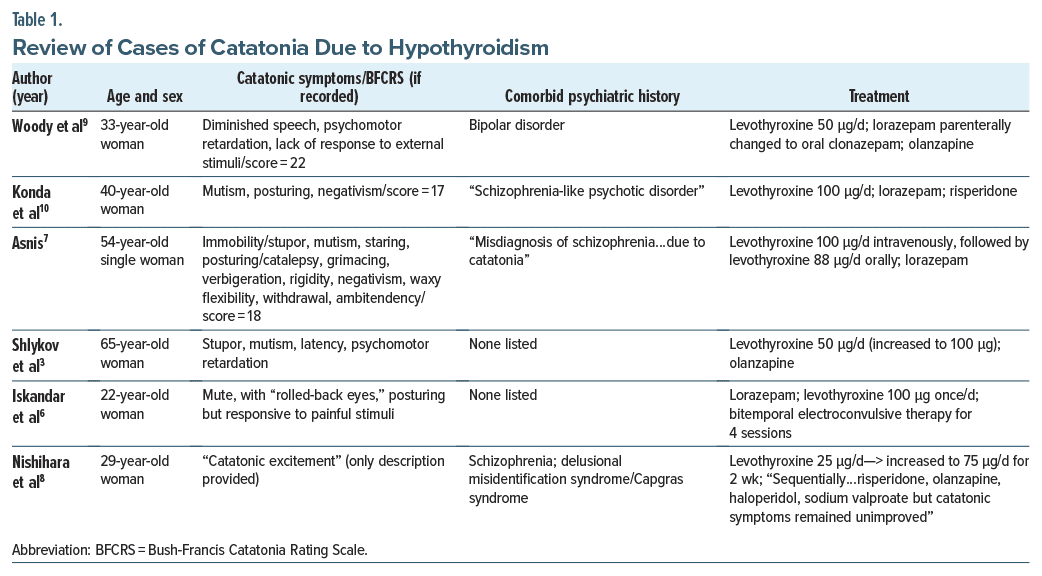
The association of mood disorders, including bipolar disorder, and thyroid dysfunction is well established. Conversely, while a spectrum of psychiatric symptoms has been noted in autoimmune thyroiditis,1 including the uncommon but well known myxedema madness/ hypothyroidism-related psychosis,2 there is a dearth in the literature of catatonia associated with thyroid conditions3–5 and more specifically, hypothyroidism (Table 1).3,6–10 As such, we present a case of catatonia in the context of a patient with nonadherence to thyroxine who developed severe hypothyroidism.
Case Report
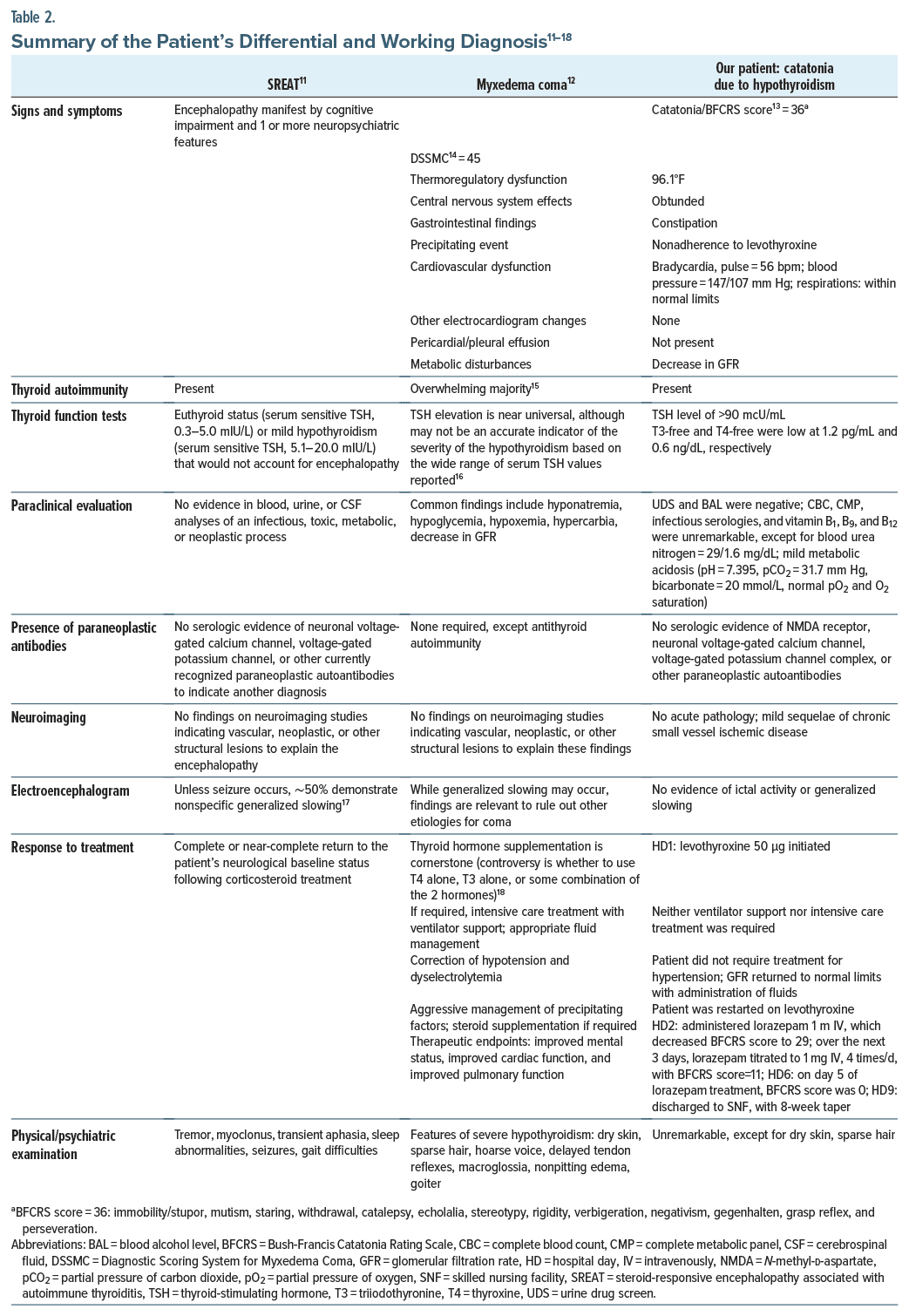
A 72-year-old woman with a medical history of hypercholesterolemia and hypothyroidism, prescribed atorvastatin and levothyroxine 100 μg/day, respectively, was brought to the emergency department by family due to failure to thrive and impaired mentation. Her family reported that, over the last 3 months, the patient had developed dysphagia, leading to poor oral intake and ∼10-lb weight loss, resulting in nonadherence to levothyroxine. The patient was admitted to the hospital for mild acute kidney injury/metabolic acidosis. After the latter was treated and the patient was started on levothyroxine 50 μg/day, we were consulted due to continued “altered mental status.” For a summary of the patient’s evaluation, assessment, and treatment, see Table 2.11–18
In brief, during the aforementioned 3-month period, the patient developed symptoms of catatonia and scored 36 on the Bush-Francis Catatonia Rating Scale (BFCRS).13 While the patient was unable to give a cogent history, she had no reported psychiatric or substance use history, with both blood alcohol and urine drug screen being negative. Lorazepam was given with immediate effect and more sustained effect within 3–5 days. There was no recurrence of catatonia on a tapering dose of lorazepam over the next 8 weeks.
Discussion
Our patient’s presentation warranted an exploration of several diagnoses, including steroid responsive encephalopathy associated with autoimmune thyroiditis (SREAT), myxedema coma, and catatonia due to hypothyroidism. See Table 2 for a review of our working and differential diagnosis for the patient.
On a recently developed scale evaluating myxedema coma,14 our patient scored 45. On this scale, a diagnostic score ≥60 is consistent with myxedema coma, whereas a score between 45 and 59 is consistent with only overt hypothyroidism but at increased risk for myxedema coma if not treated. As per Table 2, our patient did have symptoms of myxedema coma, although when combined with her psychomotor abnormalities on the BFCRS and her relatively rapid and complete response to lorazepam, myxedema coma seemed much less likely at the time of our evaluation. As a caveat, patients may not initially present with frank coma but with milder signs of depressed mental status, only to gradually decline to a coma subsequently.18 Lastly, while thyroid autoimmunity and neuropsychiatric symptoms are present in both patients with SREAT and our patient, the latter presented with a significant elevation of thyroid stimulating hormone (TSH), low triiodothyronine (T3)/thyroxine (T4) levels, no seizures, and again, a relatively prompt and thorough response to lorazepam—all not consistent with SREAT. Alternatively, about 95%–98% of patients with SREAT demonstrate an improvement/complete resolution of symptoms after immunosuppressive therapy.19
Due to the limited evidence base, few conclusions can be garnered from our patient, although TSH levels (due to hypothyroidism) associated with catatonia have been reported to range from as little as 10.78 μIU/mL10 to >100 µIU/mL,3 with our patient’s TSH level >90 µIU/mL. Nonetheless, it appears that the extent of thyroid dysfunction does not necessarily correlate with the degree of accompanying psychiatric manifestations.20 Additionally, previously reported patients’ catatonia responded to both lorazepam (as in our patient) and electroconvulsive therapy.3–10
Notably, we felt in our patient that lorazepam therapy was primarily responsible for the improvement/ resolution in catatonia. That is, in hypothyroidism-induced psychiatric symptoms, including in our patient, while thyroid replacement remains the gold standard in treatment, even with proper replacement, symptoms may take several months to abate.2
Alternatively, while not evaluated systematically, there have been reports of using loading dose levothyroxine combined with antipsychotic medication to more rapidly treat myxedema psychosis. Traditionally, loading doses were mainly reserved in the setting of myxedema coma, as the former requires a need for a rapid response within days. Similar benefits have also been described of using loading dose levothyroxine for more rapid attentuation of manic and/or psychotic symptoms. In 1 report,21 a 44-year-old woman was prescribed loading dose levothyroxine 300 μg daily for 1 week and 100 μg daily thereafter combined with adjunctive olanzapine. This resulted in rapid improvement of psychotic symptoms within 4 days. The described rationale was to establish a therapeutic levothyroxine level over a few days prior to continuing with maintenance dosing. Notably, olanzapine was utilized for a total of 4 weeks, from admission until after discharge. Limitations to this method include, to the best of our knowledge, that it has not been used in catatonia associated with hypothyroidism. Furthermore, this method should likely not be considered in the elderly or those with ischemic heart disease, as the increased myocardial oxygen demand that levothyroxine stimulates may trigger myocardial infarction, arrhythmias, or heart failure. Toward this end, in the case study,21 there was no evidence of cardiac dysfunction on electrocardiogram and chest x-ray prior to or 4 days after initiating loading dose levothyroxine.
Finally, biochemical changes associated with catatonia mainly focus on γ-aminobutyric acid (GABA)ergic, glutamatergic, and dopaminergic transmission.22 While beyond the scope of this report of the pathophysiology of how hypothyroidism can lead to catatonia, thyroid hormone has been shown to be a key factor for the induction and function of dopaminergic neurons. Thyroid hormone deficiency has been reported to lead to a decrease in the number and function of mesencephalic dopaminergic neurons,23 a known potential precipitant for catatonia. Intriguingly, a study24 demonstrated reduced GABA concentrations among hypothyroid patients and an increase in GABA concentrations after 6-month treatment with levothyroxine. In conclusion, we endorse that future research should be undertaken to further elucidate the potential relationship between hypothyroidism and catatonia.
Article Information
Published Online: August 1, 2024. https://doi.org/10.4088/PCC.23cr03700
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(4):23cr03700
Submitted: January 4, 2024; accepted March 26, 2024.
To Cite: Spiegel DR, Jahelka C, Shelton M, et al. A case and differential diagnosis of catatonia in a patient with hypothyroidism due to levothyroxine nonadherence. Prim Care Companion CNS Disord. 2024;26(4):23cr03700.
Author Affiliation: Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, Virginia (all authors).
Corresponding Author: David R. Spiegel, MD, Department of Psychiatry and Behavior Sciences, Eastern Virginia Medical School, 825 Fairfax Ave, Norfolk, Virginia 23507 ([email protected]).
Relevant Financial Relationships: Dr Spiegel is in the speaker’s bureau for Allergen, Alkermes, Otsuka, and IntraCellular but has no conflicts of interest in preparation of this manuscript. The remainder of the authors have no disclaimer/conflicts of interest to report.
Funding/Support: None.
Patient Consent: Consent was verbally received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (24)

- Johnson ET, Eraly SG, Aandi Subramaniyam B, et al. Complexities of cooccurrence of catatonia and autoimmune thyroiditis in bipolar disorder: a case series and selective review. Brain Behav Immun Health. 2022;22:100440. PubMed CrossRef
- Leal JC, Beito AH. Ramifications of untreated hypothyroidism: case report of cognitive impairment and acute psychosis in an elderly female. Ann Gen Psychiatry. 2020;19:48. PubMed CrossRef
- Shlykov MA, Rath S, Badger A, et al. Myxoedema madness’ with Capgras syndrome and catatonic features responsive to combination olanzapine and levothyroxine. BMJ Case Rep. 2016;2016:bcr2016215957. PubMed CrossRef
- Lalanne L, Meriot ME, Ruppert E, et al. Attempted infanticide and suicide inaugurating catatonia associated with Hashimoto’s encephalopathy: a case report. BMC Psychiatry. 2016;16:13. PubMed CrossRef
- Chen YW, Hung PL, Wu CK, et al. Severe complication of catatonia in a young patient with Hashimoto’s encephalopathy comorbid with Cornelia de Lange syndrome. Kaohsiung J Med Sci. 2015;31(1):60–61. PubMed CrossRef
- Iskandar M, Stepanova E, Francis A. Two cases of catatonia with thyroid dysfunction. Psychosomatics. 2014;55(6):703–707. PubMed CrossRef
- Asnis GM. Catatonia secondary to hypothyroidism may be very responsive to electroconvulsive therapy: a case study. J ECT. 2020;36(4):e46–e47. PubMed CrossRef
- Nishihara K, Kinoshita H, Kurotaki N, et al. Could subclinical hypothyroidism cause periodic catatonia with delusional misidentification syndrome? Psychiatry Clin Neurosci. 2010;64(3):338. PubMed CrossRef
- Woody DM, Chen C, Parker J. Catatonia in a patient with bipolar affective disorder and hypothyroidism: a diagnostic and therapeutic challenge. Cureus. 2023;15(10):e46989. PubMed CrossRef
- Konda PR, Reddy S, Gunde S. A rare case of recurrent psychosis with hypothyroidism precipitating catatonia. Telangana J Psychiatry. 2023;9(1):63–65.
- Castillo P, Woodruff B, Caselli R, et al. Steroid responsive encephalopathy associated with autoimmune thyroiditis. Arch Neurol. 2006;63(2):197–202. PubMed CrossRef
- Mathew V, Misgar RA, Ghosh S, et al. Myxedema coma: a new look into an old crisis. J Thyroid Res. 2011;2011:493462. PubMed CrossRef
- Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129–136. PubMed CrossRef
- Popoveniuc G, Chandra T, Sud A, et al. A diagnostic scoring system for myxedema coma. Endocr Pract. 2014;20(8):808–817. PubMed CrossRef
- Ylli D, Klubo-Gwiezdzinska J, Wartofsky L. Thyroid emergencies. Pol Arch Intern Med. 2019;129(7–8):526–534. PubMed CrossRef
- Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670–1751. PubMed CrossRef
- Endres D, Maier V, Leypoldt F, et al. Autoantibody associated psychiatric syndromes: a systematic literature review resulting in 145 cases. Psychol Med. 2022;52(6):1135–1146. PubMed CrossRef
- Ishii M. Endocrine emergencies with neurologic manifestations. Continuum (Minneap Minn). 2017;23(3, Neurology of Systemic Disease):778–801. PubMed CrossRef
- Waliszewska-Prosół M, Ejma M. Hashimoto encephalopathy-still more questions than answers. Cells. 2022;11(18):2873. PubMed
- Sardar S, Habib MB, Sukik A, et al. Myxedema psychosis: neuropsychiatric manifestations and rhabdomyolysis unmasking hypothyroidism. Case Rep Psychiatry. 2020;2020:7801953. PubMed CrossRef
- Gupta A, Bastiampillai T, Disha TI, et al. Rapid response to loading dose levothyroxine in myxedema psychosis. Prim Care Companion CNS Disord. 2017;19(1):16101974.
- Hirjak D, Kubera KM, Wolf RC, et al. Going back to kahlbaum’s psychomotor (and GABAergic) origins: is catatonia more than just a motor and dopaminergic syndrome? Schizophr Bull. 2020;46(2):272–285. PubMed CrossRef
- Charoenngam N, Rittiphairoj T, Ponvilawan B, et al. Thyroid dysfunction and risk of Parkinson’s disease: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2022;13:863281. PubMed CrossRef
- Liu B, Wang Z, Lin L, et al. Brain GABA+ changes in primary hypothyroidism patients before and after levothyroxine treatment: a longitudinal magnetic resonance spectroscopy study. Neuroimage Clin. 2020;28:102473. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite