Find more articles on this and other psychiatry and CNS topics:
The Journal of Clinical Psychiatry
The Primary Care Companion for CNS Disorders
CASE CONFERENCE
The Banner Alzheimer’s Institute Case Conference is a weekly event in which physicians and staff discuss challenging and/or teaching cases of patients seen at the Institute’s Memory Disorders Clinic. These conferences are attended by a multidisciplinary group that includes Banner Alzheimer’s Institute dementia specialists, community physicians (internal medicine, family medicine, and radiology), physician assistants, social workers, nurses, medical students, residents, and fellows.
BANNER ALZHEIMER’ S INSTITUTE
The Banner Alzheimer’s Institute located in Phoenix, Arizona, has an unusually ambitious mission: to end Alzheimer’s disease without losing a generation, set a new standard of care for patients and families, and forge a model of collaboration in biomedical research. The Institute provides high-level care and treatment for patients affected by Alzheimer’s disease, dementia, and related disorders. In addition, the Institute offers extensive support services for families and many unique and rewarding research opportunities.
Prim Care Companion CNS Disord 2013;15(2):doi:10.4088/PCC.13alz01518
© Copyright 2013 Physicians Postgraduate Press, Inc.
Received: March 22, 2013; accepted March 22, 2013.
Published online: April 25, 2013.
AUTHORS
Roy Yaari, MD, MAS, a neurologist, is associate director of the Stead Family Memory Clinic of Banner Alzheimer’s Institute and a clinical professor of neurology at the College of Medicine, University of Arizona, Phoenix.
Geri R. Hall, PhD, ARNP, GCNS, FAAN, is a gerontology clinical nurse specialist at Banner Alzheimer’s Institute and an adjunct clinical professor at the College of Nursing, University of Arizona, Phoenix.
Helle Brand, PA, is a physician assistant at the Stead Family Memory Clinic of Banner Alzheimer’s Institute.
Jan Dougherty, RN, MS, is director of Family and Community Services at Banner Alzheimer’s Institute.
Adam S. Fleisher, MD, MAS, is associate director of Brain Imaging at the Banner Alzheimer’s Institute, a neurologist at the Institute’s Stead Family Memory Clinic, and an associate professor in the Department of Neurosciences at the University of California, San Diego.
James D. Seward, PhD, ABPP, is a clinical neuropsychologist at Banner Alzheimer’s Institute.
Pierre N. Tariot, MD, a geriatric psychiatrist, is director of Banner Alzheimer’s Institute and a research professor of psychiatry at the College of Medicine, University of Arizona, Phoenix.
Corresponding author: Roy Yaari, MD, MAS, Banner Alzheimer’s Institute, 901 E. Willetta St, Phoenix, AZ 85006 ([email protected]).
CME Background
Original material is selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME activities on a variety of topics from volume to volume. This special series of case reports about dementia was deemed valuable for educational purposes by the Publisher, Editor in Chief, and CME Institute Staff. Activities are planned using a process that links identified needs with desired results.
To obtain credit, read the material and go to PrimaryCareCompanion.com to complete the Posttest and Evaluation online.
CME Objective
After studying this case, you should be able to:
- Manage patients with memory impairment and behavioral problems due to dementia, including providing support for patients’ caregivers
Accreditation Statement
The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation
The CME Institute of Physicians Postgraduate Press, Inc., designates this journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Creditâ„¢. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Note: The American Academy of Physician Assistants (AAPA) accepts certificates of participation for educational activities certified for AMA PRA Category 1 Creditâ„¢ from organizations accredited by ACCME or a recognized state medical society. Physician assistants may receive a maximum of 1.0 hour of Category I credit for completing this program.
Date of Original Release/Review
This educational activity is eligible for AMA PRA Category 1 Creditâ„¢ through April 30, 2016. The latest review of this material was April 2013.
Financial Disclosure
All individuals in a position to influence the content of this activity were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. In the past year, Larry Culpepper, MD, MPH, Editor in Chief, has been a consultant for AstraZeneca, Forest, Janssen, Lundbeck, Merck, Pfizer, and Takeda and has been a member of the speakers/advisory board for Merck. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears at the end of the article.
Ms A presented to the Stead Family Memory Clinic at the Banner Alzheimer’s Institute for a new patient evaluation with her husband, who provided the clinical history. Her husband is a reliable informant and presented a clear and detailed history. Ms A is an 80-year-old woman who was first noted to have deficits with short-term memory 3 years ago. At that time, a neurologist diagnosed her with mild cognitive impairment. Since then, her short-term memory has continued to gradually decrease, and she “constantly repeats the same questions.”
Currently, Ms A “cannot recall things said 5 minutes ago.” She misplaces dishes when emptying the dishwasher, is unable to track appointments even with a calendar, and can no longer follow a plot when watching television. Her husband took over managing the finances 2 years ago when she was struggling to balance their checking account. She drives a car rarely and only if her husband is with her. He reports that her driving is safe. Ms A is no longer able to shop alone, and her husband has gradually been doing more of the cooking. She is able to use a telephone but needs prompting for laundry and cleaning.
Ms A has had mild depressive features for much of her adult life, which is currently unchanged, but has developed occasional mild irritability specifically regarding taking medications. She has no psychotic features and is not socially inappropriate. Donepezil was initiated by Ms A’s primary care physician 2 months ago. She had no obvious benefit or side effects with 5 mg daily, but after 4 weeks of an increase to 10 mg, she developed severe nausea and mild headaches, and the dose was reduced back to 5 mg. The nausea resolved with reduction of the dose, but headaches persist.
PAST MEDICAL HISTORY
Ms A has a history of atrial fibrillation and has a pacemaker. She is treated for hypertension and insomnia.
ALLERGIES
Ms A has no known drug allergies.
MEDICATIONS
Ms A’s current medications are diltiazem, nebivolol, digoxin, hydrochlorothiazide, warfarin, trazodone 100 mg at bedtime, and donepezil 5 mg daily. Additionally, she takes zinc, fish oil, vitamin D, and vitamin C.
SOCIAL HISTORY
Ms A has 14 years of education and worked as a homemaker. She lives with her husband of 57 years. They have 2 children who live locally. There is no significant history of alcohol or tobacco use.
FAMILY HISTORY
Ms A’s father developed Alzheimer’s disease in his 80s.
PHYSICAL EXAMINATION
Ms A’s vital signs include blood pressure: 132/72 mm Hg, pulse: 80 bpm, height: 67 in, and weight: 151 lb. Her physical examination was unremarkable except for an irregular heart rhythm and bilateral cataracts.
NEUROLOGIC EXAMINATION
Ms A’s neurologic examination was unremarkable except for broken smooth pursuits. Frontal release signs were not present.
LABORATORIES/RADIOLOGY
Ms A had a recent head computed tomography (CT) that was unremarkable except for moderate atrophy. She also had a relatively recent complete blood count (CBC), comprehensive metabolic profile (CMP), and tests for vitamin B12 and thyroid-stimulating hormone (TSH) levels, all of which were unremarkable.
Smooth pursuit can be tested by asking the patient to track a small moving target at a distance of about 1 m, while keeping his/her head stationary. Both horizontal and vertical smooth pursuit should be assessed. The target should be moved at a slow uniform speed, and the pursuit eye movements are observed to determine whether they are smooth, broken up by catch-up saccades, or a fast movement of the eye. Because smooth pursuit requires the coordination of many brain regions, this is a nonspecific finding, but could be indicative of cerebral degeneration. Sudo et al (2010) reported that impaired smooth pursuit can be indicative of impaired intellectual and frontal lobe function and can be regarded as a primitive reflex (frontal release sign).
Different dementias may be associated with various physical examination findings. However, most often, the physical examination is normal in the early stages. Some subtle general findings can include frontal release signs such as a positive snout, glabellar, or palmomental reflex (Links et al, 2010).
A Mini-Mental State Examination score generally correlates with disease severity. Scores ≤ 9 points can indicate severe dementia, scores between 10-20 points can indicate moderate dementia, and scores > 20 points can indicate mild dementia (Mungas, 1991). Although MMSE scores must be interpreted in light of both the patient’s age and education, education is the primary demographic factor that affects scores. Therefore, whereas a cutoff of ≤ 23 is widely used in distinguishing between normal and abnormal performance, this cutoff may have less predictive ability in poorly educated individuals (Folstein et al, 1975).
Based on the information presented thus far, what would you expect the MMSE score to be?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. 26-30 | 11% |
| B. 21-25 | 78% |
| C. 16-20 | 11% |
| D. 11-15 | 0% |
| E. < 11 | 0% |
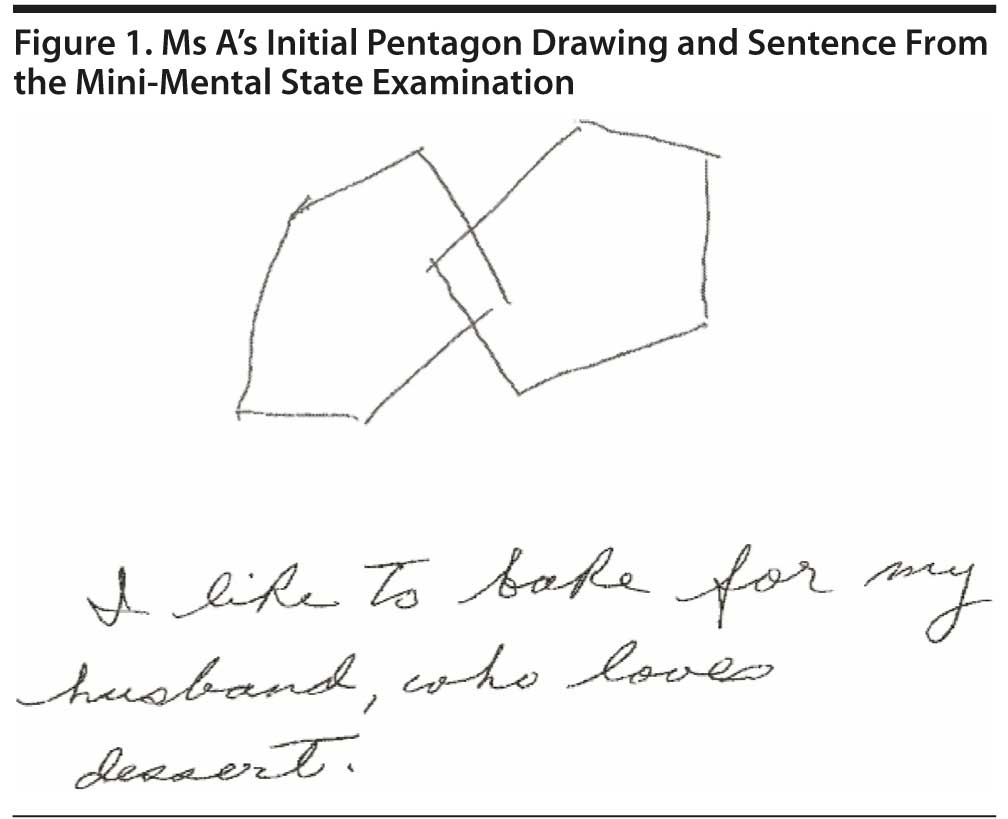
Most conference attendees predicted a mildly impaired MMSE score. Ms A scored 23 points on the MMSE; Figure 1 shows her pentagon drawing and sentence.
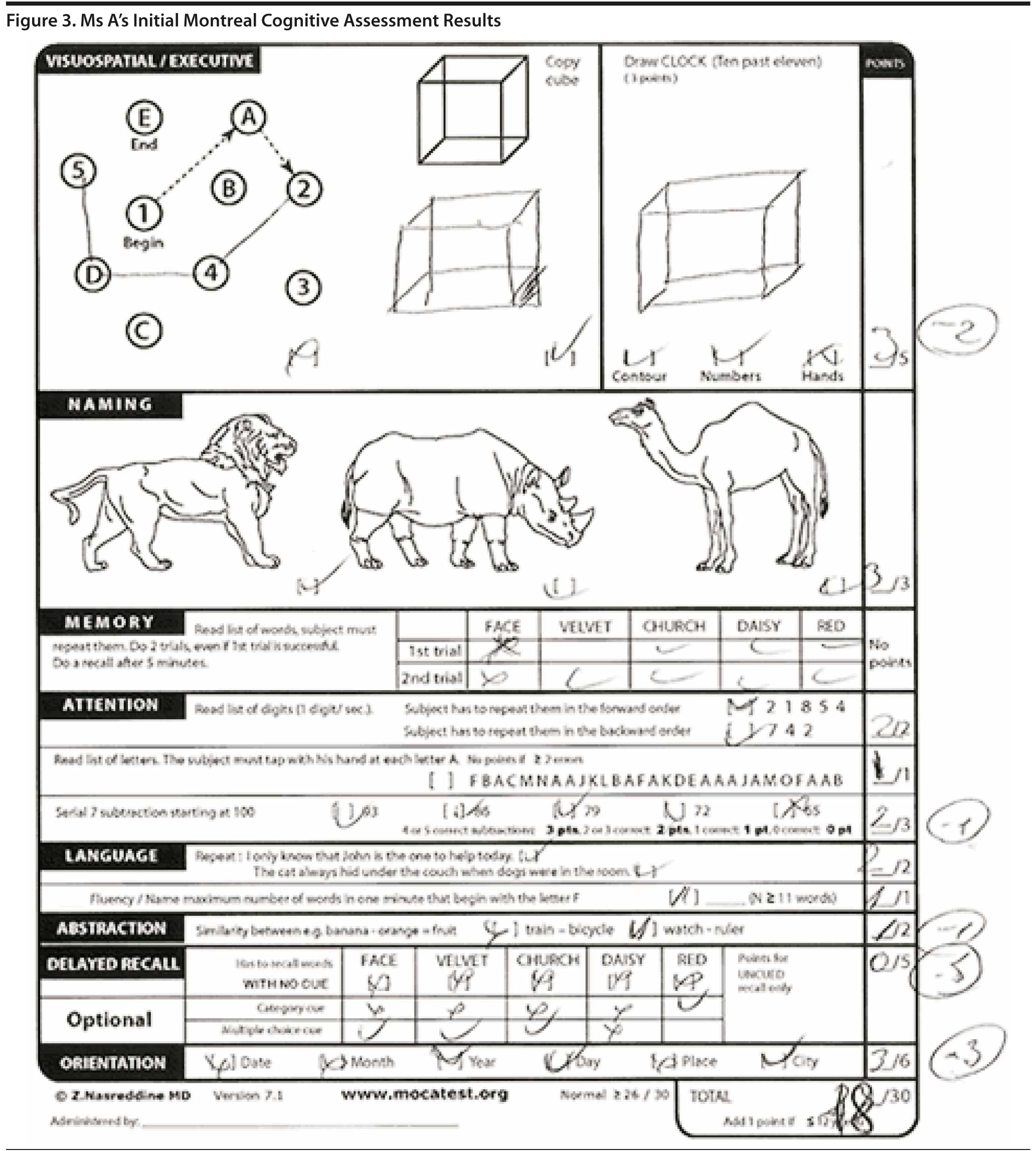
The Montreal Cognitive Assessment is a 30-point test that assesses several cognitive domains. Because it is more challenging than the Mini-Mental State Examination, it has greater sensitivity for mild cognitive impairment and early stages of dementia. With a cutoff score < 26, the sensitivity for detecting mild cognitive impairment (N = 94) was 90% and the specificity was 87% (Nasreddine et al, 2005). Research has demonstrated that MoCA scores are highly correlated with education. It is recommended that education be taken into account when interpreting MoCA performance, but there are no formal specific cutoff scores for lower education at this time (Johns et al, 2008). This test is available online at http://mocatest.org/.
Based on the information presented thus far, what would you expect the MoCA score to be?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. 26-30 | 0% |
| B. 21-25 | 33% |
| C. 16-20 | 67% |
| D. 11-15 | 0% |
| E. < 11 | 0% |
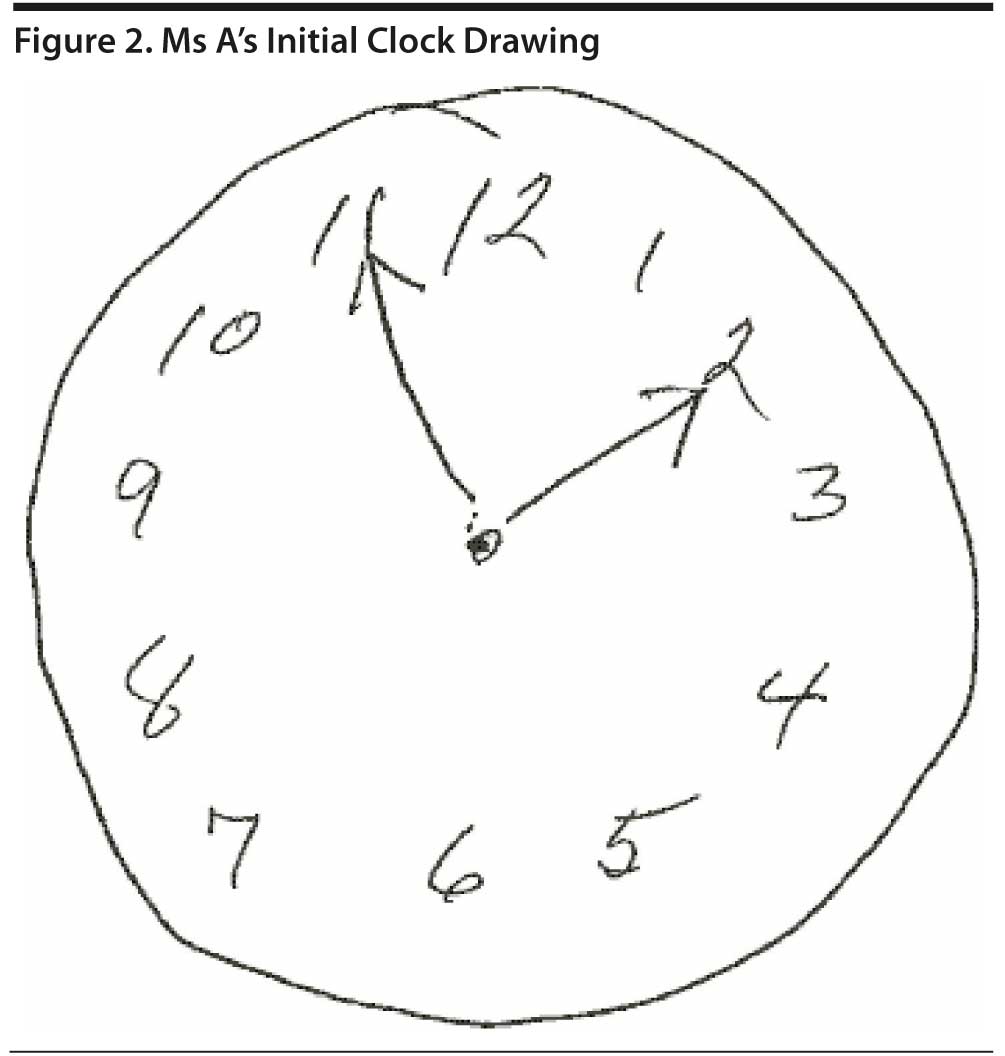
Figure 2 shows Ms A’s clock drawing. She scored 18 points on the MoCA (Figure 3).
The DSM-IV defines dementia as multiple cognitive deficits that include memory impairment and at least 1 of the following cognitive disturbances: aphasia, apraxia, agnosia, or a disturbance in executive functioning. The cognitive deficits must be sufficiently severe to cause impairment in social or occupational functioning and must represent a decline from a previously higher level of functioning. A diagnosis of dementia should not be made if the cognitive deficits occur exclusively during the course of a delirium (American Psychiatric Association, 2000).
Based on the information presented thus far, do you believe that Ms A meets criteria for dementia?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Yes | 100% |
| B. No | 0% |
Ms A has experienced the insidious onset and gradual progression of memory loss and deficits of other cognitive domains that has led to impaired function of instrumental activities of daily life such as shopping, managing finances, and misplacing items.
Based on the information presented thus far, what is the most likely diagnosis?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Frontotemporal dementia | 0% |
| B. Alzheimer’s disease | 100% |
| C. Mild cognitive impairment | 0% |
| D. Pseudodementia | 0% |
| E. Vascular dementia | 0% |
All conference attendees agreed that Alzheimer’s disease is the most likely diagnosis, although given Ms A’s history of atrial fibrillation and hypertension, vascular dementia should be considered in the differential diagnosis.
In April 2012, the US Food and Drug Administration (FDA) approved florbetapir F-18 amyloid positron emission tomography (PET) imaging in patients with cognitive impairment who are being evaluated for Alzheimer’s disease and other causes of cognitive decline. Florbetapir F-18 is a radioactive diagnostic agent that binds to amyloid plaques, a hallmark characteristic of Alzheimer’s disease, and is detected using PET scan images of the brain.
Up to this point, Ms A has had a head CT, CBC, CMP, and vitamin B12 and TSH tests, all of which were unremarkable. What further testing is indicated at this time?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Neuropsychological testing | 67% |
| B. FDG-PET | 0% |
| C. Lumbar puncture | 0% |
| D. Florbetapir PET (amyloid imaging) | 0% |
| E. No further testing is indicated | 33% |
Those conference attendees who chose “neuropsychological testing” argued that the results will clearly illustrate cognitive strengths and weakness that can be used as the basis of a care plan for the caregiver as well as the patient. This testing will also assess Ms A’s emotional status and determine if depression could be adversely affecting her cognition. In other words, although neuropsychological testing has both diagnostic and management rationale, for this patient, testing is helpful for management, while it is not necessary for diagnosis.
Those who chose “no further testing is indicated” stated that the clinical history and cognitive screening battery are quite clear, and neuropsychological testing will not provide significant information. Furthermore, in a patient who is displaying irritability, hours of cognitive tests could further increase agitation.
Guidelines for a routine dementia workup include CBC, CMP, vitamin B12, TSH, and structural brain imaging with either magnetic resonance imaging (MRI) or CT (Knopman et al, 2001). Although there was controversy regarding ordering neuropsychological testing, conference attendees did not suggest any other further testing.
Ms A could not tolerate donepezil 10 mg due to nausea and headaches. She continues with donepezil 5 mg daily but has persistent headaches that may be due to the donepezil, but it is uncertain. What action should be taken?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Discontinue donepezil. Initiate memantine. | 0% |
| B. Temporarily stop donepezil to assess whether headaches improve. | 67% |
| C. Discontinue donepezil. Initiate rivastigmine transdermal patch. | 33% |
| D. Continue donepezil 5 mg. Add acetaminophen 1,000 mg twice daily. | 0% |
Most conference attendees recommended a temporary hold of donepezil to assess if headaches resolve. If headaches resolve, then there is evidence that they are a side effect of donepezil. Some attendees wished to switch to rivastigmine transdermal patch to ensure that Ms A did not have a lapse in treatment. Memantine is currently not indicated on the basis of prescribing information, given that the patient is in the early stages of Alzheimer’s disease, and headaches are a possible side effect. The most common side effects of cholinesterase inhibitors (donepezil, rivastigmine, and galantamine) include cholinergic side effects of diarrhea, nausea, vomiting, and bradycardia (can be symptomatic with syncope), but headache is also a possible side effect. (Farlow et al, 2008).
Ms A rarely drives and only with her husband. Her husband has no concerns about driving safety. What action, if any, should be recommended regarding driving at this time?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. The patient must pass a formal on-road driving assessment in order to continue driving. | 44% |
| B. Driving should stop immediately. | 0% |
| C. Continue driving, as long as her husband continues to closely monitor. | 56% |
| D. Refer patient to a driving education class (American Automobile Association or American Association of Retired Persons). | 0% |
Some conference attendees felt that Ms A can continue to drive, even alone, as long as her husband monitors her driving very closely by being a passenger in the vehicle with her at least once every 2 weeks. Her husband should be asked whether he has to “copilot,” giving directions or prompts while she is driving. If this is the case, she should not drive alone, and her husband must be counseled that, at some point, she will not be able to follow his directions, placing both of them at risk. Others felt that driving can continue as long as she passes a formal on-road driving safety test either through the Department of Transportation or via a private facility. In either case, most attendees felt that she most likely could continue to drive but would need to be continually assessed for safety. At this time, Ms A and her husband should be warned of her safety risk, the public safety risk, and the legal and financial liability of driving with dementia. Also, her husband should be counseled as to warning signs of impaired driving safety such as the following:
- Incorrect signaling
- Trouble navigating turns
- Moving into the wrong lane
- Confusion at exits
- Parking inappropriately
- Hitting curbs/objects
- Driving at inappropriate speeds
- Delayed responses
- Missed stop sign/red light
- Increased agitation
- Scrapes or dents on car
- Becomes lost in familiar places
- Near misses (eg, car accident)
- Moving violation warnings
- Involved in car accident
- Confuses brake and gas
- Stops in traffic for no reason
- Needs prompts or directions to find familiar destinations
Currently, there are no clinical predictive tools of driving safety in dementia. The American Academy of Neurology published guidelines in 2010 (Iverson et al, 2010).
Patients and families can be directed to The Hartford Web site for further information on dementia and driving. This material can help family members understand how changes in the brain affect driving, as well as plan for driving cessation. Free guides from The Hartford regarding driving safety and dementia can be downloaded at http://www.thehartford.com/advance50/publications-on-aging.
IMPRESSION OF TREATING PHYSICIAN AT FIRST VISIT
Ms A is an 80-year-old woman who presents for a cognitive evaluation. The patient’s clinical history and cognitive findings are consistent with dementia. The most likely etiology of Ms A’s dementia is Alzheimer’s disease. She has mild long-standing depressive features, insomnia, and intermittent irritability. She has not been able to tolerate higher doses of donepezil and suffers from headaches, which may be a side effect.
PLAN
1. Stop the donepezil for 3 days. If the headaches improve, then discontinue the donepezil and initiate rivastigmine transdermal patch 4.6 mg daily. If headaches persist after stopping donepezil for 3 days, then the donepezil is not causing the headaches and donepezil 5 mg can be resumed and steadily rechallenged at a higher dose by increments of 2.5 mg up to 10 mg daily or 5 mg twice daily.
2. Memantine is not indicated at the current time.
3. Avoid use of acetaminophen PM given the anticholingergic properties of diphenhydramine. Address the issues pertaining to insomnia at the next appointment. Continue trazodone 100 mg at bedtime, which is inconsistently effective. General sleep hygiene strategies were reviewed.
4. Discussed the importance of optimizing physical, social, and mental activities.
5. Referred Ms A’s husband to caregiver education classes.
6. Discussed briefly the possibility of participating in clinical research. Ms A and her husband are amenable to this idea and would like to discuss in further detail at future visits.
7. Discussed the issue of driving. At the current time, Ms A’s driving is reportedly safe. Her husband will continue to monitor her driving. This issue will be reevaluated at the next visit.
8. Ms A will follow up in approximately 2 to 3 months.
Follow-Up 3 Months After the initial visit
When Ms A stopped donepezil, her headaches resolved. Transdermal rivastigmine 4.6 mg was administered for 4 weeks and was increased to 9.5 mg without incident. Via telephone calls, trazodone was gradually increased to 200 mg at bedtime with excellent control of insomnia. Ms A no longer takes acetaminophen PM.
Ms A’s husband observes worsening of short-term memory and worsening of depression. She is increasingly apathetic and needs more encouragement to be involved in hobbies and activities. There have been no changes in her ability to drive. Ms A’s husband has attended caregiver classes. He reports that Ms A is having difficulty “accepting the diagnosis,” which “lowers her spirits” and further irritates her. He was instructed to avoid focusing on accepting her illness.
IMPRESSION
Ms A is an 80-year-old woman with Alzheimer’s disease. She has worsening depressive symptoms. Her headaches resolved with discontinuation of donepezil. Her insomnia resolved with higher doses of trazodone. She continues to have depressive features with irritability.
PLAN
1. Continue rivastigmine 9.5 mg daily.
2. Memantine is not indicated at the current time.
3. Start citalopram 10 mg for treatment of depressive features.
4. Continue trazodone 200 mg at bedtime.
5. Ms A continues to drive but never drives alone. Her husband will continue to monitor the driving.
6. Ms A and her husband are very interested in clinical trial participation. They met with a study coordinator today for further discussion.
7. Ms A will follow up in approximately 3 to 4 months.
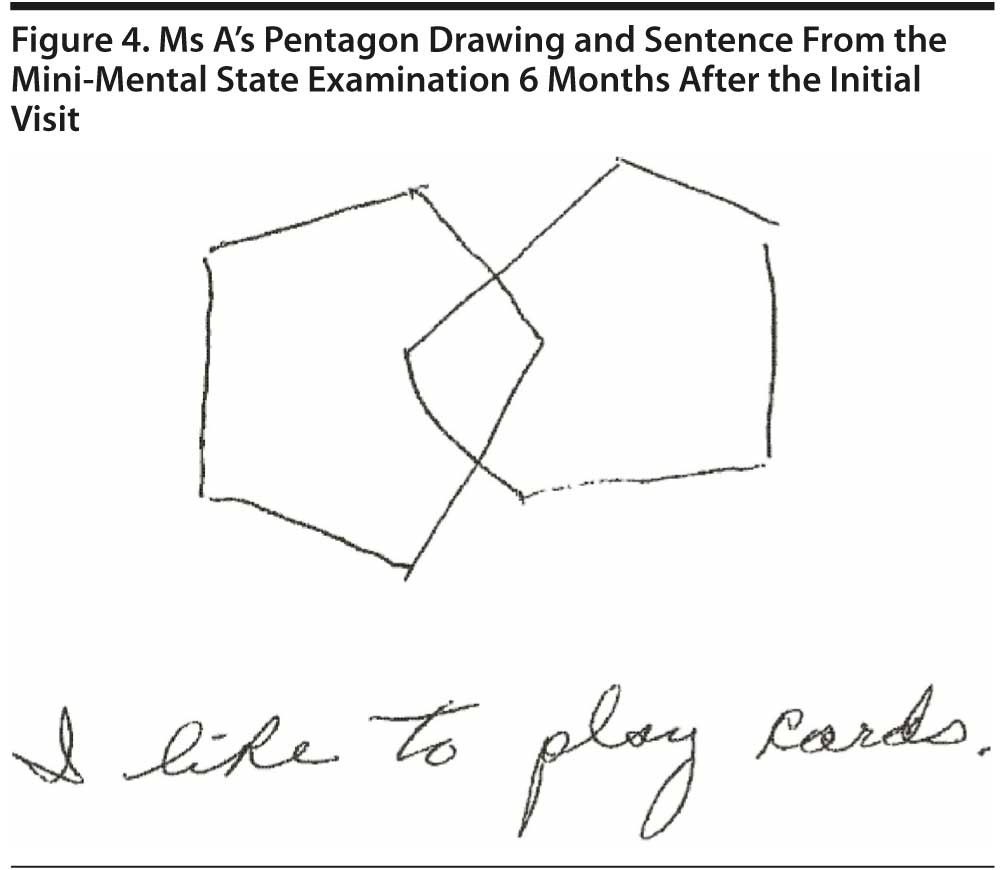
Follow-up 6 Months After the Initial Visit
Ms A’s husband notes significant improvement in her mood since initiating citalopram. The dose was increased to 20 mg via a phone call since the last appointment. Short-term memory, however, continues to significantly decline, and Ms A is increasingly repetitive. She continues to deny her diagnosis. The mention of Alzheimer’s disease angers and agitates her.
