Capgras syndrome (CS) is a delusion of misidentification that occurs when a patient believes an individual with whom the patient is familiar is no longer themselves.1 CS classically causes the patient to believe that the person has been replaced, misidentifying the person and substituting a similar individual with a different emotional connection. CS is historically rare and was initially thought to be precipitated only by psychodynamic causes; however, CS is now a known sequela of organic causes such as neurologic disorders and intracranial lesions.2
Case Report
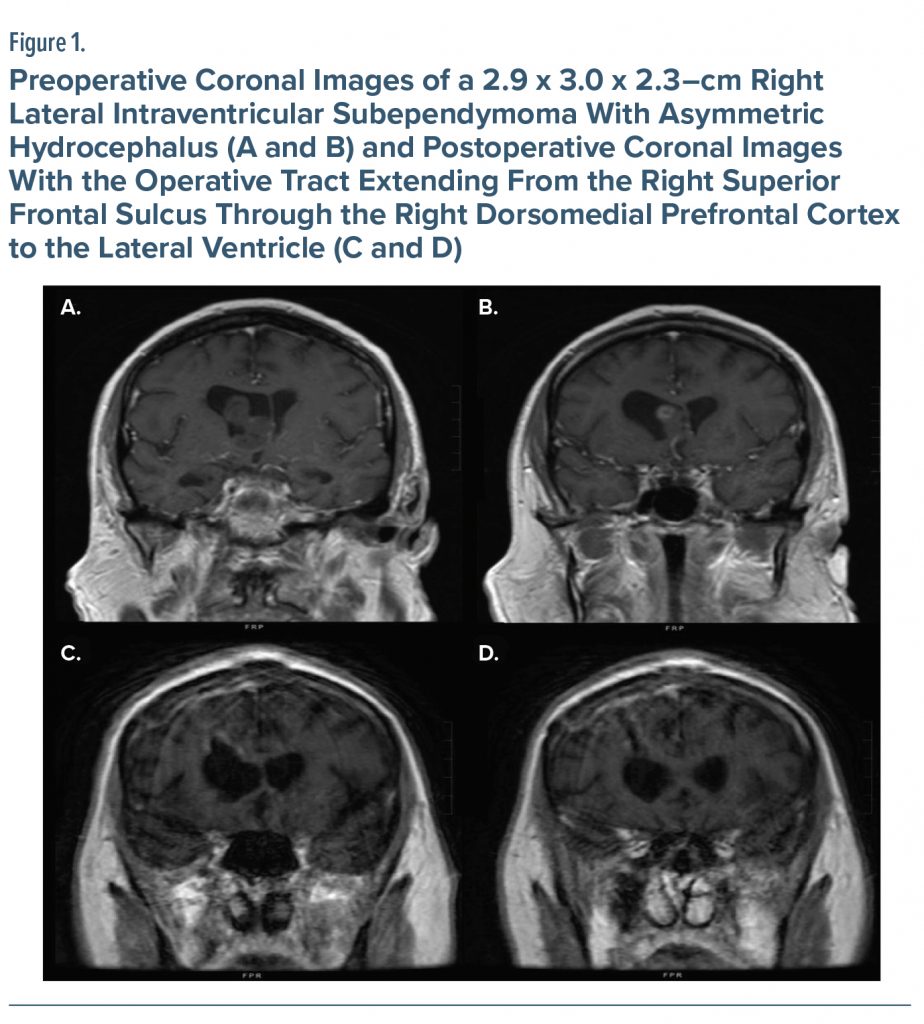
A 65-year-old White man with no history of psychiatric or substance use presented to the emergency department (ED) for evaluation of the incapability to recognize his fiancé. Due to a 2-year history of intermittent headaches, 28 days prior to admission, the patient underwent bifrontal craniotomy for excision of right lateral intraventricular subependymoma with asymmetric hydrocephalus, approached via right frontal horn (Figure 1). Head computed tomography; complete blood count; complete metabolic panel; thyroid function tests; vitamin B1, B9, and B12 levels; and infectious and toxicologic evaluation were all unremarkable. Notably, the patient’s fiancé remained with the patient after craniotomy and discharge. However, on the morning of the ED presentation, the patient believed that his fiancé had been replaced by her sister, and he called the police to report her missing. After his admission to the hospital, the psychiatry consultation team was consulted.
Table 12–4 includes details of the psychiatric evaluation with comparisons to the evidence base on CS. Notably, the patient’s mental status examination was unremarkable except for visual hallucinations and paranoid delusions. The patient was oriented × 2, while the Confusion Assessment Method5 was negative for presence of delirium. The patient scored a 53 and 22 on the Brief Psychiatric Rating Scale (BPRS)6 and Mini-Mental State Examination,7 respectively.
The neurosurgery department concluded that no new intracranial findings were present to cause CS. The patient began carbamazepine and brivaracetam after admission, and the psychiatry team added olanzapine. On days 7 and 10 of hospitalization, the patient’s BPRS scores were 42 and 38, respectively. The patient was discharged on hospital day 11 on carbamazepine, brivaracetam, and olanzapine. At follow-up 6 weeks later, the patient denied delusions of misidentification/CS, and his BPRS score was 21.
