same land her ancestors were enslaved on, arrived at The Johns Hopkins Hospital with cervical cancer.42 Without her knowledge or consent, doctors cultured her cervical tissue cells and shared them widely. Although her cells revolutionized medicine, have been included in > 134,000 PubMed publications, and continue to be sold for profit today, her family has still not been compensated despite ongoing lawsuits (Lacks died from cancer in 1951).42,43 Lacks’s story is just one of many exemplifying the mistreatment of BIPOC populations during this time period.
Mistreatment of BIPOC populations by the medical community continued through the civil rights movement; The American Psychological Association president during that time, Henry Garrett, organized scientific opposition to the movement,33 and Black people who fought for racial equality were labeled as schizophrenic to rationalize hospitalizing them.26,44 Planned Parenthood of San Antonio, Texas, sponsored a 1968 study in which 70 low-income H/L women were told they would all receive contraception, but in fact half were given a placebo without being informed of that possibility.36 Prejudice and biases also impacted medical diagnoses. Research from the 1970s and 1980s indicated that White therapists often misdiagnosed H/L clients due to lack of cultural awareness, and evaluated their Black clients as more psychologically impaired than their Black peers did.45 Psychiatrists often labeled frustration as neuroticism in White patients but as schizophrenia in non-White patients, and when presented with clinical vignettes, they diagnosed schizophrenia more often in Black patients than White patients.24 Snowden and Cheung (1990) pointed out that diagnostic bias was also likely happening to Asian and AI/AN patients but had not been given the same level of attention.46
When the deinstitutionalization of mental health care began (a push to move patient care from state psychiatric institutions to community settings), White patients benefited more than BIPOC patients. Between 1970 and 1986, inpatient hospitalization rates dropped 54% for White patients but only 20% for BIPOC patients.45 Researchers in the 1980s found that Black and H/L patients with bipolar disorder were more often misdiagnosed with schizophrenia than White patients.45 The health care system has been slow to change; throughout the 2000s researchers have continued to find that Black, Asian, and H/L people are diagnosed with schizophrenia at significantly higher rates.47
Throughout the second half of the 20th century, psychologists continued publishing racist pseudoscience. Raymond Cattell, known for his work in multivariate personality research, promoted eugenics in his system of “Beyondism” and argued into the 1980s that the interbreeding of different groups of immigrants contributed to high crime and mental illness rates.33,48 Richard Herrnstein and Charles Murray (authors of The Bell Curve, a book steeped in scientific racism), as well as Philippe Rushton, argued that Black people are inherently less intelligent than White people.4,49 In the present day, psychologists still publish papers claiming that differences in behavior and intelligence are due to race,50 and Black physicians work in an environment where the word slave is used repeatedly in peer-reviewed medical journal articles and surgery rooms to refer to supportive parts of medical devices.51
At the end of the 20th century, differential treatment by the medical community continued to be associated with stark disparities in health and financial wellness for BIPOC populations compared with the White population. In the 1980s, the average median net worth was $43,279 for White, $4,169 for Black, and $5,524 for H/L renters and homeowners.52 During this period, compared with White Americans, H/L and AI/AN Americans had higher rates of end-stage renal disease,53,54 and Black Americans had 2 to 3 times higher rates of very low birthweight, infant mortality, maternal mortality, deaths from diabetes, and deaths from kidney disease.5 These disparities continued into the early 2000s, with Black and H/L patients receiving less health care than White patients, including fewer mental health visits, mammograms, and flu vaccinations.55,56
To this day, people who are H/L, AI/AN, or Black are far more likely to live in poverty in the US and less likely to have health insurance than White people.57–59 BIPOC children have higher rates of infant mortality, low birth weight, premature birth, obesity, and asthma than White children,60 and Black newborns die at nearly 3 times the rate as White newborns.61
A study of > 600,000 Americans’ health care use from 1963 to 2019 indicated that White people accessed health care more than Black people every single year during that nearly 6-decade period and that inequities have broadened in the last 5 years to reach a record high.62 Use of mental health services is also substantially lower for BIPOC populations than for the White population.56,57,59,63 Further, rates of youth antidepressant usage,59 high school suicide attempts,64 and completed suicides differ by ethnicity (eg, AI/AN females aged 15–19 years completed suicides at a rate nearly 4 times higher than White females).58
Compared with the general population, Black Americans are offered evidence-based psychotherapy or medication less frequently,57 and those with mental health conditions are imprisoned more frequently than Asian, H/L, or White Americans.57,65 Between 2016 and 2020, there were 116,722 excess premature deaths related to mental and behavioral health among BIPOC populations in the US, costing $278 billion (ie, from office and emergency room visits, hospitalizations, medications, and loss of life).65 These data do not even include the billions of dollars in mental and behavioral health excess costs arising from unhoused and incarcerated populations, where BIPOC populations are overrepresented.66 The COVID-19 pandemic has further highlighted health care inequities; compared with rates for non-Hispanic White Americans, COVID-19 hospitalization and death rates are higher for AI/AN (2.8 and 2.1 times higher, respectively), Black (2.2 and 1.7 times higher, respectively), and H/L (2.1 and 1.8 times higher, respectively) Americans.67
Racial and ethnic disparities in health care are reflected by the lack of diversity in the associated workforce. In 2018, the proportion of H/L, Black, and AI/AN physicians was much lower than that of the general US population (Figure 1).68,69 This result is problematic for numerous reasons, not the least of which is that physician-patient racial discordance is linked to worse communication, with shorter visits and lower levels of information-giving, satisfaction, and participatory decision-making.70 The mortality rate of Black newborns is reduced by 53% when a Black infant is cared for by a Black doctor versus by a White doctor.61 Addressing both the shortage of Black physicians and the ongoing racial and ethnic disparities in the health care system is a crucial need.
PERSISTENT SYSTEMIC INEQUALITIES
Terminology for Discussing Racism
Racial and ethnic disparities in physical and mental health care persist today, as does the structural racism that maintains them.10,11 In 2021, the American Psychiatric Association acknowledged that the discrimination “embedded within psychiatry” has contributed to BIPOC populations receiving poorer quality of care historically and to this day.24,25 Racism within psychiatry contributes to mental health disparities, misattribution of the causes of those disparities, scientific racism, and underrepresentation of marginalized populations in mental health research and treatment.11,71 Addressing racism in mental health care requires change from the individual to societal levels.71
Structural racism refers to a system where institutional practices, public policies, laws, ideologies, and customs work together to maintain inequities between racial and ethnic groups.12,72,73 In the US, structural racism is reinforced by inequitable systems and resources such as housing, education, wealth, employment, nutritious food, legal justice, and health care, with differential access for BIPOC and White populations.60,73,74
Interpersonal racism happens at the individual level as microaggressions and discrimination—intentional or unintentional.10,73 The vast majority of AI/AN, Black, H/L, and Asian Americans report having faced interpersonal racial discrimination (eg, slurs, harassment, threats, violence).75
Internalized racism occurs when an individual accepts and incorporates racist stereotypes and ideologies into their worldview; this self-stigmatization can lead to depressive symptoms and diminished well-being.73
The Connection Between Historical and Contemporary Inequities
BIPOC communities are systematically oppressed in the US, from where they live and their medical treatment to how they are policed and imprisoned. Many of the inequities that have historically occurred in the US continue today, including those stemming from redlining, racism in health care, slave patrols, and the leasing of people who are convicted.
After the Great Depression of the 1930s, the US government established the Home Owners’ Loan Corporation program to save homeowners from mortgage default.76 The program ranked city neighborhoods by lending risk, using racial demographics as one of the factors to compute risk; low risk areas were assigned the color green, and “hazardous” areas, the color red.76 Areas with BIPOC populations tended to be rated as higher risk and were described with terms such as “thoroughly blighted.”77,78 Today, many of the redlined areas (74%) in the US are still designated as low or moderate income, have a majority of BIPOC residents (64% of neighborhoods), and are associated with worse air pollution, less greenspace, higher temperatures, pre-term birth, delayed cancer diagnosis, and higher rates of poor physical and mental health.76,79,80
In addition to housing discrimination, BIPOC populations still experience discrimination in the health care system. The myth that Black people do not feel pain as much as White people—once used to validate performing surgeries without anesthesia on enslaved Black people4—persists in the current health care system, whereby doctors provide less pain medication to Black children than to White children for acute appendicitis and broken bones60 and National Collegiate Athletic Association medical staff believe Black athletes feel less pain than White athletes.81 Blackness was pathologized during slavery (eg, drapetomania, leprosy),22,26 and that continues today, as evidenced by recent studies that confuse race with genetic ancestry and imply that racial differences in health are biological rather than normal responses to systemic racism, oppression, exploitation, and trauma.7 As Opara and colleagues (2021) aptly stated: “Racism, not race, is the vector of disease and health disparities.”7(p226)
Historically, Black Americans have also been treated differently in the criminal justice system. The slave patrols of the early 1700s (formed to capture people attempting to escape slavery and to prevent revolts by people who were enslaved) grew into modern-day police forces in the US,75,82 with Black Americans often the targets of police violence. More than half of Black, H/L, and multiracial children report having been followed by a security guard in a store, and one-third have reported unfair treatment by a police officer.60 Police use force 3.6 times more often with and fatally shoot nearly 3 times more Black Americans than White Americans; they arrest proportionally more Black men than White men by age 23 (48.9% vs 37.9%); and they fatally shoot Black teens at 21 times the rate of White teens.82,83 On any given day in 2015, approximately 1.6% of White men, 3.9% of Hispanic men, and 9.1% of Black men aged 20–34 years were incarcerated.83
Convict leasing, whereby the majority Black prisoner population was forced into manual labor, historically funded the judicial system and US state economies (eg, in 1898, convict leasing accounted for 73% of Alabama’s revenue).84 The US continues to profit from prison labor. Although slavery has been banned, the 13th Amendment makes an exception for people convicted of crimes85; the US prison population, in which Black, AI/AN, and H/L people are heavily overrepresented,86–88 produces more than $11 billion annually in goods and services while unprotected by minimum wage laws, overtime, or workplace safety measures.85 The average maximum wage in prison is $0.52 per hour, and those incarcerated who refuse to work can be punished.85
Thus, historical discrimination in housing, medical treatment, policing, and incarceration of BIPOC communities has directly led to present-day inequalities. Systemic racism still permeates the nation, with drastic health consequences for BIPOC populations.75
Inequities in Clinical Trials
As with the broader US health care system,62,63,67 clinical trials are rife with racial and ethnic disparities, in terms of both their participants and the researchers who conduct them.89,90 Lack of diversity in clinical trials is both an ethical and a medical issue,91 and addressing this disparity was a primary motivator for the panel and this publication.
Participant diversity is crucial for trial results to be generalizable and trustworthy.90,92 Low participant diversity contributes to skewed clinical data91 and can exacerbate existing health disparities.92,93 For example, the predictive power of genetic data for complex traits is far lower for H/L, Asian, and African populations than for those of White European descent,94 giving them less access to accurate health information for making important clinical decisions.95 The pharmacokinetics and pharmacodynamics of medications can differ across patient populations, and the efficacy and safety profiles of a drug may vary for different races and ethnicities.91,96 Approximately 10%–21% of US Food and Drug Administration (FDA) newly approved drugs have known differences in terms of safety, efficacy, dosing, pharmacogenetics, or pharmacokinetics for various racial or ethnic groups.97,98 Despite this knowledge, most drugs approved by the FDA have been tested in clinical trials consisting primarily of White participants.95 The danger of this lack of diversity was demonstrated in clinical trials for 5-fluorouracil to treat cancer, in which study investigators missed the medication’s increased risk of toxicity in Black participants due to the low participant diversity in these trials.92 Because of such underrepresentation, BIPOC populations have benefited less from biomedical advances than White people in the US.91
In 2018, only 41% of the 213 clinical trials that reported results included race and ethnicity data from all 5 commonly reported groups (AI/AN, Asian, Black, H/L, White).89 In studies that did report racial and ethnic demographics, White participants were overrepresented and H/L, Asian, and AI/AN participants were all underrepresented.89 Despite underrepresentation in most clinical trials, Black people are overrepresented in trials that use the FDA’s exceptions from informed consent (EFIC) process.99 EFIC trials conduct research on people without decision-making capacity due to having life-threatening conditions with inadequate treatments; a systematic review of EFIC trials found that 29% of the participants were Black and the overwhelming majority of the experimental treatments were not effective.99 Black people are overrepresented in clinical trials of schizophrenia drugs100 and in psychiatric drug trials in general (45% of participants), while Asian (1.24%) and AI/AN (0.45%) people are underrepresented.101 In fact, just 0.17% of clinical research funded by the National Institutes of Health (NIH) from 1992 to 2018 focused on Asian American, Native Hawaiian, and Pacific Islander individuals.93 In randomized clinical trials of depression treatments, these individuals had the lowest rates of enrollment.102
To improve diversity in clinical trials, the FDA issued draft guidance in April 2022 recommending that sponsors submit a diversity plan to enroll participants from racial and ethnic populations in numbers that represent their proportions in the US.103 In 2018, the racial and ethnic makeup of the psychologist-based workforce indicated underrepresentation of Asian (4% vs 6%), Black (4% vs 13%), and Hispanic (6% vs 18%) psychologists versus the general US population.68,104 Similarly, at all levels of the psychiatry-based workforce, there are significantly fewer people from historically underrepresented populations among residents (16.2%), faculty (8.7%), and practicing physicians (10.4%) than in the general population (32.6%).105 NIH grant applications submitted by Black investigators are discussed at a lower rate (44% vs 57%) and funded at a lower rate (11% vs 18%) than those by White investigators.106 Although the NIH has attempted to address this disparity, researchers have argued that the efforts have been inadequate.107 Another factor driving racial and ethnic inequality in clinical trial populations is that some doctors have implicit biases that prevent them from discussing clinical trials with BIPOC patients, including believing these patients are less trustworthy, less compliant with treatment, mistrustful of the medical establishment, and overall poor trial candidates.108 However, one of the most effective methods for improving clinical trial recruitment of marginalized populations is community engagement.90
ADDRESSING DISPARITIES VIA COMMUNITY ENGAGEMENT
Defining Community Engagement
Since disparities in health care are rooted in socioeconomic inequality, the key to addressing them is partnering with individuals, agencies, and institutions in the community.109 Community engagement is “the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people.”109(p7) Through a two-way exchange of information, researchers learn the needs of the community, and the community learns the rationale of the researchers—both groups partner in designing, executing, and communicating the results of a study.3,90
Figure 2 shows one example of how community engagement can be implemented. It starts by building relationships with community stakeholders (eg, local health care providers [HCPs])110 and establishing one or more community advisory boards (CABs).111 A CAB is a formal group consisting of individuals from academia and/or the government (eg, researchers, policymakers) as well as the community (eg, patients, HCPs, social service agencies, community groups) who reflect the target research population, share their expertise, and advise researchers during each step of the clinical trial process.110,112
Next, researchers collaborate on the study design with the CAB, including revising inclusion/exclusion criteria, implementing changes to ensure participant safety and comfort, adapting the study protocol, and engaging patients (eg, sharing patient newsletters, birthday cards, thank you notes).111 After conducting the trial, clinical trial staff meet with community stakeholders to discuss trial findings and identify which are most relevant for disseminating to the community.110 Researchers can also meet with the CAB to discuss which findings would be of most interest to various stakeholders and tailor the content to specific audiences (eg, community forums, continuing education trainings).110 Staff then present findings to the community with interactive presentations that incorporate personal stories and show how community feedback was implemented in the study.110 Following the presentations, the staff schedule in-person and remote meetings with the community to further strengthen relationships.110 The goal is to cultivate an enduring synergistic relationship between researchers and the community.90
How the Community and Sponsor Benefit From Collaboration
Although community engagement takes time and resources from both the community and researchers, the many benefits outweigh the costs.109
Communities can benefit from community engagement by shaping the study to align with community needs and by gaining new skills, knowledge, and sustainable resources.109,113 Furthermore, communities benefit by participating in the study more easily, receiving financial compensation for their involvement, growing their network, increasing transparency of the research, understanding the pros and cons of participating in research, helping to develop programs in culturally appropriate ways, and becoming empowered.109,113 Community engagement is an effective tool for combating racial and ethnic disparities in clinical trials by increasing recruitment and participation of marginalized populations.113
Trial sponsors can benefit from community engagement by gaining access to funding sources that require community engagement as part of the research proposal, improving their study design and intervention through increased understanding of the community and the area of research, and identifying and resolving ethical problems that may arise (such as with consent).114 Sponsors can further benefit by broadening the impact of their results109 and laying the groundwork for recruitment for future studies.113 When the community is informed about a clinical trial and involved in it (such as by helping finalize consent forms), recruitment is enhanced (eg, by speeding up the process, recruiting more participants, increasing diversity).109,115
Implementing Solutions: New Approaches to Engaging With Communities
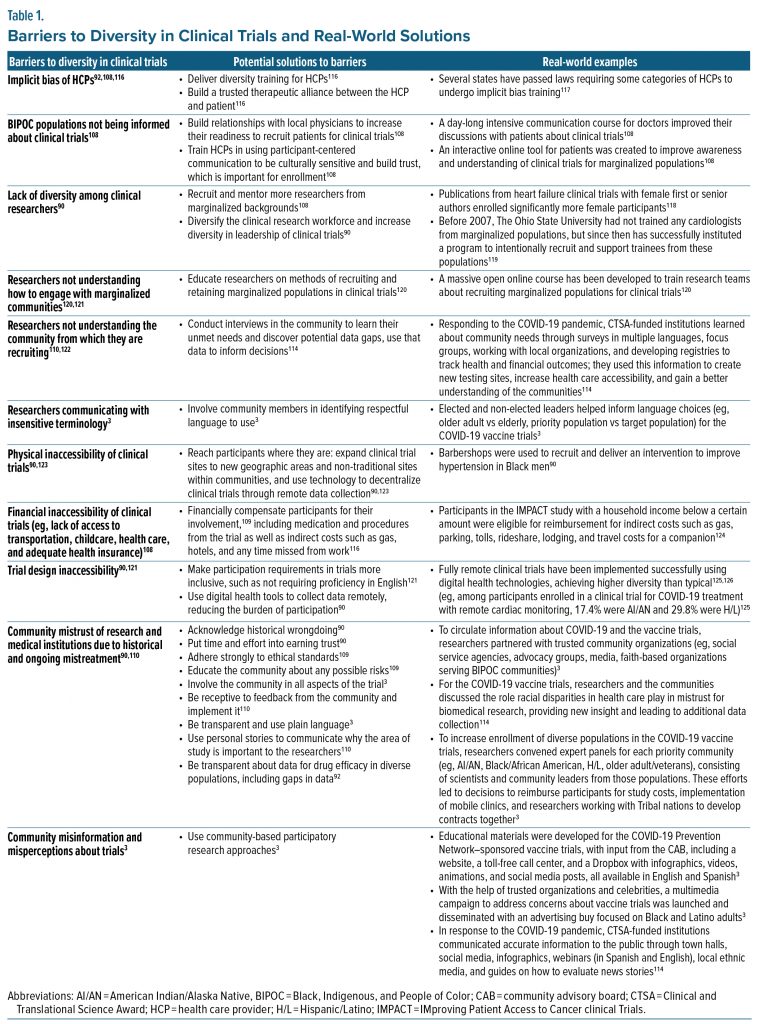
There are numerous barriers to increasing diversity in clinical trials; however, each has its potential solutions. Table 1 provides examples of how these strategies have been implemented in clinical trials.
One barrier to diversifying recruitment for clinical trials is lack of public awareness. Only a small proportion of patients are offered participation in clinical trials, but over half of those who are offered do enroll.127 Racially marginalized populations are as likely as non-Hispanic White populations to consent to participating in a clinical trial if given the opportunity; however, BIPOC populations are often not informed about clinical trials.108,128 This obstacle can be overcome by supporting and training HCPs in recruiting BIPOC participants, as well as offering patients information about clinical trials directly with online tools designed to educate and enroll racially and ethnically diverse participants.108
Another factor contributing to the lack of diversity among clinical trial participants is a similar lack of diversity among the researchers conducting the trials.90 Researchers do not always understand the communities they are recruiting from.120,122 Some White researchers are uncomfortable approaching people from marginalized populations, while others believe it is not even possible to increase diversity in research.121 Yet, it is crucial to integrate social and cultural factors when building research processes to ensure strong health outcomes.129 Fortunately, trainings have been designed for clinical trial research teams and HCPs to learn about including marginalized populations in clinical trials.108,120 To better understand the communities they are recruiting from and to ensure communication with culturally sensitive terminology,3,122 researchers have also interviewed community members and asked for their help identifying respectful language to use in consent forms and communications.3,114 There is a learning curve involved in building relationships with the community, but many studies have reported on their approach to this process, which is critical for building culturally appropriate interventions.129
Researchers need not only diversity training, but also to increase the diversity of the clinical research workforce by making it a priority to recruit, support, and mentor more researchers from marginalized populations, offering targeted professional development and tailored recruitment activities.90,108,119 Increased researcher diversity has been linked to increased participant diversity in clinical trials—one example is that published heart failure studies with female first or senior authors had a higher enrollment of female participants.118
Another barrier to diversity in clinical trials is the mistrust of medical research due to the past and present inequities and mistreatment experienced by BIPOC communities in the name of medical advancement, detailed earlier.90,110 Efforts to build trust through community engagement that have been implemented include acknowledging historical wrongdoing and current gaps in data,90,92 communicating plainly, being transparent,3,92 and implementing community feedback.110 Before asking for something from the community, researchers should first give to the community.130 After asking how to help the community, when conducting a trial, it is important for researchers to honestly share their intentions, honor their word, and alert the community to any changes in planning.130 The Resource Centers for Minority Aging Research achieved their goal of improving trust and relationships between 3 of their university sites (in California, North Carolina, and Colorado) and specific BIPOC communities through community engagement efforts such as hiring members of the community, integrating cultural practices with research protocols, and communicating trial results to the community.131 Another essential aspect of trust building is time. “Helicopter researchers” fly into a community, collect data, and leave; however, researchers should devote time to being continuously and actively engaged in not only their research but also their partnerships with the community.130
Accessibility and inclusivity are additional challenges to increasing diversity in clinical trials. Researchers should aim to ensure trials are physically and financially accessible and include participants from marginalized populations.90,108 For instance, researchers have expanded trial sites to non-traditional locations (eg, barbershops, community clinics),90,123 used digital health tools to collect data remotely,90 reimbursed participants for both the direct (eg, medication, procedures) and indirect (eg, gas, lodging, time off work) costs of participating in a trial,109,116 and removed barriers to participation such as requiring English proficiency.121 Community engagement practices have been implemented for decades and were successfully used to recruit representative samples of BIPOC participants to clinical trials for vaccines against COVID-19, illustrating that equitable enrollment is achievable.3
CONCLUSION
Human genetic diversity is far greater within than between populations, with continuous, extensive gene flow for hundreds of thousands of years showing all humans have a single evolutionary lineage.132–134 Despite lacking a meaningful biological basis,10,12,21,132,135 race is a real sociopolitical construct with drastic consequences in the US.8,10,18,136 From the time the Americas were first colonized to the present, racism has systematically disadvantaged BIPOC populations in the US,11,12 which has created a public health crisis.137 Clinical researchers can help to address this crisis by understanding how systemic racism creates and maintains racial and ethnic disparities in health care.11,12 The education process includes reading, reflecting, receiving training on providing culturally informed health care, cultivating friendships with people from different backgrounds, concentrating on social determinants of health, and participating in interventions aimed at institutional change.11,12 Moreover, supporting community engagement efforts is vital for increasing diversity in clinical trials,3 repairing the relationship between the biomedical community and the marginalized populations it has mistreated and exploited throughout history, and eliminating the pervasive racial and ethnic disparities in health care.
Clinical Points
- Compared with White people, Black, Indigenous, People of Color (BIPOC) populations are less likely to have health insurance and access health care less (including mental health services). Additionally, BIPOC populations have higher rates of infant mortality and have been harder hit by the COVID-19 pandemic.
- Racial and ethnic disparities are also widespread in clinical trials and a major ethical and medical concern.
- Diversity in clinical trials can be enhanced through community engagement efforts, an important step toward eliminating racial and ethnic disparities in health care.
© 2023 Physicians Postgraduate Press, Inc.
Published Online: June 12, 2023. https://doi.org/10.4088/JCP.23ah14887
To Cite: Ruiz-White I, Kramer L, Philips L, et al. Racial and ethnic disparities in physical and mental health care and clinical trials. J Clin Psychiatry. 2023;84(4):23ah14887.
Author Affiliations: Otsuka Pharmaceutical Development & Commercialization, Inc, Princeton, New Jersey (Ruiz-White, Wong, and Lonergan); Patient Advocacy and Community Engagement Evolution Research Group, New Providence, New Jersey (Kramer); Inside Edge Consulting Group, Princeton, New Jersey (Philips); and University of Arizona College of Medicine, Tucson, Arizona (Moreno). Dr Ruiz-White is not currently affiliated with Otsuka Pharmaceutical Development & Commercialization, Inc. but was at the time of the writing of the manuscript.
Corresponding Author: Inez Ruiz-White, PhD, Otsuka Pharmaceutical Development & Commercialization, Inc, 508 Carnegie Center Dr, Princeton, NJ 08540
([email protected]).
Relevant Financial Relationships: Mr Kramer, Mr Philips, and Dr Moreno are paid consultants of Otsuka Pharmaceutical Development & Commercialization, Inc. Dr Wong and Ms Lonergan are employees of Otsuka Pharmaceutical Development & Commercialization, Inc. Dr Ruiz-White is a former employee of Otsuka Pharmaceutical Development & Commercialization, Inc.
Funding/Support: This manuscript was funded and supported by Otsuka Pharmaceutical Development & Commercialization, Inc. Medical writing support was provided by Madeline Rose Keleher, PhD, of Oxford PharmaGenesis Inc., Newtown, Pennsylvania, and funded by Otsuka Pharmaceutical Development & Commercialization, Inc.
Acknowledgment: The authors thank John Kraus, MD, for leading a segment of the original oral presentation.
References (137)

- Smith C, Boyd JW. Social (in)justice and mental health. J Psychiatr Pract. 2021;27(5):406–408. CrossRef
- Andrasik MP, Maunakea AK, Oseso L, et al. Awakening: the unveiling of historically unaddressed social inequities during the COVID-19 pandemic in the United States. Infect Dis Clin North Am. 2022;36(2):295–308. PubMed CrossRef
- Andrasik MP, Broder GB, Wallace SE, et al. Increasing Black, Indigenous and People of Color participation in clinical trials through community engagement and recruitment goal establishment. PLoS One. 2021;16(10):e0258858. PubMed CrossRef
- Chowdhury K, Madden EF. Scientific racism attitudes among diverse undergraduate pre–health professions students. Pedagogy Health Promot. 2021;7(4):331–340. CrossRef
- Byrd WM, Clayton LA. An American health dilemma: a history of Blacks in the health system. J Natl Med Assoc. 1992;84(2):189–200. PubMed
- Byrd WM, Clayton LA. Race, medicine, and health care in the United States: a historical survey. J Natl Med Assoc. 2001;93(suppl):11S–34S. PubMed
- Opara IN, Riddle-Jones L, Allen N. Modern day drapetomania: calling out scientific racism. J Gen Intern Med. 2022;37(1):225–226. PubMed CrossRef
- Herd P, Mills MC, Dowd JB. Reconstructing sociogenomics research: dismantling biological race and genetic essentialism narratives. J Health Soc Behav. 2021;62(3):419–435. PubMed CrossRef
- Fernando S. Institutional Racism in Psychiatry and Clinical Psychology: Race Matters in Mental Health. Springer Nature; 2017.
- Flanagin A, Frey T, Christiansen SL; AMA Manual of Style Committee. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326(7):621–627. PubMed CrossRef
- Haeny AM, Holmes SC, Williams MT. Applying anti-racism to clinical care and research. JAMA Psychiatry. 2021;78(11):1187–1188. PubMed CrossRef
- Haeny AM, Holmes SC, Williams MT. The need for shared nomenclature on racism and related terminology in psychology. Perspect Psychol Sci. 2021;16(5):886–892. PubMed CrossRef
- Wilson TW, Grim CE. Biohistory of slavery and blood pressure differences in blacks today: a hypothesis. Hypertension. 1991;17(suppl):I122–I128. PubMed CrossRef
- Owens DC, Fett SM. Black maternal and infant health: historical legacies of slavery. Am J Public Health. 2019;109(10):1342–1345. PubMed CrossRef
- Coelho PRP, McGuire RA. Biology, diseases, and economics: an epidemiological history of slavery in the American South. J Bioeconomics. 1999;1(2):151–190. CrossRef
- Snyder TL. Suicide, slavery, and memory in North America. J Am Hist. 2010;97(1):39–62. CrossRef
- Reséndez A. Perspective: The Other Slavery. Smithsonian Institute. 2021. Accessed August 15, 2022. https://americanindian.si.edu/sites/1/files/pdf/seminars-symposia/the-other-slavery-perspective.pdf
- Shim RS. Dismantling structural racism in psychiatry: a path to mental health equity. Am J Psychiatry. 2021;178(7):592–598. PubMed CrossRef
- US Department of the Interior. Secretary Haaland Announces Federal Indian Boarding School Initiative. June 22, 2021. Accessed September 5, 2022. https://www.doi.gov/pressreleases/secretary-haaland-announces-federal-indian-boarding-school-initiative
- US Department of the Interior. Federal Indian Boarding School Initiative. Accessed October 1, 2022. https://www.bia.gov/service/federal-indian-boarding-school-initiative
- Price JL, Bruce MA, Adinoff B. Addressing structural racism in psychiatry with steps to improve psychophysiologic research. JAMA Psychiatry. 2022;79(1):70–74. PubMed CrossRef
- Smith KM. Discrimination and Racism in the History of Mental Health Care. July 6, 2020. Accessed August 8, 2022. https://nami.org/Blogs/NAMI-Blog/July-2020/Discrimination-and-Racism-in-the-History-of-Mental-Health-Care
- Cartwright S. Diseases and Peculiarities of the Negro Race. De Bow’s Review. 1851. https://www.pbs.org/wgbh/aia/part4/4h3106t.html.
- American Psychiatric Association. Historical Addendum to APA’s Apology to Black, Indigenous and People of Color for Its Support of Structural Racism in Psychiatry. January 18, 2021. https://psychiatry.org/news-room/historical-addendum-to-apa-apology
- American Psychiatric Association. APA’s Apology to Black, Indigenous and People of Color for Its Support of Structural Racism in Psychiatry. January 18, 2021. https://www.psychiatry.org/news-room/apa-apology-for-its-support-of-structural-racism
- Waite R, Hassouneh D. Structural competency in mental health nursing: understanding and applying key concepts. Arch Psychiatr Nurs. 2021;35(1):73–79. PubMed CrossRef
- Gordon-Achebe K, Hairston DR, Miller S, et al. Origins of Racism in American Medicine and Psychiatry. Humana Press; 2019.
- Kenny SC. Power, opportunism, racism: human experiments under American slavery. Endeavour. 2015;39(1):10–20. PubMed CrossRef
- Suite DH, La Bril R, Primm A, et al. Beyond misdiagnosis, misunderstanding and mistrust: relevance of the historical perspective in the medical and mental health treatment of people of color. J Natl Med Assoc. 2007;99(8):879–885. PubMed
- Iheme W. Black bodies in America as the metaphors for oppression, poverty, violence, and hate: searching for sustainable solutions beyond the black-letter law. J Black Stud. 2022;53(3):290–319. CrossRef
- Gibson C, Jung K. Historical Census Statistics on Population Totals by Race, 1790 to 1990, and by Hispanic Origin, 1970 to 1990, for the United States, Regions, Divisions, and States. United States Census Bureau. September 2002. https://www.census.gov/content/dam/Census/library/working-papers/2002/demo/POP-twps0056.pdf
- Cohn D. Census History: Counting Hispanics. Pew Research Center. 2010. Accessed March 3, 2010. https://www.pewresearch.org/social-trends/2010/03/03/census-history-counting-hispanics-2/
- Winston AS. Scientific Racism and North American Psychology. Oxford Research Encyclopedia of Psychology; 2020.
- Amy JJ, Rowlands S. Legalised non-consensual sterilisation—eugenics put into practice before 1945, and the aftermath, Part 1: USA, Japan, Canada and Mexico. Eur J Contracept Reprod Health Care. 2018;23(2):121–129. PubMed CrossRef
- Chatters LM, Taylor RJ, Schulz AJ. The return of race science and why it matters for family science. J Fam Theory Rev. 2022;14(3):442–462. PubMed CrossRef
- Cacari-Stone L, Avila M. Rethinking research ethics for Latinos: the policy paradox of health reform and the role of social justice. Ethics Behav. 2012;22(6):445–460. PubMed CrossRef
- Stern AM. Forced sterilization policies in the US targeted minorities and those with disabilities—and lasted into the 21st century. September 23, 2020. Accessed November 29, 2022. https://ihpi.umich.edu/news/forced-sterilization-policies-us-targeted-minorities-and-those-disabilities-and-lasted-21st.
