ABSTRACT
Objective: To examine sleep duration at admission and discharge and change in sleep duration during hospitalization in patients experiencing a manic episode and compare these parameters to patients hospitalized for major depressive disorder (MDD) during the same time frame. The correlation between sleep duration parameters in those with mania and MDD with length of hospital stay, after accounting for possible confounders, was also examined.
Methods: This retrospective study examined patients admitted to an acute care psychiatric unit from 2018 to 2021 with an episode of mania or MDD. Sleep duration was determined based on nursing observer report.
Results: The study included 41 patients with mania (32.9 ± 1.7 years) and 38 patients with MDD (32.7 ± 1.8 years). Mania patients had longer hospitalization and received higher antipsychotic and benzodiazepine doses, but fewer hypnotics (all P < .005). No differences were found in sleep duration at admission (P = .109) and discharge (P = .623) in the mania and MDD groups. Change in sleep duration was 1.14 ± 0.27 and 0.37 ± 0.28 hours (P = .05) in the groups, respectively. In those with mania, sleep duration at admission negatively correlated with length of stay (r = –0.033; P = .03). Sleep duration parameters were not correlated with length of stay in patients with MDD.
Conclusion: There was a trend toward greater improvement in sleep duration in inpatients with mania versus MDD. Sleep duration at admission correlated with length of hospitalization in patients with mania. Future studies should examine whether attempts to increase sleep duration can improve patient outcomes.
Prim Care Companion CNS Disord 2024;26(1):23m03620
Author affiliations are listed at the end of this article.
Bipolar disorder type I is a chronic illness consisting of both manic and depressive mood episodes. Bipolar disorder is a leading cause of disability worldwide.1 Epidemiological studies estimate the lifetime prevalence for bipolar disorder type I to be approximately 1%.2 Additionally, it is estimated that there is an incidence of bipolar mania of around 5 in 100,000 of population.3 Manic episodes, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, are characterized by distinct periods of abnormally and persistently elevated, expansive, or irritable mood.4 Furthermore, the mood disturbances are associated with increased goal-directed activity or energy lasting at least 1 week. Manic episodes are usually accompanied by a significantly reduced need for sleep. Evidence suggests that sleep disturbance escalates just prior to an episode of mania.5
Hospitalization is often necessary for the management of manic episodes. In hospitalized patients, sleep restoration typically occurs and precedes improvement of psychotic and manic symptoms.6 Previous research has shown that sleep duration on the day of admission can predict the rate of improvement in manic symptoms.7 In addition, sleep duration has also been shown to be associated with the level of cooperation and improvement in irritability.8 These prior investigations have not examined trends in sleep duration prior to discharge and its effect on length of hospitalization. Furthermore, the effects of benzodiazepines and sedative hypnotic medications as well as other potential confounders on sleep duration have not been accounted for.
In this study, we aimed to examine sleep duration at admission and discharge and change in sleep duration during hospitalization in patients experiencing a manic episode and compare these parameters to patients hospitalized for major depressive disorder (MDD) during the same time frame. We also examined the correlation between sleep duration parameters in those with mania and MDD with length of hospital stay after accounting for possible confounders.
METHODS
We retrospectively examined a cohort of patients who were admitted to the Acute Psychiatric Care Unit at Mayo Clinic, Rochester, Minnesota, from 2018 to 2021 with an episode of mania or MDD.
Sample
Only patients who provided prior written authorization allowing the use of their medical records for research purposes were included. The unit admits patients between the ages of 18 and 62 years with a primary psychiatric diagnosis requiring acute psychiatric stabilization. Voluntary status could be an effect modifier, as patients that are undergoing a commitment process could experience significantly prolonged hospitalization secondary to court dates, processing, and county-determined dispositions; therefore, patients who were under commitment were excluded. Patients in whom mania or MDD was not the primary diagnosis at the time of discharge were also excluded.
Sleep Data
We obtained information on sleep duration from nursing logs that recorded data at 15-minute intervals for safety checks. To reduce bias and account for possible outliers, sleep duration at admission for each patient was determined by averaging the total sleep time on the second and third days of admission and similarly for discharge by averaging the total sleep time on days 3 and 2 prior to discharge. We did not include the first or last night of the hospitalization, as sleep is often disrupted by the admission and discharge process, adjustment to a new environment, and other extraneous factors that may not be associated with the illness.
Additional Data
For each patient, we collected (1) antipsychotic doses in chlorpromazine equivalents, (2) benzodiazepine doses in diazepam equivalents (all benzodiazepines including those with specific US Food and Drug Administration (FDA) indications for insomnia were included in this category), (3) patient status as voluntary and involuntary (at any part of hospitalization), (4) sex, (5) age, (6) mood stabilizer use, (7) sedative hypnotic use (all FDA-approved hypnotic medications except benzodiazepines were included in this category; additionally, trazodone and melatonin, which are commonly used off-label as hypnotics in our inpatient setting, were included in this category), (8) comorbid substance use disorder, and (9) tobacco use from the electronic health record. We considered benzodiazepine and antipsychotic use as effect modifiers, as administration of these medications would likely increase sleep duration. We converted benzodiazepine and antipsychotic dosage into diazepam and chlorpromazine equivalents, respectively, for the purposes of comparison. Data on substance use disorders were collected, as these disorders are often comorbid with mania and MDD and can impact sleep duration and quality of sleep.
Analyses
Differences between the 2 groups were evaluated using student t tests and χ square tests as appropriate. The differences between sleep duration were examined using paired student t tests. The correlation between sleep duration and length of hospital stay was calculated after adjusting for benzodiazepine and antipsychotic dosage, use of a hypnotic, and a diagnosis of substance use disorder.
RESULTS
We retrospectively screened 81 patients admitted and discharged with a diagnosis of mania, and 41 patients met the inclusion and exclusion criteria. In the MDD group, we screened 246 patients, and 38 patients met the inclusion and exclusion criteria. Patients were excluded either because they were under a commitment process or because mania/MDD was not the primary diagnosis at the time of admission following review of the electronic record.
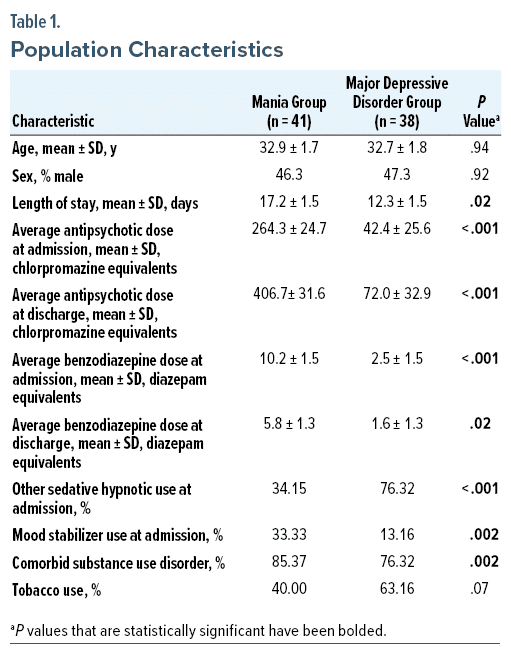
The mean ± SD age was 32.9 ± 1.7 years in the mania group and 32.7 ± 1.8 years in the MDD group (Table 1). The 2 groups did not differ based on sex, with 46.3% and 47.3% male in the mania and MDD groups, respectively (P = .92). The mean length of hospitalization was 17.2 ± 1.5 and 12.3 ± 1.5 days for the mania and MDD groups, respectively, which was significantly longer for patients with mania (by 4.95 days, P = .02).
Average antipsychotic dose differed between the groups both at admission and discharge. Patients admitted for mania received antipsychotic doses (in chlorpromazine equivalents) of 264.3 ± 24.7 mg at admission, while the MDD group received 42.4 ± 25.6 mg (P < .001). The mania group received 406.7 ± 31.6 mg in chlorpromazine equivalents at discharge, and the MDD group received 72.0 ± 32.9 mg (P < .001). The average benzodiazepine dose (in diazepam equivalents) also differed in the 2 groups; the mania group received 10.2 ± 1.5 mg at admission compared to the MDD group who were administered 2.5 ± 1.5 mg (P < .001). The mania group received 5.82 ± 1.29 mg in diazepam equivalents at discharge, and the MDD group received 1.6 ± 1.3 mg (P = .02). Sedative hypnotic use differed between the 2 groups, with 34.15% in the mania group and 76.3% in the MDD group (P < .001). Mood stabilizer use differed between the 2 groups, with 3.33% and 13.16% in the mania and MDD groups, respectively (P = .002). High rates of comorbid substance use were observed in both groups, with 85.4% in the mania group and 76.3% in the MDD group (P = .002). Tobacco use did not statistically differ between the groups, with 40% and 63% in the mania and MDD groups, respectively (P = .07).
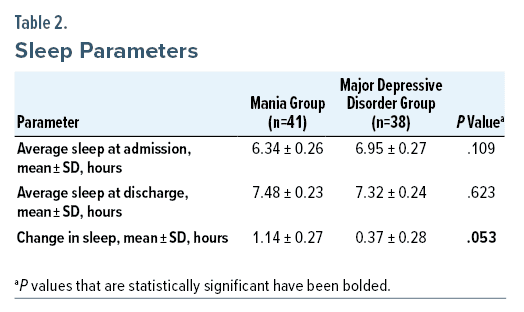
There was no statistically significant difference in sleep duration at admission between the mania group (6.34 ± 0.26 hours) and the MDD group (6.95 ± 0.27 hours, P = .109) (Table 2). Similarly, sleep duration at discharge was not statistically significant in the mania and MDD groups (7.48 ± 0.23 hours and 7.32 ± 0.24 hours, respectively, P = .623). However, change in sleep duration through hospitalization trended toward statistical significance at 1.14 ± 0.27 hours and 0.37 ± 0.28 hours in the mania and MDD groups, respectively (P = .05).
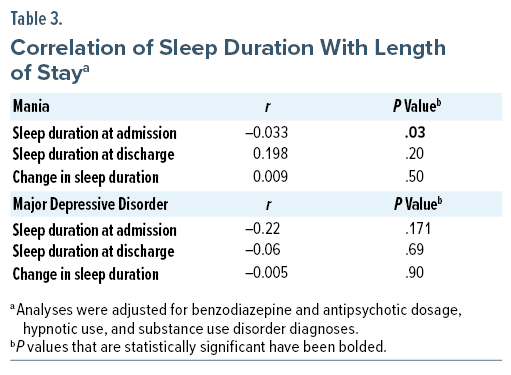
We examined the correlation between sleep duration at admission and discharge and change in sleep duration with length of stay after accounting for benzodiazepine and antipsychotic dosage, hypnotic use, and substance use disorder diagnoses (Table 3). In the mania group, sleep duration at admission negatively correlated with length of stay (r = –0.033, P = .03), but sleep duration at discharge (r = 0.198, P = .20) and change in sleep duration (r = 0.009, P = .50) were not correlated with length of stay. In the MDD group, sleep duration at admission (r = –0.22, P = .171) and at discharge (r = –0.06, P = .69) and change in sleep duration (r = –0.005, P = .90) were not correlated with length of stay.
DISCUSSION
We hypothesized that sleep duration would be significantly shorter in patients with mania compared to MDD. Our data revealed that sleep duration was shorter at admission in the mania group versus those with MDD, but this difference was not statistically significant. There was a trend toward greater improvement in sleep duration during hospitalization in patients with mania compared to those with MDD. Sleep duration at admission negatively correlated with length of hospitalization in patients with mania. Finally, patients with mania received higher dosages of antipsychotics, benzodiazepines, and mood stabilizers but fewer sedative hypnotics.
Prior studies have shown that during episodes of mania, most patients (69%–99%) demonstrate a reduced sleep duration based on self-report and polysomnography.5 Data from large trials suggest that insomnia is more common (up to 88%) than hypersomnia (27%) in patients with MDD.9 Therefore, it would be reasonable to postulate that the sleep duration of both patient groups may be reduced. Direct comparisons of sleep duration between these 2 conditions have not been previously undertaken.
Research into sleep duration and its association with length of hospital stay in patients with mania is limited. A study7 that compared patients with rapid improvements in manic symptoms to those who did not have a rapid response revealed that the former was more likely to have slept longer on the first night of hospitalization. This study7 did not examine whether greater improvements in sleep duration were associated with greater symptom improvement and/or shorter hospital stay. Another study6 of 100 patients with bipolar mixed or manic episodes showed that sleep duration increased slowly during the initial hospitalization, and this was followed by a rapid increase in sleep duration that preceded improvements in other manic and psychotic symptoms in the hospital. Taken together, these findings appear to suggest that sleep duration could predict the treatment response, correlate with hospital length of stay, and serve as a potential therapeutic target in patients with mania.
In our sample, similar to the study by Nowlin-Finch et al,7 shorter sleep duration at admission was associated with longer hospital stay. Short sleep duration at the time of admission could serve as a proxy for symptom severity and indicate more severe illness that may take longer to improve. The mean length of stay in the mania group of 17.2 ± 1.5 days in our sample was also comparable to prior research from the United States. However, length of hospitalization for a manic episode appears to be quite variable. In Sweden, the average length of inpatient stay for a manic episode is 29.2 days,10 Australia 49 days, Germany 40 days, and the United States 15 days.11 Unlike prior studies,10,11 we were able to compare sleep duration in patients with mania to those with MDD and found that sleep duration at admission and at discharge and change in sleep duration during hospitalization did not influence length of stay in patients with MDD.
As expected, patients with mania received higher dosages of antipsychotics, benzodiazepines, and mood stabilizers compared to those with MDD. Patients with MDD were more likely to be prescribed sedative hypnotic medications. The increased use of sedative hypnotic medications in patients with MDD could explain the longer sleep duration in these patients at baseline, although this difference did not reach statistical significance. Also, a significant proportion of patients with MDD were on antipsychotic medication as well as mood stabilizers, likely as augmenting medications. This could also have influenced the sleep duration at admission.
The sleep duration of 6.34 ± 0.26 hours at admission in our sample was slightly longer than a previously reported sleep duration of just under 5 ½ hours in a prior sample of hospitalized patients with bipolar mixed or manic episodes.6 The increased use of benzodiazepines in patients with mania, both as mood-stabilizing and hypnotic agents, may have precluded the need for additional sedative hypnotics and in conjunction with the use of antipsychotics/mood stabilizers potentially accounted for the longer than expected sleep duration at baseline.
Limitations
The results of our study need to be interpreted considering certain limitations. First, the sample size was fairly small, which likely explains the trend that did not reach statistical significance toward improvement in sleep duration in patients with mania versus MDD. Second, we observed that patients with mania were more likely to receive antipsychotics and benzodiazepines at admission and discharge. These medications have significant sedative effects and may increase sleep duration, possibly resulting in smaller differences between the 2 groups. However, our analyses examining the correlation between sleep duration and hospital stay accounted for these possible confounders. Third, systematic information about comorbidities including primary sleep disorders such as sleep apnea, periodic limb movement disorder, and restless legs syndrome as well as other medical and neurologic comorbidities was not available, and these conditions could have potentially impacted sleep in our patients. Last, our sleep data were collected by nursing staff who perform 15-minute safety checks, and if the patient does not appear awake, it is recorded as sleep time. Future studies should attempt to utilize more objective measures of sleep such as actigraphy; however, there are ethical concerns regarding consent for research during a manic episode, and observer report may be the best available proxy.
CONCLUSION
Sleep duration may be lower at admission in patients with mania compared to MDD, and there may be a greater improvement in sleep duration during hospitalization in those with mania. These findings did not reach statistical significance in our study likely due to the small sample size. After accounting for potential confounders, sleep duration at admission negatively correlated with length of hospital stay in patients with mania but not in those with MDD, suggesting that short sleep duration is a major feature of the underlying psychopathology in mania. Future investigations should explore whether sleep duration could serve as a treatment target to improve clinical outcomes in patients with mania.
Clinical Points
- Short sleep duration in patients with acute mania is associated with a longer length of hospital stay.
- Sleep duration may show greater improvements in patients with acute mania compared to those with major depressive disorder during acute hospitalization.
Article Information
Published Online: February 20, 2024.
https://doi.org/10.4088/PCC.23m03620
© 2024 Physicians Postgraduate Press, Inc.
Submitted: August 3, 2023; accepted: November 3, 2023.
To Cite: Golebiowski R, Mansukhani MP, Kolla BP. Correlates to improvement in sleep duration in acute mania and depression. Prim Care Companion CNS Disord. 2024;26(1):23m03620.
Author Affiliations: Center for Sleep Medicine, Mayo Clinic, Rochester, Minnesota (all authors); Department of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota (Kolla).
Corresponding Author: Bhanu Prakash Kolla, MD, FRCPsych, Mayo Clinic, 2nd St SW, Rochester, MN 55905 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: Poster presented at the American Academy of Sleep Medicine SLEEP annual meeting; Charlotte, North Carolina; virtual; June 4–8, 2022.
References (11)

- Krahn GL. WHO World Report on Disability: a review. Disabil Health J. 2011;4(3):141–142. PubMed CrossRef
- Merikangas KR, Jin R, He JP, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68(3):241–251. PubMed CrossRef
- Baldwin P, Browne D, Scully PJ, et al. Epidemiology of first-episode psychosis: illustrating the challenges across diagnostic boundaries through the Cavan-Monaghan study at 8 years. Schizophr Bull. 2005;31(3):624–638. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th Edition. American Psychiatric Publishing, a division of American Psychiatric Association; 2013.
- Harvey AG. Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. Am J Psychiatry. 2008;165(7):820–829. PubMed CrossRef
- Galynker II, Yaseen ZS, Koppolu SS, et al. Increased sleep duration precedes the improvement of other symptom domains during the treatment of acute mania: a retrospective chart review. BMC Psychiatry. 2016;16(1):98. PubMed CrossRef
- Nowlin-Finch NL, Altshuler LL, Szuba MP, et al. Rapid resolution of first episodes of mania: sleep related? J Clin Psychiatry. 1994;55(1):26–29. PubMed
- Barbini B, Bertelli S, Colombo C, et al. Sleep loss, a possible factor in augmenting manic episode. Psychiatry Res. 1996;65(2):121–125. PubMed CrossRef
- Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329–336. PubMed CrossRef
- Ösby U, Tiainen A, Backlund L, et al. Psychiatric admissions and hospitalization costs in bipolar disorder in Sweden. J Affect Disorders. 2009/06/01/ 2009;115(3):315–322.
- Auffarth I, Busse R, Dietrich D, et al. Length of psychiatric inpatient stay: Comparison of mental health care outlining a case mix from a hospital in Germany and the United States of America. Ger J Psychiatry. 2008:11.
Please sign in or purchase this PDF for $40.
Save
Cite