Ms A continues to drive, but very rarely. Ms A never drives alone because her husband is very concerned that she might get lost. Otherwise, he reports that her driving skills are intact and that she is a safe driver.
The MMSE was repeated. What would you expect the MMSE score to be?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. 26-30 | 0% |
| B. 21-25 | 11% |
| C. 16-20 | 89% |
| D. 11-15 | 0% |
| E. < 11 | 0% |
Ms A scored 21 points on the MMSE; Figure 4 shows her pentagon drawing and sentence.
At this time, should there be any further medication changes?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Switch rivastigmine to galantamine. | 0% |
| B. Discontinue rivastigmine. | 0% |
| C. Add memantine. | 33% |
| D. No further medical intervention at this time. | 67% |
What action, if any, should be taken regarding driving at this time?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Suggest to husband to gradually decrease driving frequency and stop over the next few weeks. | 22% |
| B. Notify the Department of Transportation. | 11% |
| C. Advise a formal on-road driving safety assessment. | 11% |
| D. Stop driving. | 56% |
Should they be told that driving must stop, it will be important to teach Ms A’s husband appropriate strategies. For example, instead of saying, “You can no longer drive,” her husband should say, “I’ ll drive this time. I need the practice.”
What action, if any, should be taken regarding Ms A’s refusal to accept her diagnosis?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Logically explain to her how the diagnosis was made; show results of cognitive testing. | 0% |
| B. Calmly review Alzheimer’s disease using brochures or informative Web sites. | 0% |
| C. Do not mention Alzheimer’s disease to her; terms such as memory issues or other terms may be a better alternative. | 100% |
| D. Refer patient and her husband to meet with a case manager. | 0% |
Note: The combination of impaired reasoning and lack of insight creates mood and behavioral issues when family members try to reason with and/or convince a loved one of a diagnosis of Alzheimer’s disease.
IMPRESSION 6 Months After the Initial Visit
Ms A is an 80-year-old woman with Alzheimer’s disease who has worsened cognitively since her last visit. Her depressive symptoms are controlled with citalopram, and insomnia is controlled with trazodone. Ms A prefers not to use the term Alzheimer’s disease and prefers other terms such as memory loss.
PLAN
1. At this time, initiate memantine, as Ms A appears to be encroaching upon the moderate stages of Alzheimer’s disease per clinical report and MMSE score. A starter pack was provided as well as a prescription for 10 mg twice daily. Potential side effects were discussed.
2. Continue transdermal rivastigmine 9.5 mg daily.
3. Continue trazodone 200 mg at bedtime and citalopram 20 mg daily.
4. Advised at this time to continue to wean Ms A off driving and subsequently stop driving over the next few weeks.
5. Discussed caregiver responses to the repetitive questioning such as:
- Ask “Why are you asking that?” and address concerns the patient expresses.
- Write the second answer on a card that the patient can carry and refer to.
- Use distraction such as “Can you help me with (name a task).”
- Understand that patients often obsess on plans announced in advance; thus, the caregiver should not announce plans in advance.
6. Ms A and her husband are interested in clinical trial participation and would like to be contacted should there be a suitable study, but Ms A has a pacemaker, which has excluded her from our current available studies.
7. Ms A will follow up in approximately 2 to 3 months.
Follow-Up 9 Months After the Initial Visit
Ms A was initiated on memantine at the last visit; however, after 1 week, worsening confusion was observed. The patient was unable to recognize her home or a close friend. She was unable to play a simple card game that she has never had problems with previously. After 18 days, memantine was discontinued. Within days, her cognitive status returned to baseline (Note: Confusion is a known rare side effect of memantine [Tariot et al, 2004]).
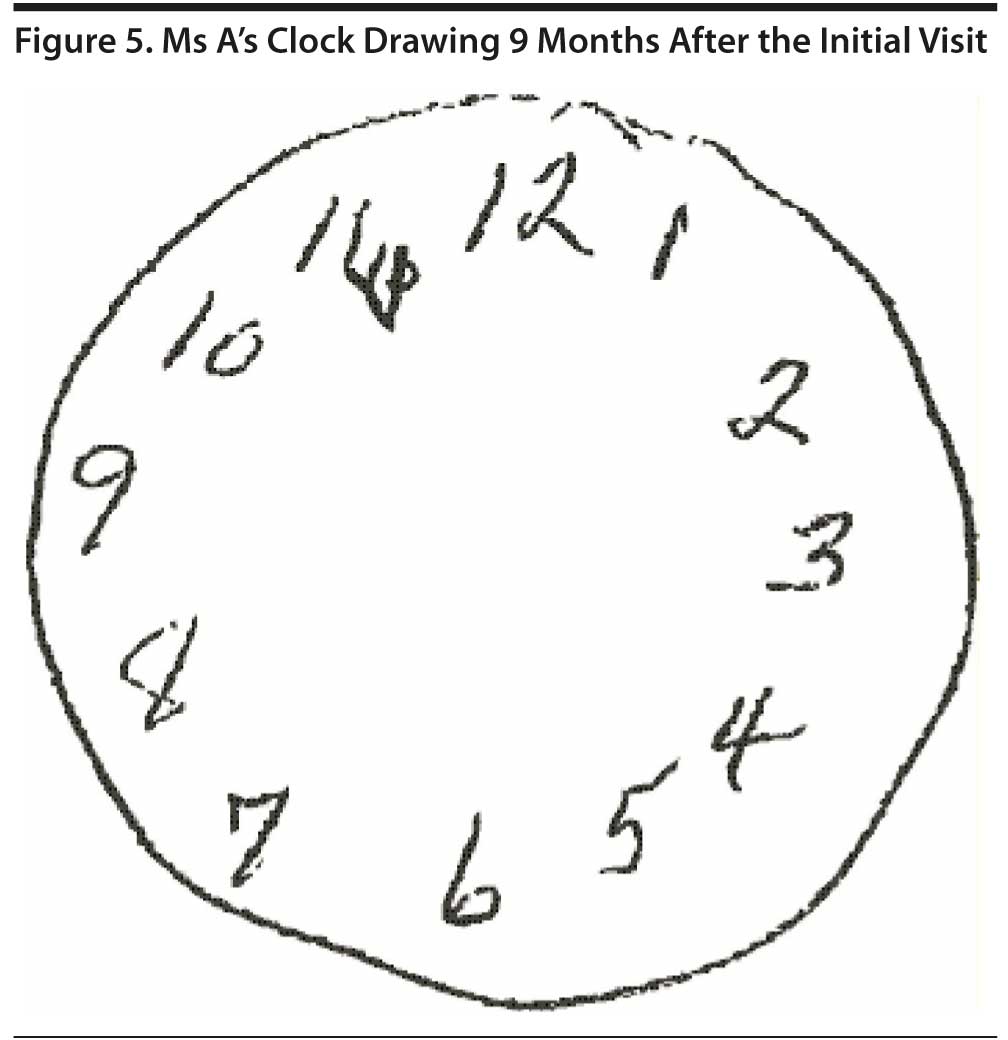
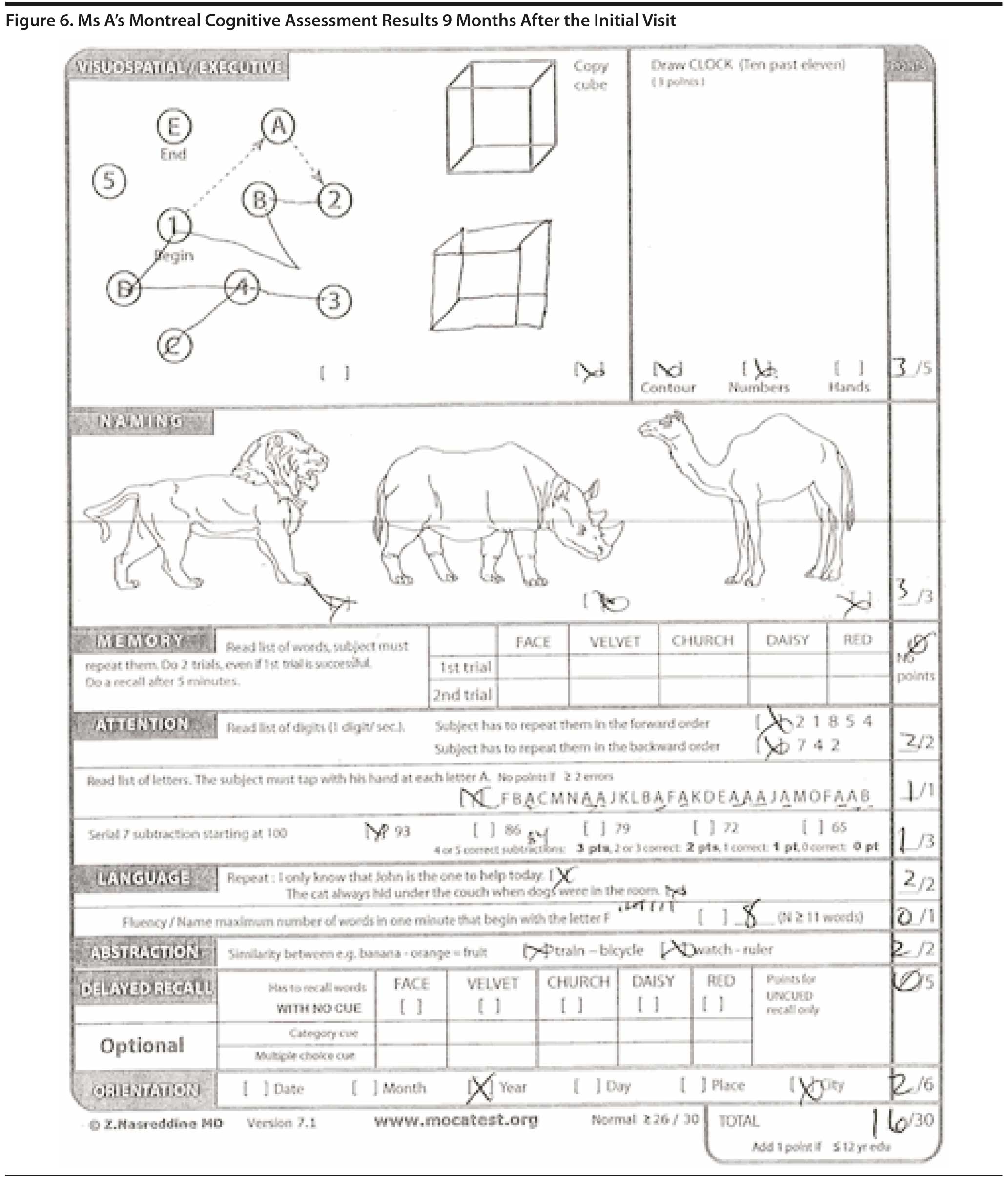
In the past 3 months, Ms A has had continued gradual worsening of short-term memory. She is now developing changes in her personality. She gets more frustrated and irritable when people ask her questions that she cannot answer. Ms A is no longer driving. Figure 5 shows Ms A’s clock drawing at this visit. A MoCA was repeated; Ms A scored 16 out of 30 (Figure 6).