Discussion
CS is the most prevalent of the delusional misidentification syndromes. It appears in both psychiatric illness and medical/neurologic–based brain dysfunction.8 Toward this end, in a review of 260 case reports of delusional misidentification syndrome, approximately 70% had CS. The most common diagnoses included schizophrenia (73.0% of CS cases), dementia or other organic mental disorders (26.4%), and mood disorders (16.7%). Additionally, a CS prevalence of approximately 15.3% has been suggested among neurologic disorders, similar to risks among persons with major psychiatric disorders.9
While there is mixed evidence regarding lesions of a single brain region causing CS,10–12 our case supports frontal lobe involvement in CS.13,14 Specifically, during resection of our patient’s subependymoma, the superior frontal sulcus was microdissected, and corticotomy of white matter tracts at the base of the middle frontal gyrus was performed to approach the frontal horn for tumor excision. Postoperative imaging depicts this tract through the prefrontal cortex (see Table 1). We propose that chronic postsurgical changes in the latter may have had a role in the development of CS. More specifically, right frontal dysfunction has been associated with the pathological persistence of delusional beliefs after neurologic injuries.3 While our patient’s abnormal perception occurred from a disconnection between implicit and explicit facial processing, between visual facial perceptual areas and limbic structures or other unknown mechanisms, he certainly met criteria for CS.3 Fortunately, resolution of symptoms were noted at 6-week follow-up. Thus, while our case does not resolve the pathophysiology of CS, it does lend further support to a right hemispheric frontal lesion as partly causative.
Article Information
Published Online: November 7, 2023. https://doi.org/10.4088/PCC.23cr03524
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2023;25(6):23cr03524
Submitted: March 13, 2023; accepted June 7, 2023.
To Cite: Spiegel DR, Teixeira MN, Tracz JA, et al. Capgras syndrome after bifrontal craniotomy for excision of right lateral intraventricular subependymoma. Prim Care Companion CNS Disord. 2023;25(6):23cr03524.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk (all authors).
Corresponding Author: David R. Spiegel, MD, Department of Psychiatry and Behavior Sciences, Eastern Virginia Medical School, 825 Fairfax Avenue, Norfolk, Virginia 23507 ([email protected]).
Relevant Financial Relationships: Dr Spiegel is in the Speaker’s Bureau for Allergen, Alkermes, Otsuka, and IntraCellular but has no conflict of interest in preparation of this manuscript. Dr Colangelo and Mss Teixeira and Tracz report no relevant financial relationships.
Funding/Support: None.
Patient Consent: Consent was verbally received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (14)

- Wise N. The Capgras delusion: an integrated approach. Phenomenol Cogn Sci. 2016;15(2):183–205. CrossRef
- Pandis C, Agrawal N, Poole N. Capgras’ delusion: a systematic review of 255 published cases. Psychopathology. 2019;52(3):161–173. PubMed CrossRef
- Darby R, Prasad S. Lesion-related delusional misidentification syndromes: a comprehensive review of reported cases. J Neuropsychiatry Clin Neurosci. 2016;28(3):217–222. PubMed CrossRef
- Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225–235. PubMed CrossRef
- Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. a new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948. PubMed CrossRef
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10(3):799–812. CrossRef
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. PubMed CrossRef
- Hillers Rodríguez R, Madoz-Gúrpide A, Tirapu Ustárroz J. Propuesta de una batería neuropsicológica para la exploración del síndrome de Capgras. (Capgras syndrome: a proposal of neuropsychological battery for assessment) Rev Esp Geriatr Gerontol. 2011;46(5):275–280. PubMed CrossRef
- Salvatore P, Bhuvaneswar C, Tohen M, et al. Capgras syndrome in first-episode psychotic disorders. Psychopathology. 2014;47(4):261–269. PubMed CrossRef
- Christodoulou GN. The syndrome of Capgras. Br J Psychiatry. 1977;130(6):556–564. PubMed CrossRef
- Darby RR, Laganiere S, Pascual-Leone A, et al. Finding the imposter: brain connectivity of lesions causing delusional misidentifications. Brain. 2017;140(2):497–507. PubMed CrossRef
- Luca M, Bordone A, Luca A, et al. Clinical features and imaging findings in a case of Capgras syndrome. Neuropsychiatr Dis Treat. 2013;9:1095–1099. PubMed
- Jedidi H, Daury N, Capa R, et al. Brain metabolic dysfunction in capgras delusion during alzheimer’s disease: a positron emission tomography study. Am J Alzheimers Dis Other Demen. 2015;30(7):699–706. PubMed CrossRef
- Garcha M, Sivakumar K, Leary M, et al. Transient Capgras syndrome secondary to bilateral Ischemic stroke: a case report. Cogn Behav Neurol. 2018;31(2):96–98. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite