Prim Care Companion CNS Disord 2023;25(3):22cr03409
To cite: Bachu AK, Bachu R, Mousa H, et al. Causes of cognitive decline and dementia in a young patient. Prim Care Companion CNS Disord. 2023;25(3):22cr03409.
To share: https://doi.org/10.4088/PCC.22cr03409
© 2023 Physicians Postgraduate Press, Inc.
aBaptist Health-UAMS North Little Rock, Arkansas
bNorthpointe Psychiatry, Lewisville, Texas
*Corresponding authors: Sahar Ashraf, MD, Northpointe Psychiatry, 860 Hebron Pkwy, Ste 1101, Lewisville, TX 75057 ([email protected]); Anil K. Bachu, MD, Department of Behavioral Health, Baptist Health, 3500 Springhill Dr, North Little Rock, AR 72117 ([email protected]).
Dementia is an acquired decline in cognition in multiple cognitive domains sufficiently severe to affect social or occupational function.1 The number of cases of infectious syphilis in the United States has steadily increased since 2000. Neurosyphilis is a serious complication of syphilis that can develop 10–25 years after the onset of the infection and present with neurologic symptoms including general paresis, tabes dorsalis, and dementia. If left untreated, it can lead to irreversible neuronal damage.2 Alzheimer’s disease is the most common form of dementia, accounting for about 50% to 60% of all dementia, followed by vascular dementia, frontotemporal lobar dementia, dementia with Lewy bodies, and Parkinson’s disease dementia.3
Case Report
A 50-year-old Black man with a history of hypertension (he was not compliant with medications), hyperlipidemia, prediabetes, depression, PCP (phencyclidine) abuse, and tobacco use disorder presented to our clinic with progressive cognitive and functional decline, memory problems, falls, personality and behavioral changes, depressed mood, apathy, anhedonia, belligerence, hyperphagia, hypersomnia, and poor self-care.
He was treated for depression by his primary care physician for 2 years with no improvement in functional status. The patient was dependent for most activities of daily living and instrumental activities of daily living. Discussion with his mother revealed that he had an episode of hypertensive emergency in 2018. There was no history of cerebrovascular accidents or HIV infection. Lately, his father had noticed that the patient was urinating and passing stools on himself, having multiple falls, getting lost in the neighborhood, and having behavioral tantrums.
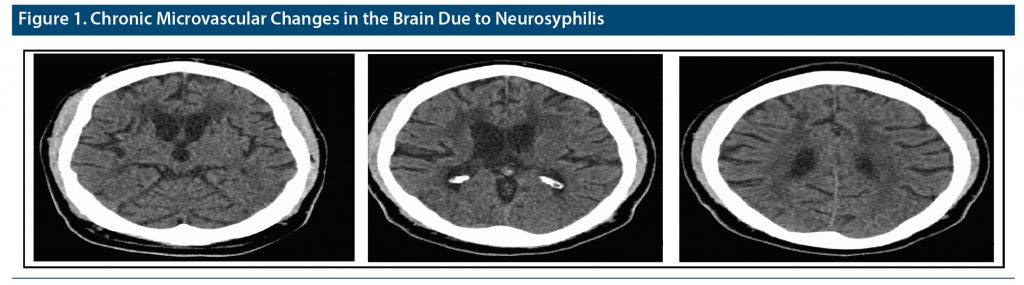
On examination, the patient was apathetic, alert, oriented in all spheres, and slow in responding to questions. His Montreal Cognitive Assessment4 score was 14–15/30, and his Mini-Mental State Examination5 score was 15. He had a grossly abnormal gait pattern, slowed and wide based on reduced arm swing. His pupils showed normal reactivity to light and accommodation. Laboratory studies for dementia were unremarkable except for reactive rapid plasma reagin and a positive fluorescent treponemal antibody–absorption test (FTA-ABS) test. He had a history of syphilis in 1996 and was treated with antibiotics. Computed tomography of the head showed chronic microvascular changes more than typical for his age (Figure 1). Lumbar puncture showed nonreactive cerebrospinal fluid (CSF) venereal disease research laboratory test (VDRL) but with an elevated protein of 51, suggesting neurosyphilis.
The patient was sent to an infectious disease specialist, and he received a 14-day course of intravenous penicillin G. A month later, he returned to the clinic with reported good blood pressure control, and his father described an improvement in behavioral issues, especially belligerence after treatment with paroxetine, but no improvement in cognitive deficits and function. A social worker was added to the treatment team to avoid nursing home placement.
Discussion
In this case, a young patient with progressive cognitive decline was treated for possible neurosyphilis. PCP use and chronic hypertension could also have contributed to his cognitive decline. Cognitive decline differential diagnosis at a young age is a wide and timely diagnosis, and treatment can prevent irreversible damage. Fifty million people live with dementia around the world, and this number is expected to increase to 152 million by 2050.1 Reflecting on our patient, most likely he had multifactorial dementia. Factors supporting the diagnosis of vascular dementia are the history of hypertension (noncompliance with medications leading to hypertensive emergencies in the past), progressive deterioration in mental status, abnormal neurologic signs, and extensive ischemic changes on a magnetic resonance imaging scan. Others include neurosyphilis from lumbar puncture findings and PCP use for more than 30 years as an adjuvant factor.
Early-onset dementia is common and is diagnosed in one-third of patients with a diagnosis of dementia. The differential diagnosis could be challenging due to the many causes involved. Some causes are treatable, so timely diagnosis is crucial. Thus, a systematic approach to early diagnosis and treatment is warranted to prevent cognitive decline and loss of function.6 The younger a person is, the more likely genetics (familial history) are the cause of early-onset dementia. Alzheimer’s disease, vascular disease, frontotemporal dementia, and dementia with Lewy bodies are other common causes of dementia. Neurosyphilis, a common cause of dementia in the past, is now a rare condition in developed countries, but cases continue to be reported, leading to progressive cognitive decline with or without psychiatric features.2 Starting with memory decline and personality changes, the patient shows a continued decline in memory, as well as depression, mania, or psychosis. A neurologic examination is normal in the initial stage of the disease.2 Untreated neurosyphilis can potentially lead to irreversible sequela.7 Syphilis is a reportable disease in the United States. Primary and secondary syphilis cases have been on the rise since 2000. It is more prevalent in men, and 75% of infected men are homosexual. Half of these men are also infected with HIV.8
Potentially reversible etiologies including inflammatory disorders, infectious diseases, toxic/metabolic abnormalities, transient epileptic amnesia, obstructive sleep apnea, and normal pressure hydrocephalus also represent important differential diagnostic considerations in young-onset dementia.9 A negative VDRL should not suggest negative disease due to low sensitivity, and confirmation is prompted by the CSF FTA-ABS test. A major effect of PCP use occurs in the frontal and prefrontal cortex of the brain. Long-term use of PCP is associated with attention deficit, aggressiveness and violent behaviors, psychosis, depression, long-term cognition, and memory loss.10
Despite our patient receiving therapy for neurosyphilis, he only showed mild improvement according to his father. He will need further follow-up at 3, 6, and 12 months with lumbar puncture and imaging. Without a doubt, education and social and psychological support are essential for family members of dementia patients.
Conclusions
Neurosyphilis should be part of the differential diagnosis of patients showing cognitive deterioration and behavioral disturbances. Physicians need to be diligent regarding the recognition of risk factors of vascular dementia and vigorous management. Substance use history should be part of the dementia workup.
Published online: June 6, 2023.
Relevant financial relationships: None.
Funding/support: None.
Additional information: Information has been de-identified to protect anonymity.
References (10)

- Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of dementia: review. JAMA. 2019;322(16):1589–1599. PubMed CrossRef
- Marra CM. Neurosyphilis. Continuum (Minneap Minn). 2015;21(6 Neuroinfectious Disease):1714–1728. PubMed
- Mahalingam S, Chen MK. Neuroimaging in Dementias. Semin Neurol. 2019;39(2):188–199. PubMed CrossRef
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. PubMed CrossRef
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. PubMed CrossRef
- Fadil H, Borazanci A, Ait Ben Haddou E, et al. Early onset dementia. Int Rev Neurobiol. 2009;84:245–262. PubMed CrossRef
- Ha T, Tadi P, Dubensky L. Neurosyphilis. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2021.
- Centers for Disease Control and Prevention, Department of STD Prevention. CDC website. Sexually transmitted disease surveillance. Published December 2014. Accessed March 15, 2023. www.cdc.gov/std/stats13/surv2013-print.pdf
- Kuruppu DK, Matthews BR. Young-onset dementia. Semin Neurol. 2013;33(4):365–385. PubMed CrossRef
- The dangers of PCP. Oxford Treatment Center website. Accessed March 15, 2023. https://oxfordtreatment.com/substance-abuse/pcp/
Please sign in or purchase this PDF for $40.
Save
Cite