Catatonia comprises a neuropsychiatric syndrome characterized by altered psychomotor and behavioral symptoms, as well as autonomic dysfunction.1,2 Catatonia is currently classified in the DSM-5 as a possible specifier of a psychotic, affective, neurologic, or other medical condition or unknown cause (idiopathic).3 Here, we present a case of an inpatient with catatonic schizophrenia with multiple systemic repercussions and complex etiology.
Case Report
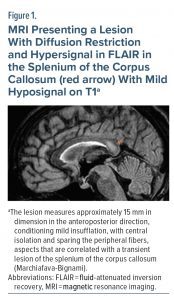
In February 2018, a 23-year-old male university student was admitted to the hospital to undergo electroconvulsive therapy (ECT). The patient presented with mutism, and the main sources for history taking were family members and his clinical reports. He had a 2-year progressive onset of diverse symptoms not consistently described until he experienced full-blown catatonia. The following remarks were included in his clinical report: “catatonic stupor, with psychomotor inhibition, selective mutism, negativism, active resistance to feeding with significant weight loss and insomnia . . . affective indifference and sitophobia.” He had been fed with a permanent nasogastric tube for 8 months at the time of admission. During the previous admission, psychotropic medications with benzodiazepines, antidepressants, antipsychotics, and mood stabilizers were tried. The examinations at admission showed no important alterations. At admission to our unit, he looked emaciated and was uncooperative with avoidant contact, staying silent with negativism and mitgehen (an observation finding consisting of the examiner being able to move the patient’s body with the slightest touch). He scored 12 + 3 on the Bush-Francis Catatonia Rating Scale.4 The clinical examination showed a lesion in the corpus callosum splenium compatible with Marchiafava-Bignami syndrome (Figure 1) and malnutrition. No other relevant alterations were found on extensive blood, urine, and cerebrospinal fluid tests (including N-methyl-d-aspartate antibodies).
Based on the history provided by the family, the medical team first considered an affective episode as the underlying disorder, and ECT (total of 18 sessions) and lorazepam titrated to 15 mg/d and venlafaxine titrated to 225 mg/d were started. The nasogastric tube feeding was optimized. Due to the sparse response and later clarification of symptomatology as having a clearer psychotic undertone (schizophrenia with catatonic features), olanzapine was initiated and titrated to 15 mg/d, with haloperidol also being tried at a later stage. In time, the patient began to communicate through gestures and written language, started feeding by his own hands, and became more socially interactive, with remission of most psychomotor symptoms.
Due to an otolaryngologic intercurrence (possibly traumatic in nature and in temporal relation to nasogastric tube removal), he needed a tracheostomy. Therefore, his medications were temporarily reduced and ECT was suspended as a precaution. After therapeutic revision, he was started on clozapine and haloperidol and was discharged in November 2018 with clozapine 400 mg/d and intramuscular haloperidol 200 mg/month without psychomotricity changes. He had euthymic mood and was feeding autonomously, communicating in an unspoken manner (due to tracheostomy), and autonomous in his care.
It is vital to stress the importance of occupational therapy and the dedication of all members of the team during his treatment and care. The findings of Marchiafava-Bignami syndrome were reversed on the discharge magnetic resonance imaging scan. He currently presents no active psychotic or affective symptoms, although some cognitive symptoms remain, and takes clozapine 200 mg/d and haloperidol 200 mg/month. With time, it was possible to remove the tracheostomy, and he now speaks with no restrictions. The patient is now well integrated socially and started a job after directed training.
Discussion
Acute- and long-term catatonia share the initial treatment regimen of benzodiazepines and ECT, but chronic catatonia presents no clinical response and needs further treatment, with the management of nonpsychiatric causes prioritized.5–7 Long-term catatonic presentation in psychotic illness is usually associated with a worse prognosis, incomplete recovery, and several years of neuropsychiatric symptoms,2,6,8 but the treatment approach in this case was successful.
Article Information
Published Online: November 2, 2023. https://doi.org/10.4088/PCC.22cr03455
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2023;25(6):22cr03455
Submitted: December 22, 2022; accepted February 24, 2023.
To Cite: Rema JP, Cavaco T, Ferreira D, et al. Complex long-term catatonia. Prim Care Companion CNS Disord. 2023;25(6):22cr03455.
Author Affiliations: Psychiatry and Mental Health Service of the Neurosciences Department of Centro Hospitalar Universitário Lisboa Norte, Hospital Santa Maria, Lisbon, Portugal (Rema, Cavaco, Ferreira, Pereira); Clínica Universitária de Psiquiatria e Psicologia da Faculdade de Medicina da Universidade de Lisboa, Lisbon, Portugal (Rema, Ferreira); Hospital de Cascais, Alcabideche, Portugal (Rema).
Author Contributions: Drs Rema and Cavaco are first co-authors.
Corresponding Author: Diogo Ferreira, MD, Psychiatry and Mental Health Service of the Neurosciences Department of Centro Hospitalar Universitário Lisboa Norte, Hospital Santa Maria, Avenida Professor Egas Moniz 1649-035 Lisbon, Portugal ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: The case report was presented as a poster at the XVI Congresso Nacional de Psiquiatria; November 17–19, 2022; Algarve, Portugal.
ORCID: João P. Rema: https://orcid.org/0000-0002-2552-5175; Tânia Cavaco: https://orcid.org/0000-0002-9397-3025; João M. Pereira: https://orcid.org/0000-0001-5119-4210
Patient Consent: Consent was received from the patient to publish the case report, and information (including the dates) has been de-identified to protect anonymity.
References (8)

- Barnes MP, Saunders M, Walls TJ, et al. The syndrome of Karl Ludwig Kahlbaum. J Neurol Neurosurg Psychiatry. 1986;49(9):991–996. PubMed CrossRef
- Tandon R, Heckers S, Bustillo J, et al. Catatonia in DSM-5. Schizophr Res. 2013;150(1):26–30. PubMed CrossRef
- Bush G, Fink M, Petrides G, et al. Catatonia, I: rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129–136. PubMed CrossRef
- Rajagopal S. Catatonia. Adv Psychiatr Treat. 2007;13(1):51–59. CrossRef
- Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181. PubMed CrossRef
- Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6(4):391–398. PubMed CrossRef
- Burrow JP, Spurling BC, Marwaha R. Catatonia. In StatPearls. StatPearls Publishing; 2021.
- Burrow JP, Spurling BC, Marwaha R. Catatonia. In StatPearls. StatPearls Publishing; 2021.
Please sign in or purchase this PDF for $40.
Save
Cite