IMPRESSION
Ms A is an 80-year-old woman with Alzheimer’s disease. Cognitive symptoms continue to gradually worsen from visit to visit. Her insomnia is controlled with trazodone. Ms A prefers not to use the term Alzheimer’s disease and prefers to use other terms such as memory loss. Depressive symptoms are worsening.
PLAN
1. Continue rivastigmine transdermal patch 9.5 mg daily. Ms A was not able to tolerate donepezil or memantine.
2. Continue trazodone 200 mg daily.
3. Continue citalopram 20 mg daily. Monitor depressive symptoms.
4. Ms A is no longer driving.
5. Ms A and her husband would like to be notified should there be any studies available that do not require MRIs, as she has a pacemaker.
6. Ms A will follow up in approximately 4 months.
Follow-Up Phone Call 12 Months After the Initial Visit
Ms A’s husband called in a panic reporting that Ms A ran out of the house this morning, banging on neighbors’ doors and yelling that she could no longer stand living with her husband. They had just returned from visiting family in northern Arizona for 2 days. Over the past 2 weeks, there have been increased episodes of agitated behavior, but “nothing like this.” The drive home was uneventful. When they returned home, Ms A suddenly became angry and agitated, fixated on the fact that she is no longer in control of their finances. She became distressed about not having money. Her husband physically pulled her back to the house “by her wrists.” Two neighbors helped to calm her down, and she remains calm. Ms A has a follow-up appointment scheduled in less than 2 weeks.
What is the best next step?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Initiate an atypical antipsychotic. | 0% |
| B. Suggest that she be seen by her primary care physician/urgent care to rule out an occult infection. | 100% |
| C. Recommend an inpatient geriatric psychiatry evaluation. | 0% |
| D. Increase citalopram. | 0% |
| E. No action. Await follow-up appointment in 2 weeks and reassess. | 0% |
A delirium due to an occult infection such as a urinary tract infection can result in a similar presentation, and, thus, an evaluation is warranted. The most likely etiology of Ms A’s agitated episode, however, is her response to the stress of traveling. People with dementia have ever-increasing trouble with changes of pace, changes in location, fatigue, groups of people, changes of time zone, and noise. In a familiar setting, there are many environmental cues that help a person with dementia to remain connected to reality such as a favorite chair or a familiar floor plan. Unfamiliar places can trigger fear, anger, and agitation (see supplementary material for the Travel Guide for People With Dementia). In addition to counseling regarding travel, Ms A’s husband will need to be counseled in regard to his response to his wife’s behaviors.
He should be counseled regarding the possible causes of the agitation and fear and instructed on measures to avoid the development of agitation as follows:
- Avoiding fatigue—having rest periods twice a day in a quiet area;
- Avoiding changes in routine, care provider, and relocation/travel;
- Having appropriate activities throughout the day;
- Avoiding questioning or trying to get the patient to recover lost functions;
- Controlling overwhelming or misleading stimuli (television);
- Preventing illness and treating pain.
Ms A’s husband should share these strategies with other family members and friends who may interact with his wife so they too can be aware of common behavioral triggers. Once catastrophic behaviors occur, he should be taught to treat his wife as if these behaviors are a panic attack as follows:
- Stop any activity;
- Try to get the patient to a secure and quiet place. If it occurs in a public setting such as a restaurant, leave;
- Reassure the patient she is safe in a soft voice. If she allows, rub her back or use gentle touch;
- Explore if the patient is hungry, in pain, or needs to use the bathroom and quietly accommodate these needs;
- Give the patient a 10-15 minute “time out” during which she is encouraged to rest quietly, possibly reading or listening to quiet music. The time out allows the person to rest and regain control and diminishes anxiety.
outcome of the follow-up Phone call
Ms A’s husband was instructed to take her to her primary care physician or urgent care to rule out an occult infection or other acute medical issue. She was seen by her primary care physician after her behavioral episode, and a physical examination, urinalysis, and basic laboratory results were normal.
Follow-Up Appointment 13 Months After the Initial Visit
Ms A continues to have intermittent episodes of agitated behavior. For example, she did not want to get out of the car for her appointment. When Ms A finally agreed to be seen, she insisted that she see the physician without her husband present. She insists that all items in their house belong to her, and her husband “can’ t do anything right.” Her husband states, “I can’ t disagree with her or she gets very angry.” “Little things” trigger agitation and anger.
Her husband has met with a social worker with the Family and Community Services team for caregiver counseling. They discussed the option of adult day health programs as well how to respond to her agitated behavior. For example, Mr A was counseled not to reason with his wife and to redirect the conversation. It was recommended that Ms A be on a consistent schedule with regular rest periods. Her response to groups and noise should be monitored and adjusted accordingly. Her daytime activities should include pleasurable activities. These activities need to be easily accessible for the caregiver. Common activities to utilize often include prerecorded old TV comedies and game shows, favorite music, picture books, and favorite foods that are generally soft and sweet (eg, chocolate and ice cream). In responding to Ms A’s behaviors, her husband should take a nonconfrontational approach.
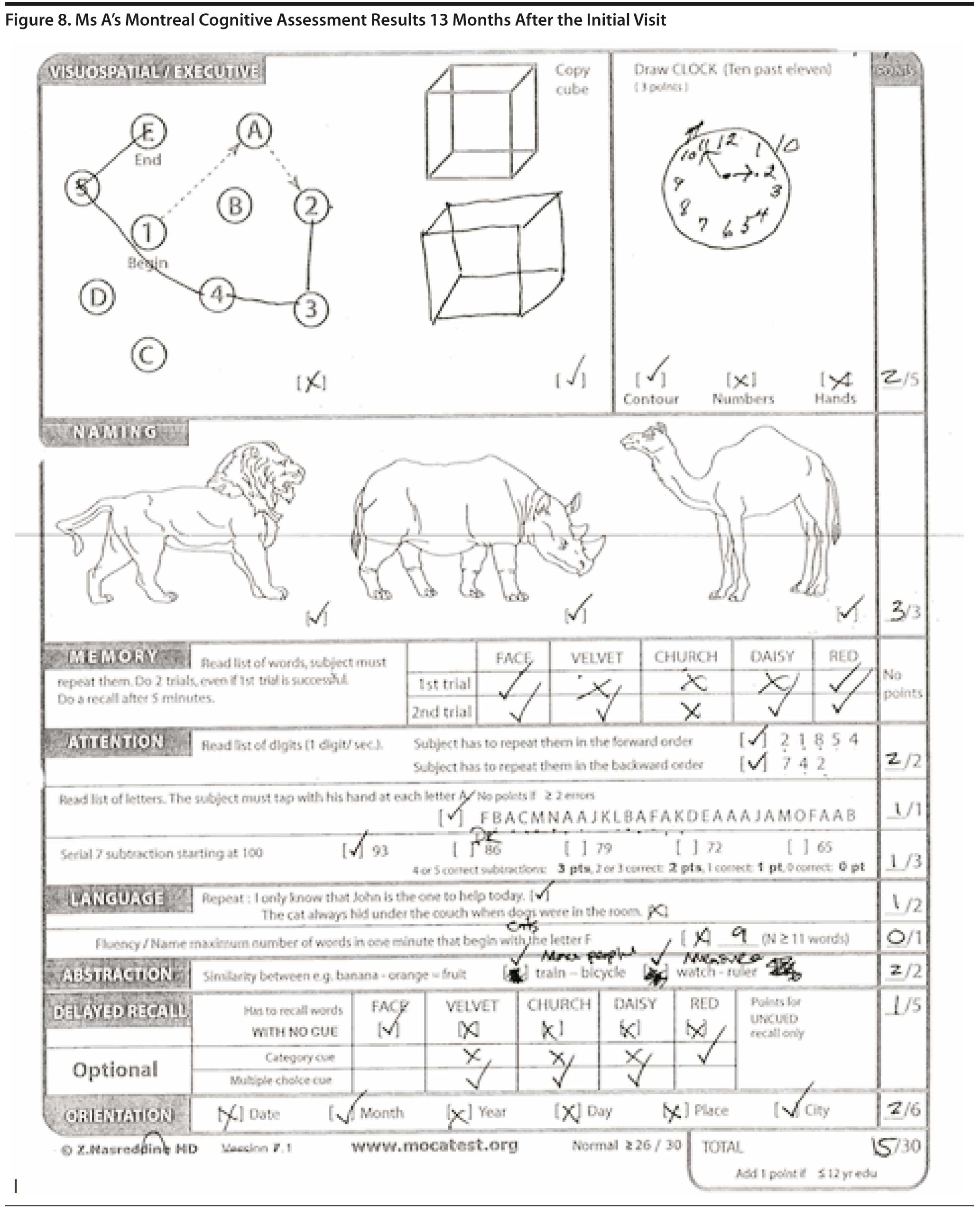
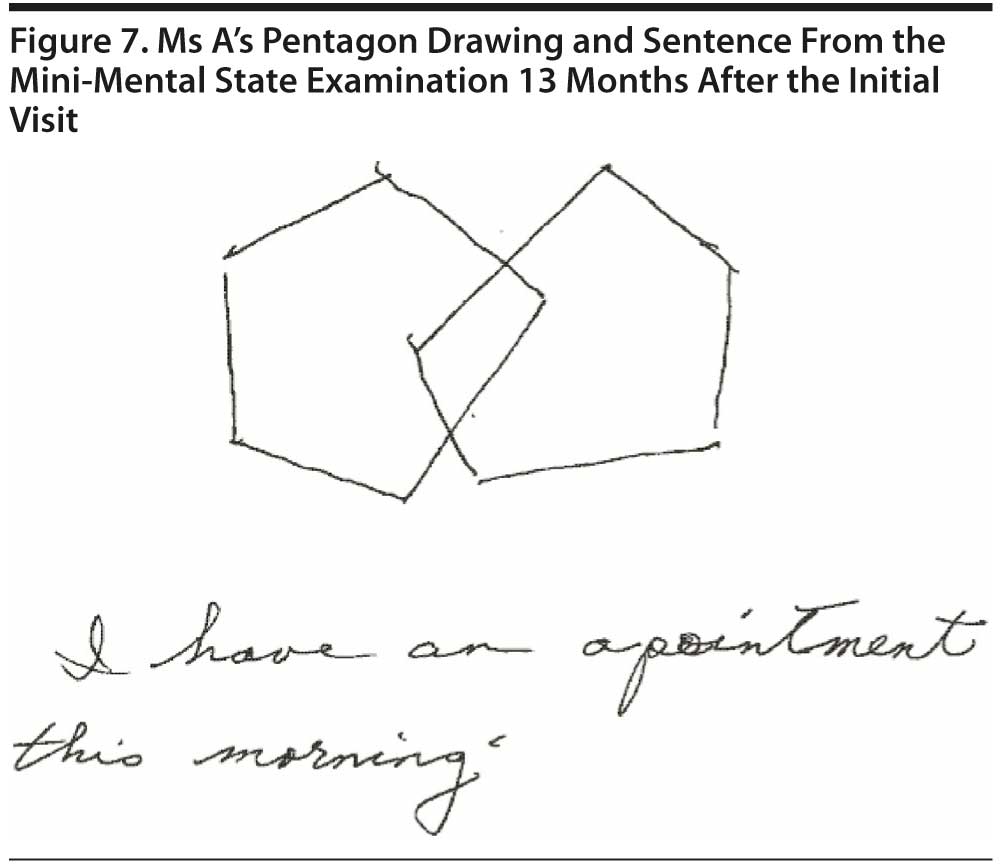
COGNITIVE TESTING
Ms A scored 21 points on the MMSE; Figure 7 shows her pentagon drawing and sentence. She scored 15 points on the MoCA (Figure 8).
What medication changes, if any, would you recommend at this time?
Your colleagues who attended the Banner Alzheimer’s Institute Case Conference answered as follows:
| A. Initiate an atypical antipsychotic such as quetiapine. | 17% |
| B. Switch the citalopram to a different antidepressant. | 0% |
| C. Initiate a typical antipsychotic such as haloperidol. | 0% |
| D. No medication changes; continue caregiver education. | 83% |
IMPRESSION 13 Months After the Initial Visit
Ms A is an 81-year-old woman with dementia due to Alzheimer’s disease. Cognitive symptoms continue to worsen, and she has developed agitated behaviors. Insomnia is well controlled with trazodone. Ms A prefers not to use the term Alzheimer’s disease and prefers to use other terms such as memory loss.
PLAN
1. Continue rivastigmine 9.5 mg daily. Ms A is not able to tolerate donepezil or memantine.
2. Given the significant agitated behaviors that have been emerging, initiate quetiapine 25 mg at bedtime with an additional 25 mg as needed every 24 hours for agitation. The side effects of this medication as well as the black box warning, which includes an increased incidence of heart attack, stroke, and all-cause mortality, were discussed at length with Ms A’s husband, who has medical power of attorney. Despite the potential risk of this medication, it was agreed that the potential benefit outweighs the potential risk at this time.
3. Continue citalopram 20 mg daily.
4. Once the quetiapine has been initiated, the trazodone could potentially be decreased.
5. Follow up in 6 weeks.
There are no US Food and Drug Administration (FDA)-approved medications to treat agitation or psychosis for Alzheimer’s disease, so use of atypical antipsychotics, which is common practice, is considered “off-label” use. Atypical antipsychotics carry an FDA boxed warning for use in dementia that states that these medications increase the risk of mortality by 1.6 to 1.7 fold. This warning is based on a meta-analysis of 17 trials, and although the causes of death were varied, most of the deaths were cardiovascular or infectious in nature (FDA, 2005).
Follow-Up 14.5 Months After the Initial Appointment
Ms A’s husband reported that quietiapine is “a miracle drug.” Her agitated behaviors have resolved, and she has returned to her baseline personality and behavior. She is “friendly again.” No further medication changes were made. She continues to take transdermal rivastigmine 9.5 mg daily, quetiapine 25 mg at bedtime, citalopram 20 mg daily, and trazodone 100 mg at bedtime.
Follow-Up 17 Months After the Initial Appointment
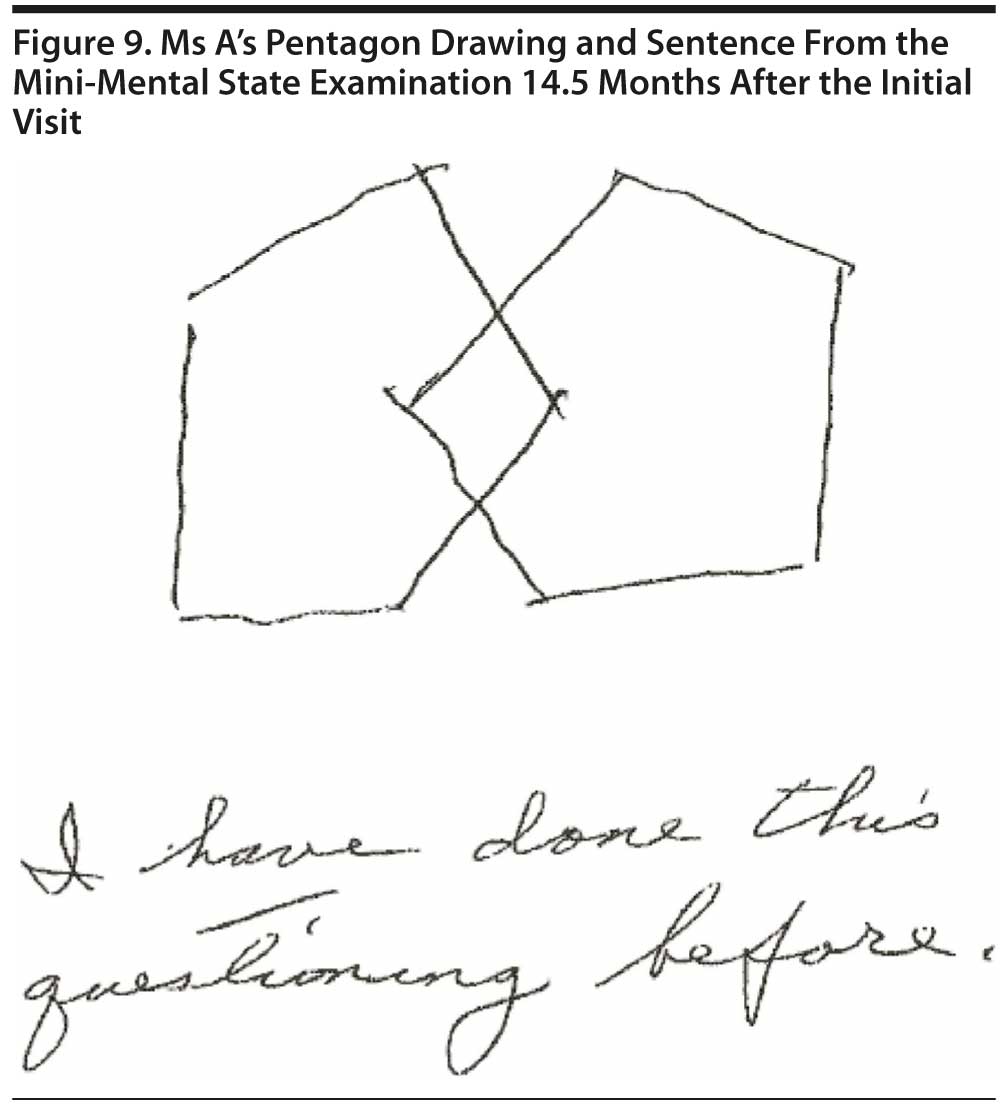
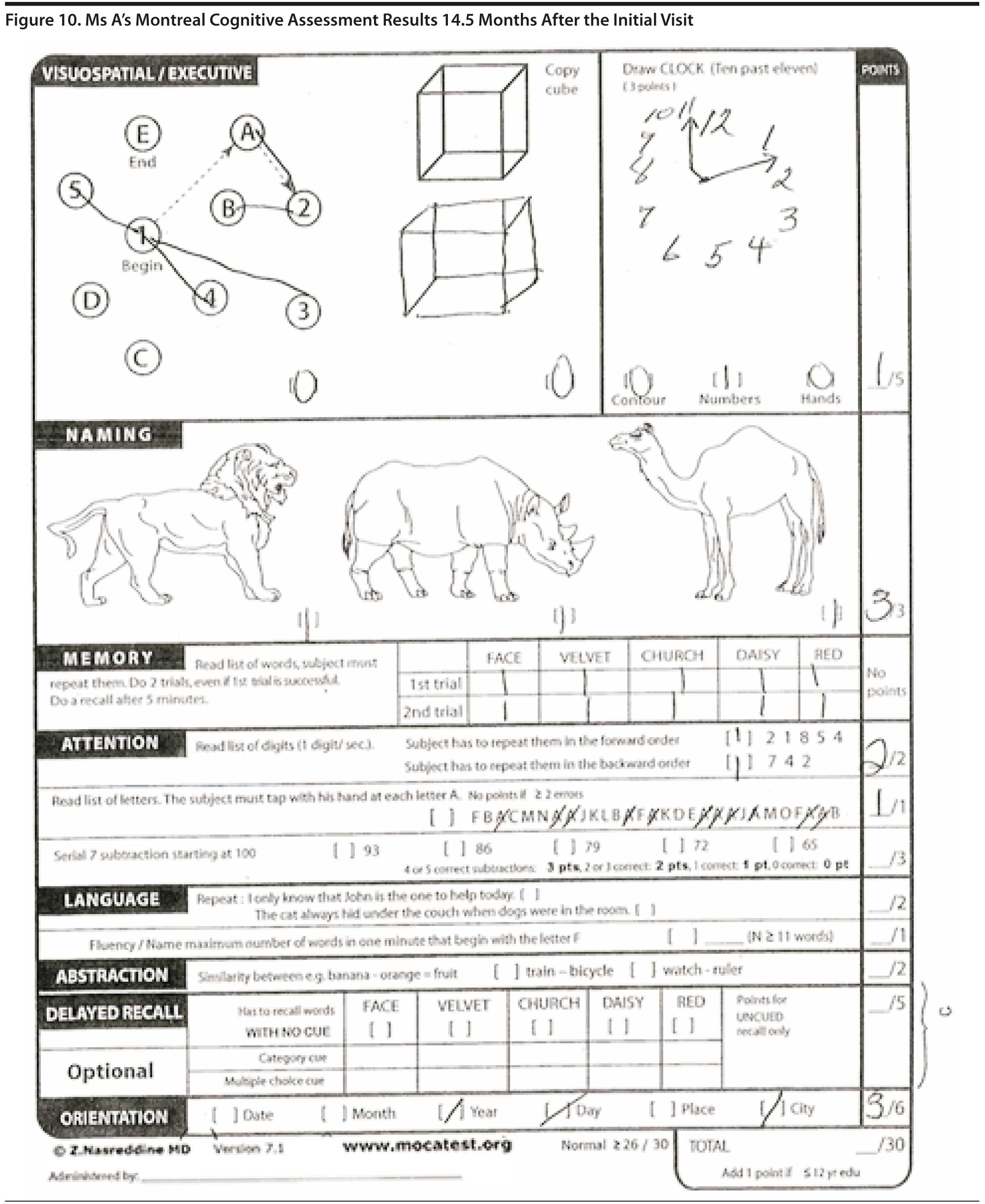
Ms A continues to live at home with her husband with support from their daughters. Due to an increase in morning agitation, Ms A has been taking an extra 25 mg of quetiapine every morning in addition to her evening dose. When she intermittently does not remember being married and does not recognize her husband, her agitation increases. She will lock herself in the bedroom. She is also insistent that she control her own medications and does not allow for assistance. Upon arriving to our institute, the sign at the entrance stating “Banner Alzheimer’s Institute” angered her, and she did not want to enter the building. She has no insight into her illness and does not believe she has a problem. The MMSE score was 21 of 30 and the MoCA score was 10 of 22. The MoCA was not fully completed, as Ms A grew angry and refused to finish the testing. Figure 9 shows Ms A’s pentagon drawing and sentence from the MMSE. Figure 10 shows Ms A’s MoCA results.
Impression
Ms A is an 81-year-old woman with moderate stage Alzheimer’s disease with significant behavioral issues. She refuses to take medications and demands control of them, focuses on wanting to drive, and intermittently does not recognize her husband. Behaviors seem to be worse in the early morning and then again in the late afternoon/early evening hours.
Plan
1. Increase quetiapine to 50 mg at bedtime and 25 mg in the morning, with an additional 25 mg as needed. Monitor and adjust as needed.
2. General communication strategies were discussed to minimize frustration and to address delusions. The discussion was also focused on identifying triggers for the behaviors and eliminating them either from the environment or from communication interactions.
3. Medications can be crushed, placed in food, or dissolved in liquid in order to facilitate taking them. Medication bottles should be placed out of sight so that they do not serve as a trigger for behaviors.
4. A men’s support group was recommended to Ms A’s husband, and the issue of caregiver stress and the need for respite was reviewed.
5. It was stressed that Ms A cannot be left alone and requires 24/7 supervision.
6. Ms A will follow up in 4 months.
Follow-Up 21 Months After the Initial Appointment
Ms A did not speak with her husband for 2 days after the last appointment. She refuses to come to the Banner Alzheimer’s Institute, and the term Alzheimer’s continues to cause great anger. She refused to attend today’s appointment, and her husband presented alone. She continues to cognitively worsen, but with the current medication regimen, her behavioral issues are generally very well controlled. Given her continued refusal to present to the “Alzheimer’s Institute,” we agreed that we will manage any new issues via the telephone, so long as Ms A is seen in the clinic at least once a year.
Follow-Up 31 Months After the Initial Appointment
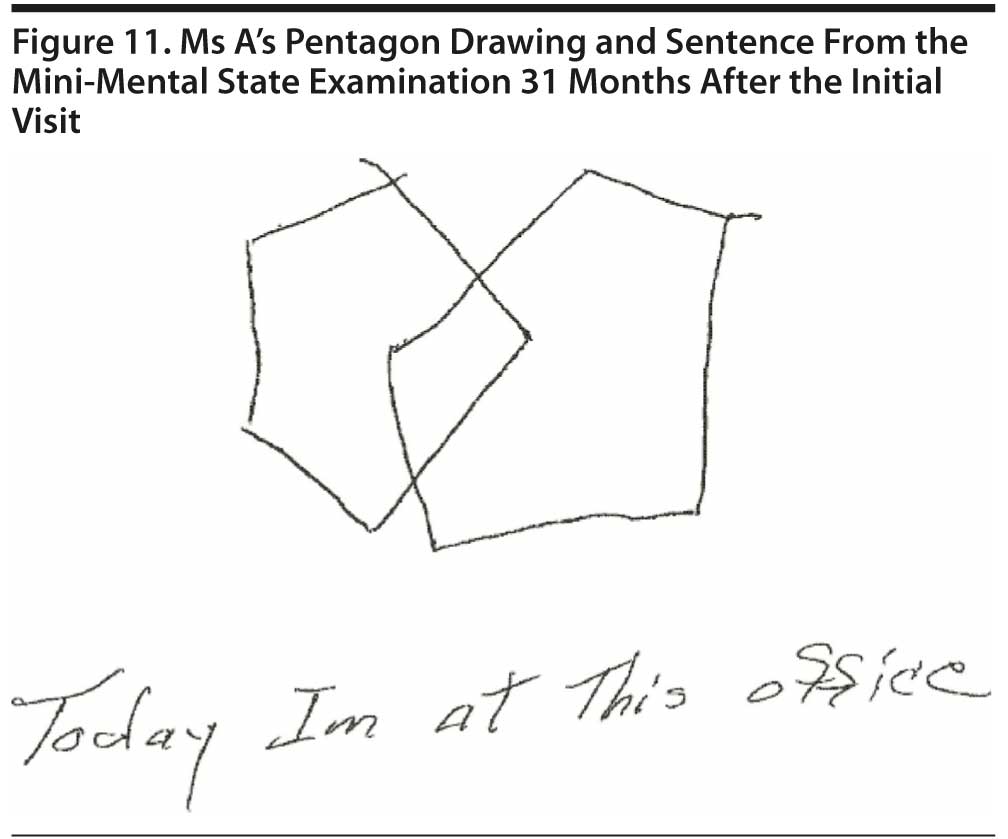
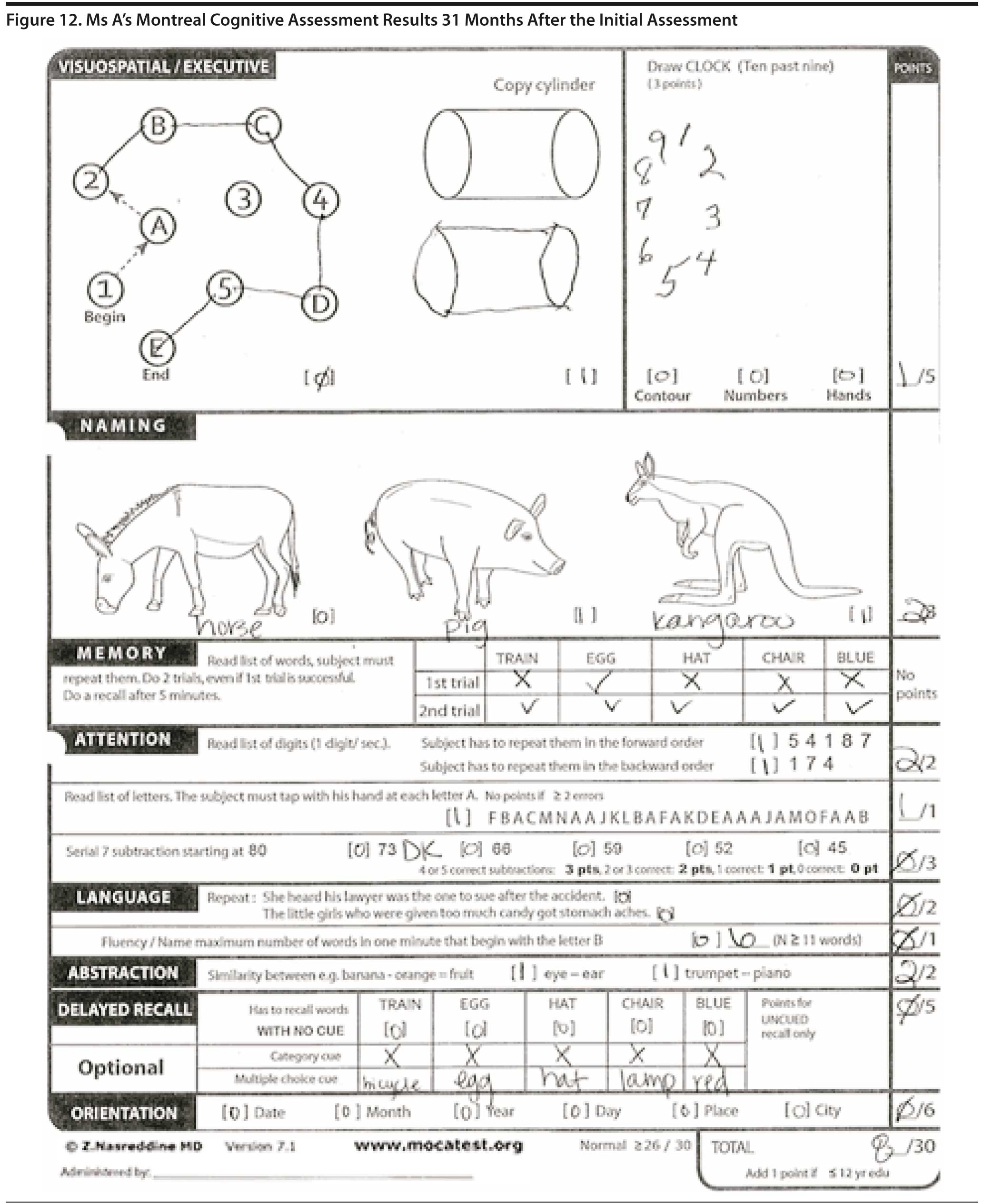
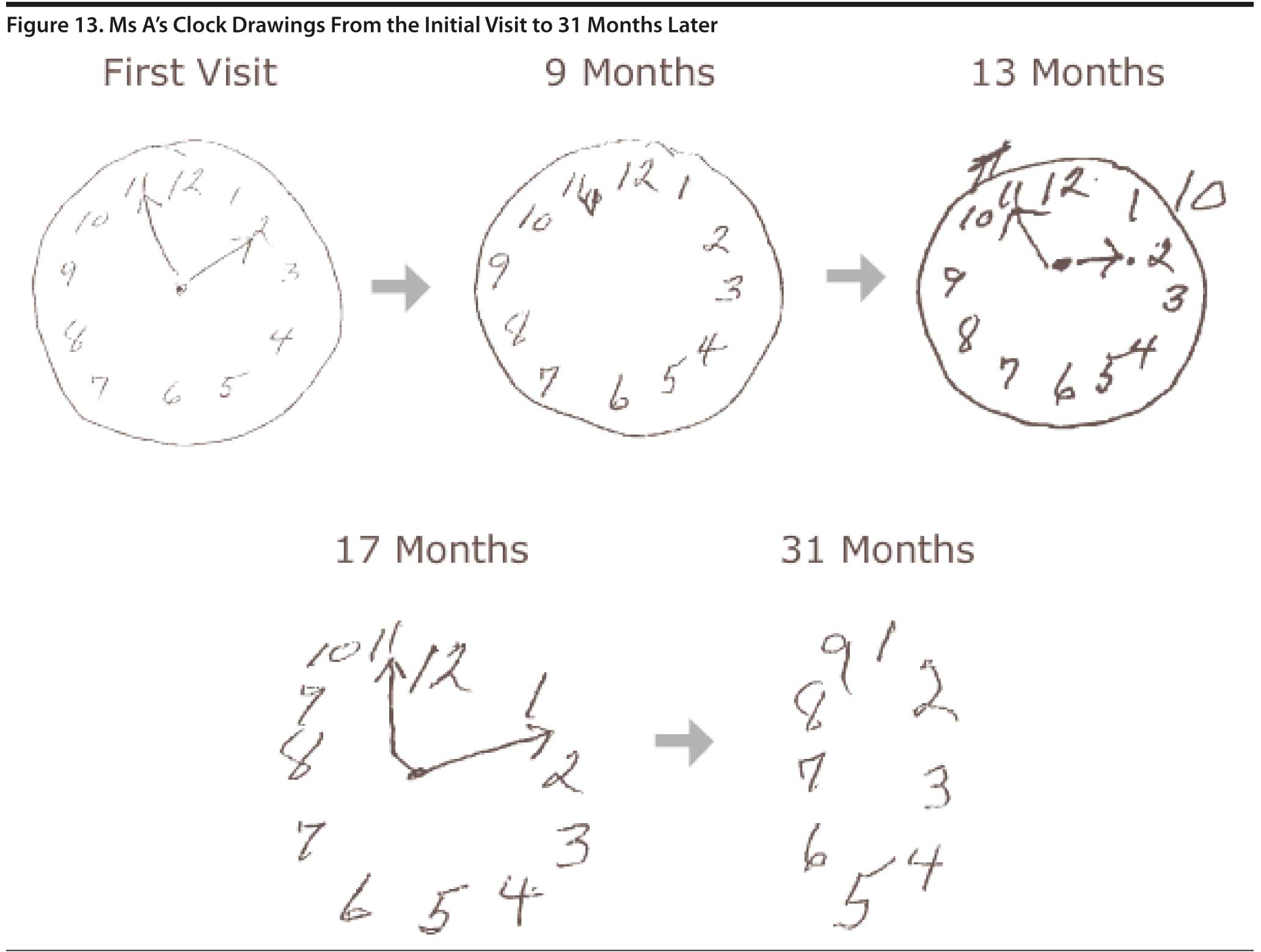
Ms A has continued progressive cognitive decline. She cannot recognize objects. She confuses the remote control and the telephone. She is unable to get items out of the refrigerator. The morning dose of quetiapine was discontinued. With quetiapine 50 mg at bedtime, behaviors are controlled with limited aggression, although she was quite irate about coming in to the “Alzheimer’s Institute” today. She scored 12 points on the MMSE and 8 points on the MoCA. Figure 11 shows Ms A’s pentagon drawing and sentence from the MMSE. Figure 12 shows Ms A’s MoCA results. Figure 13 shows Ms A’s clock drawings from the first visit to 31 months later.
IMPRESSION
Ms A is an 82-year-old woman in the moderate-to-severe stages of Alzheimer’s disease dementia. She has been having a relatively rapid progression of symptoms. She has had significant behavioral issues and agitation, which are currently well controlled on her current medication regimen. Ms A becomes very irate when coming to our Institute, and the term Alzheimer’s disease is not to be used with her.
PLAN
1. Continue transdermal rivastigmine 9.5 mg daily.
2. Continue quetiapine 50 mg at bedtime, with an additional 25-50 mg as needed daily.
3. Continue citalopram 20 mg daily.
4. Ms A will follow up in approximately 1 year. The cognitive testing will not be repeated at that time, given that it creates significant anger in this patient.
FINANCIAL DISCLOSURE
Dr Yaari is a consultant for Amedisys Home Health. Dr Tariot has served as a consultant for Abbott, AC Immune, Adamas, Avanir, Boehringer-Ingelheim, Chase, Chiesi, Eisai, Elan, MedAvante, Merz, Neuroptix, Otsuka, and Sanofi-Aventis; has received consulting fees and research support from AstraZeneca, Avid, Bristol-Myers Squibb, Eli Lilly, Genentech, GlaxoSmithKline, Janssen, Medivation, Merck, Pfizer, Roche, and Toyama; has received research support only from Baxter, Functional Neuromodulation, GE, and Targacept; has received other research support from Alzheimer’s Association, Arizona Department of Health Services, National Institute of Mental Health, and National Institute on Aging; is a stock shareholder in Adamas; and is listed as a contributor to a patent owned by the University of Rochester (Rochester, New York) for “Biomarkers of Alzheimer’s Disease.” Drs Hall, Fleisher, and Seward and Mss Brand and Dougherty have no personal affiliations or financial relationships with any commercial interest to disclose relative to the activity.
FUNDING/SUPPORT
None reported.
CASE CONFERENCE
The Banner Alzheimer’s Institute Case Conference is a weekly event in which physicians and staff discuss challenging and/or teaching cases of patients seen at the Institute’s Stead Family Memory Clinic. These conferences are attended by a multidisciplinary group that includes Banner Alzheimer’s Institute dementia specialists, community physicians (internal medicine, family medicine, and radiology), physician assistants, social workers, nurses, medical students, residents, and fellows.
DISCLAIMER
The opinions expressed are those of the authors, not of Banner Health or Physicians Postgraduate Press, Inc.
Disclosure of off-label usage
The authors have determined that, to the best of their knowledge, quetiapine is not approved by the US Food and Drug Administration for behavioral management in dementia.
Clinical Points
- To improve the quality of life of those with dementia and of their caregivers, clinicians need to treat the symptoms that can be managed, as well as comorbid depression and agitation, and provide caregivers with management strategies.
- Medication management of behavioral manifestations of dementia is often beneficial.
- Caregiver counseling and support is a vital part of treating behavioral manifestations of dementia.
This CME activity is expired. For more CME activities, visit cme.psychiatrist.com.
Find more articles on this and other psychiatry and CNS topics:
The Journal of Clinical Psychiatry
The Primary Care Companion for CNS Disorders
REFERENCES
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington, VA: American Psychiatric Association; 2000.
Farlow MR, Miller ML, Pejovic V. Treatment options in Alzheimer’s disease: maximizing benefit, managing expectations. Dement Geriatr Cogn Disord. 2008;25(5):408-422. doi:10.1159/000122962 PubMed
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. doi:10.1016/0022-3956(75)90026-6 PubMed
Iverson DJ, Gronseth GS, Reger MA, et al; Quality Standards Subcommittee of the American Academy of Neurology. Practice parameter update: evaluation and management of driving risk in dementia: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010 Apr 20;74(16):1316-1324. doi: 10.1212/WNL.0b013e3181da3b0f PubMed
Johns EK, Phillips NA, Chertkow H, et al. The effect of education on performance on the Montreal Cognitive Assessment (MoCA): normative data from the community. Canadian J Geriatrics. 2008:11(1):62.
Johns EK, Phillips NA, Chertkow H, et al. The Montreal Cognitive Assessment: normative data in the community. J International Neuropsychological Society. 2008;41(suppl 1):58. doi: http://dx.doi.org/10.1017/S1355617708080429
Knopman DS, DeKosky ST, Cummings JL, et al. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Practice parameter: diagnosis of dementia (an evidence-based review). Neurology. 2001;56(9):1143-1153. doi:10.1212/WNL.56.9.1143 PubMed
Links KA, Merims D, Binns MA, et al. Prevalence of primitive reflexes and Parkinsonian signs in dementia. Can J Neurol Sci. 2010;37(5):601-607. PubMed
Mungas D. In-office mental status testing: a practical guide. Geriatrics. 1991;46(7):54-58, 63, 66. PubMed
Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-699. doi:10.1111/j.1532-5415.2005.53221.x PubMed
Sudo K, Mito Y, Tajima Y, et al. Smooth-pursuit eye movement: a convenient bedside indicator for evaluating frontal lobe and intellectual function. In Vivo. 2010;24(5):795-797. PubMed
Tariot PN, Farlow MR, Grossberg GT, et al; Memantine Study Group. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA. 2004;291(3):317-324. doi:10.1001/jama.291.3.317 PubMed
US Food and Drug Administration. Deaths With Antipsychotics in Elderly Patients With Behavioral Disturbances. April 11, 2005. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm053171.htm?utm_campaign=Google2&utm_source=fdaSearch&utm_medium=website&utm_term=Deaths With Antipsychotics in Elderly Patients With Behavioral Disturbances 2008&utm_content=1. Accessed May 23, 2012.
Please sign in or purchase this PDF for $40.00.
Save
Cite