- Smith SL. Mustard gas and American race-based human experimentation in World War II. J Law Med Ethics. 2008;36(3):517–521. PubMed CrossRef
- Killmeier MA. The family Nagashi: anti-racist radio and the Japanese internment. Radio Jl:Int Studs Broadcast Audio Media. 2018;16(2):185–205. CrossRef
- Alsan M, Wanamaker M, Hardeman RR. The Tuskegee Study of Untreated Syphilis: a case study in peripheral trauma with implications for health professionals. J Gen Intern Med. 2020;35(1):322–325. PubMed CrossRef
- Centers for Disease Control and Prevention. The Tuskegee Timeline. Accessed April 22, 2021. https://www.cdc.gov/tuskegee/timeline.htm
- Sodeke SO, Powell LR. Paying tribute to Henrietta Lacks at Tuskegee University and at The Virginia Henrietta Lacks Commission, Richmond, Virginia. J Health Care Poor Underserved. 2019;30(4S):1–11. PubMed CrossRef
- Kunzelman M. Henrietta Lacks estate sues company using her “stolen” cells. Associated Press. October 4, 2021.
- Misra S, Etkins OS, Yang LH, et al. Structural racism and inequities in incidence, course of illness, and treatment of psychotic disorders among Black Americans. Am J Public Health. 2022;112(4):624–632. PubMed CrossRef
- Wade JC. Institutional racism: an analysis of the mental health system. Am J Orthopsychiatry. 1993;63(4):536–544. PubMed CrossRef
- Snowden LR, Cheung FK. Use of inpatient mental health services by members of ethnic minority groups. Am Psychol. 1990;45(3):347–355. PubMed CrossRef
- Gurak K, Maura J, de Mamani AW, et al. Racial and ethnic diagnostic patterns in schizophrenia spectrum disorders. Cultural Comp Applied Psychol. 2018;603–617. CrossRef
- Zenderland L. Review: The Cattell Controversy. Race, Science, and Ideology by William H. Tucker. Hist Philos Life Sci. 2013;35(2):299–301. https://www.jstor.org/stable/43862184.
- Gillborn D, Heads I. Win, tails you lose: anti-black racism as fluid, relentless, individual and systemic. Peabody J Educ. 2018;93(1):66–77. CrossRef
- Winegard B, Winegard B, Anomaly J. Dodging Darwin: race, evolution, and the hereditarian hypothesis. Pers Individ Dif. 2020;160:109915. CrossRef
- Edwards S, Park J, Benjenk I, et al. A call to cease the use of slave analogies in medical literature. Ann Surg. 2022;276(2):e72–e74. PubMed CrossRef
- US Census Bureau. Income, Poverty, and Wealth in the United States: A Chart Book. 1992. https://www.census.gov/library/publications/1992/demo/p60-179.html
- Haffner SM, Mitchell BD, Pugh JA, et al. Proteinuria in Mexican Americans and non-Hispanic whites with NIDDM. Diabetes Care. 1989;12(8):530–536. PubMed CrossRef
- Newman JM, Marfin AA, Eggers PW, et al. End state renal disease among Native Americans, 1983–1986. Am J Public Health. 1990;80(3):318–319. PubMed CrossRef
- Fiscella K, Franks P, Doescher MP, et al. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40(1):52–59. PubMed CrossRef
- Biener AI, Zuvekas SH. Do racial and ethnic disparities in mental health treatment vary with underlying mental health? Med Care Res Rev. 2021;78(4):392–403. PubMed CrossRef
- American Psychiatric Association. Mental Health Disparities: African Americans. 2017. December 19, 2017. https://www.psychiatry.org/File%20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-African-Americans.pdf
- American Psychiatric Association. Mental Health Disparities: American Indians and Alaska Natives. December 19, 2017. https://www.psychiatry.org/File%20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-American-Indian-Alaska-Natives.pdf
- American Psychiatric Association. Mental Health Disparities: Hispanics and Latinos. December 19, 2017. https://www.psychiatry.org/File%20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-Hispanic-Latino.pdf
- Wright JL, Jarvis JN, Pachter LM, et al. “Racism as a public health issue” APS racism series: at the intersection of equity, science, and social justice. Pediatr Res. 2020;88(5):696–698. PubMed CrossRef
- Greenwood BN, Hardeman RR, Huang L, et al. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci U S A. 2020;117(35):21194–21200. PubMed CrossRef
- Dickman SL, Gaffney A, McGregor A, et al. Trends in health care use among black and white persons in the US, 1963-2019. JAMA Netw Open. 2022;5(6):e2217383. PubMed CrossRef
- Center for Behavioral Health Statistics and Quality SAMHSA. Racial/ethnic differences in mental health service use among adults and adolescents (2015–2019): Department of Health and Human Services; Report No: PEP21-07-01-002. 2021. https://www.samhsa.gov/data/sites/default/files/reports/rpt35324/2021NSDUHMHChartbook102221B.pdf
- Ivey-Stephenson AZ, Demissie Z, Crosby AE, et al. Suicidal ideation and behaviors among high school students: youth risk behavior survey, United States, 2019. MMWR suppl. 2020;69(1):47–55. PubMed CrossRef
- Hawthorne WB, Folsom DP, Sommerfeld DH, et al. Incarceration among adults who are in the public mental health system: rates, risk factors, and short-term outcomes. Psychiatr Serv. 2012;63(1):26–32. PubMed CrossRef
- Satcher Health Leadership Institute Morehouse School of Medicine; Eugene S. Farley, Jr. Health Policy Center at the University of Colorado Anschutz Medical Campus; Robert Graham Center. The Economic Burden of Mental Health Inequities in the United States Report. September 2022. https://satcherinstitute.org/wp-content/uploads/2022/09/The-Economic-Burden-of-Mental-Health-Inequities-in-the-US-Report-Final-single-pages.V3.pdf
- Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity. July 28, 2022. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- US Census Bureau. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States. 2019. Accessed November 8, 2022. https://data.census.gov/cedsci/table?q=S0201%202018&tid=ACSSPP1Y2018.S0201
- Association of American Medical Colleges. Diversity in Medicine: Facts and Figures 2019. Accessed 2019. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
- Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117–140. PubMed CrossRef
- Bryant BE, Jordan A, Clark US. Race as a social construct in psychiatry research and practice. JAMA Psychiatry. 2022;79(2):93–94. PubMed CrossRef
- Pacheco N, Trinh NH, Jahan A, et al. Dismantling structural racism in psychiatric residency training: nurturing a new generation of Black, Indigenous, and People of Color (BIPOC) psychiatrists. Acad Psychiatry. 2022;46(5):657–662. PubMed CrossRef
- Schouler-Ocak M, Bhugra D, Kastrup MC, et al. Racism and mental health and the role of mental health professionals. Eur Psychiatry. 2021;64(1):e42. PubMed CrossRef
- Rose JCC, MacManus C, MacDonald J, et al. Mitigating racial inequity by addressing racism in the criminal justice system: a behavior analytic approach. Behav Anal Pract. 2022;15(2):635–641. PubMed CrossRef
- Serchen J, Doherty R, Atiq O, et al; Health and Public Policy Committee of the American College of Physicians. Racism and health in the United States: a policy statement from the American College of Physicians. Ann Intern Med. 2020;173(7):556–557. PubMed CrossRef
- Nardone A, Rudolph KE, Morello-Frosch R, et al. Redlines and greenspace: the relationship between historical redlining and 2010 greenspace across the United States. Environ Health Perspect. 2021;129(1):017006. PubMed CrossRef
- Swope CB, Hernández D, Cushing LJ. The relationship of historical redlining with present-day neighborhood environmental and health outcomes: a scoping review and conceptual model. J Urban Health. 2022;99(6):959–983. PubMed CrossRef
- Michney TM, Winling L. New perspectives on new deal housing policy: explicating and mapping HOLC loans to African Americans. J Urban Hist. 2019;46(1):150–180. CrossRef
- Mitchell B, Franco J. Home Owners’ Loan Corporation “REDLINING” MAPS: the persistent structure of segregation and economic inequality: National Community Reinvestment Coalition. March 20, 2018. https://ncrc.org/holc/
- Lynch EE, Malcoe LH, Laurent SE, et al. The legacy of structural racism: associations between historic redlining, current mortgage lending, and health. SSM Popul Health. 2021;14:100793. PubMed CrossRef
- Druckman JN, Trawalter S, Montes I, et al. Racial bias in sport medical staff’s perceptions of others’ pain. J Soc Psychol. 2018;158(6):721–729. PubMed CrossRef
- McLeod MN, Heller D, Manze MG, et al. Police interactions and the mental health of Black Americans: a systematic review. J Racial Ethn Health Disparities. 2020;7(1):10–27. PubMed CrossRef
- Pettit B, Gutierrez C. Mass incarceration and racial inequality. Am J Econ Sociol. 2018;77(3–4):1153–1182. PubMed CrossRef
- Roberts JD, Dickinson KL, Hendricks MD, et al. “I can’t breathe”: examining the legacy of American racism on determinants of health and the ongoing pursuit of environmental justice. Curr Environ Health Rep. 2022;9(2):211–227. PubMed CrossRef
- American Civil Liberties Union, Global Human Rights Clinic. Captive Labor: Exploitation of Incarcerated Workers. 2022. https://www.aclu.org/report/captive-labor-exploitation-incarcerated-workers
- US Census Bureau. QuickFacts United States. Accessed August 22, 2022. https://www.census.gov/quickfacts/fact/table/US/PST045221. 2021
- Bureau of Prisons. Bureau of Prisons Statistics: Inmate Ethnicity. Accessed August 13, 2022. https://www.bop.gov/about/statistics/statistics_inmate_ethnicity.jsp
- Bureau of Prisons. Bureau of Prisons Statistics: Inmate Race. Accessed August 13, 2022. https://www.bop.gov/about/statistics/statistics_inmate_race.jsp
- Turner BE, Steinberg JR, Weeks BT, et al. Race/ethnicity reporting and representation in US clinical trials: a cohort study. Lancet Reg Health Am. 2022;11:100252. PubMed CrossRef
- Kelsey MD, Patrick-Lake B, Abdulai R, et al. Inclusion and diversity in clinical trials: actionable steps to drive lasting change. Contemp Clin Trials. 2022;116:106740. PubMed CrossRef
- Clark LT, Watkins L, Piña IL, et al. Increasing diversity in clinical trials: overcoming critical barriers. Curr Probl Cardiol. 2019;44(5):148–172. PubMed CrossRef
- Sharma A, Palaniappan L. Improving diversity in medical research. Nat Rev Dis Primers. 2021;7(1):74. PubMed CrossRef
- Ðoàn LN, Takata Y, Sakuma KK, et al. Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander participants funded by the US National Institutes of Health, 1992 to 2018. JAMA Netw Open. 2019;2(7):e197432. PubMed CrossRef
- Martin AR, Kanai M, Kamatani Y, et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet. 2019;51(4):584–591. PubMed CrossRef
- Knepper TC, McLeod HL. When will clinical trials finally reflect diversity? Nature. 2018;557(7704):157–159. PubMed CrossRef
- Gross AS, Harry AC, Clifton CS, et al. Clinical trial diversity: an opportunity for improved insight into the determinants of variability in drug response. Br J Clin Pharmacol. 2022;88(6):2700–2717. PubMed CrossRef
- Ramamoorthy A, Kim HH, Shah-Williams E, et al. Racial and ethnic differences in drug disposition and response: review of new molecular entities approved between 2014 and 2019. J Clin Pharmacol. 2022;62(4):486–493. PubMed CrossRef
- Ramamoorthy A, Pacanowski MA, Bull J, et al. Racial/ethnic differences in drug disposition and response: review of recently approved drugs. Clin Pharmacol Ther. 2015;97(3):263–273. PubMed CrossRef
- Feldman WB, Hey SP, Kesselheim AS. A systematic review of the Food and Drug Administration’s “exception from informed consent” pathway. Health Aff (Millwood). 2018;37(10):1605–1614. PubMed CrossRef
- Food and Drug Administration. Drug Trials Snapshots. Accessed January 3, 2023. https://www.fda.gov/drugs/drug-approvals-and-databases/drug-trials-snapshots
- Lolic M, Araojo R, Okeke M, et al. US racial and ethnic participation in global clinical trials by therapeutic areas. J Clin Pharm Ther. 2021;46(6):1576–1581. PubMed CrossRef
- Polo AJ, Makol BA, Castro AS, et al. Diversity in randomized clinical trials of depression: a 36-year review. Clin Psychol Rev. 2019;67:22–35. PubMed CrossRef
- Food and Drug Administration. Diversity Plans to Improve Enrollment of Participants from Underrepresented Racial and Ethnic Populations in Clinical Trials Guidance for Industry: Draft Guidance. April 2022. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/diversity-plans-improve-enrollment-participants-underrepresented-racial-and-ethnic-populations
- American Psychological Association. Psychology’s workforce is becoming more diverse. APA website. https://www.apa.org/monitor/2020/11/datapoint-diverse. November 1, 2020. Accessed August 30, 2022.
- Wyse R, Hwang WT, Ahmed AA, et al. Diversity by race, ethnicity, and sex within the US psychiatry physician workforce. Acad Psychiatry. 2020;44(5):523–530. PubMed CrossRef
- Hoppe TA, Litovitz A, Willis KA, et al. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci Adv. 2019;5(10):eaaw7238. PubMed CrossRef
- Taffe MA, Gilpin NW. Racial inequity in grant funding from the US National Institutes of Health. eLife. 2021;10:e65697. PubMed CrossRef
- Hamel LM, Penner LA, Albrecht TL, et al. Barriers to clinical trial enrollment in racial and ethnic minority patients with cancer. Cancer Contr. 2016;23(4):327–337. PubMed CrossRef
- Clinical and Translational Science Awards Consortium Community Engagement Key Function Committee Task Force on the Principles of Community Engagement. Principles of Community Engagement Second Edition. NIH Publication No. 11-7782; 2011.
- McDavitt B, Bogart LM, Mutchler MG, et al. Dissemination as dialogue: building trust and sharing research findings through community engagement. Prev Chronic Dis. 2016;13:150473. PubMed CrossRef
- Roennow A, Sauvé M, Welling J, et al. Collaboration between patient organisations and a clinical research sponsor in a rare disease condition: learnings from a community advisory board and best practice for future collaborations. BMJ Open. 2020;10(12):e039473. PubMed CrossRef
- Anderson KA, Dabelko-Schoeny H, Koeuth S, et al. The use of community advisory boards in pragmatic clinical trials: the case of the Adult Day Services Plus project. Home Health Care Serv Q. 2021;40(1):16–26. PubMed CrossRef
- Wieland ML, Njeru JW, Alahdab F, et al. Community-engaged approaches for minority recruitment into clinical research: a scoping review of the literature. Mayo Clin Proc. 2021;96(3):733–743. PubMed CrossRef
- Eder MM, Millay TA, Cottler LB. A compendium of community engagement responses to the COVID-19 pandemic. J Clin Transl Sci. 2021;5(1):e133. PubMed CrossRef
- Fregonese F. Community involvement in biomedical research conducted in the global health context; what can be done to make it really matter? BMC Med Ethics. 2018;19(suppl 1):44. PubMed CrossRef
- Woods-Burnham L, Johnson JR, Hooker SE Jr, et al. The role of diverse populations in US clinical trials. Med. 2021;2(1):21–24. PubMed CrossRef
- Cooper LA, Saha S, van Ryn M. Mandated implicit bias training for health professionals—a step toward equity in health care. JAMA Health Forum. 2022;3(8):e223250. PubMed CrossRef
- Reza N, Tahhan AS, Mahmud N, et al. Representation of women authors in international heart failure guidelines and contemporary clinical trials. Circ Heart Fail. 2020;13(8):e006605. PubMed CrossRef
- Auseon AJ, Kolibash AJ Jr, Capers Q. Successful efforts to increase diversity in a cardiology fellowship training program. J Grad Med Educ. 2013;5(3):481–485. PubMed CrossRef
- Kusnoor SV, Villalta-Gil V, Michaels M, et al. Design and implementation of a massive open online course on enhancing the recruitment of minorities in clinical trials—Faster Together. BMC Med Res Methodol. 2021;21(1):44. PubMed CrossRef
- Passmore SR, Kisicki A, Gilmore-Bykovskyi A, et al. “There’s not much we can do…” researcher-level barriers to the inclusion of underrepresented participants in translational research. J Clin Transl Sci. 2021;6(1):e4. PubMed CrossRef
- Erves JC, Mayo-Gamble TL, Malin-Fair A, et al. Needs, priorities, and recommendations for engaging underrepresented populations in clinical research: a community perspective. J Community Health. 2017;42(3):472–480. PubMed CrossRef
- Woodcock J, Araojo R, Thompson T, et al. Integrating research into community practice—toward increased diversity in clinical trials. N Engl J Med. 2021;385(15):1351–1353. PubMed CrossRef
- Borno HT, Zhang L, Zhang S, et al. Implementation of a multisite financial reimbursement program in cancer clinical trials integrated with patient navigation: a pilot randomized clinical trial. JCO Oncol Pract. 2022;18(6):e915–e924. PubMed CrossRef
- Mayfield JJ, Chatterjee NA, Noseworthy PA, et al; COVID-19 Early Treatment Team. Implementation of a fully remote randomized clinical trial with cardiac monitoring. Commun Med (Lond). 2021;1(1):62. PubMed CrossRef
- Ben-Zeev D, Chander A, Tauscher J, et al. A smartphone intervention for people with serious mental illness: fully remote randomized controlled trial of CORE. J Med Internet Res. 2021;23(11):e29201. PubMed CrossRef
- Unger JM, Hershman DL, Till C, et al. “When offered to participate”: a systematic review and meta-analysis of patient agreement to participate in cancer clinical trials. J Natl Cancer Inst. 2021;113(3):244–257. PubMed CrossRef
- Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics. 2021;39(6):653–665. PubMed CrossRef
- Haldane V, Chuah FLH, Srivastava A, et al. Community participation in health services development, implementation, and evaluation: a systematic review of empowerment, health, community, and process outcomes. PLoS One. 2019;14(5):e0216112. PubMed CrossRef
- Edwards HA, Monroe DY, Mullins CD. Six ways to foster community-engaged research during times of societal crises. J Comp Eff Res. 2020;9(16):1101–1104. PubMed CrossRef
- Holzer JK, Ellis L, Merritt MW. Why we need community engagement in medical research. J Investig Med. 2014;62(6):851–855. PubMed CrossRef
- Templeton AR. Biological races in humans. Stud Hist Philos Biol Biomed Sci. 2013;44(3):262–271. PubMed CrossRef
- Templeton AR. Human races: a genetic and evolutionary perspective. Am Anthropol. 1998;100(3):632–650. CrossRef
- Race, Ethnicity, and Genetics Working Group. The use of racial, ethnic, and ancestral categories in human genetics research. Am J Hum Genet. 2005;77(4):519–532. PubMed CrossRef
- Ibrahim Z, Brown C, Crow B, et al. The propagation of race and racial differences as biological in preclinical education. Med Sci Educ. 2022;32(1):209–219. PubMed CrossRef
- Thompson EC. The Problem of “Race as a Social Construct.” Anthropology News, American Anthropological Association. February and March 2006. https://understandingrace.org/pdf/rethinking/thompson.pdf
- Wright JH, Mishkind M. Computer-assisted CBT and mobile apps for depression: assessment and integration into clinical care. Focus Am Psychiatr Publ. 2020;18(2):162–168. PubMed CrossRef
This PDF is free for all visitors!
Save
Cite