Prim Care Companion CNS Disord 2023;25(3):22cr03360
To cite: Spiegel DR, Yrastorza-Daghma MI, Sharma SS, et al. Differential diagnosis of anterograde amnesia from bilateral hippocampal ischemia due to opiate intoxication. Prim Care Companion CNS Disord. 2023;25(3):22cr03360.
To share: https://doi.org/10.4088/PCC.22cr03360
© 2023 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, Virginia
*Corresponding author: David R. Spiegel, MD, Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, 825 Fairfax Ave, Norfolk, VA 23507 ([email protected]).
Acute, complete, and bilateral ischemia of the hippocampus is a rare cause of anterograde amnesia (AA). While cardiopulmonary and cerebrovascular mechanisms have served as plausible etiologies, toxic exposures, especially to opiates, have recently gained increased notoriety.1 We present the case of a patient with no history of premorbid cognitive deficits who, after being found unconscious at her home, presented to our team with a clear mentation but dense AA.
Case Report
The patient was a 57-year-old woman who presented to the emergency department after an acute change in her mental status. She was described as somnolent, with decreased respiratory rate and oxygen saturation of 89%, which improved to 98% with 5 L of oxygen. Following administration of naloxone 0.2 g, her mentation improved. The patient’s past medical history was unremarkable, while her psychiatric history was notable for cocaine use disorder.
See Figure 1 for the patient’s diagnostic assessment. Her blood alcohol screen was negative, but the urine toxicology was positive for opiates.
On hospital day 2, the patient was reported to be alert, oriented times 1. On day 3, with stable vital signs, our team was consulted due to “altered mental status.” On evaluation, the patient repeatedly asked where she was and the events surrounding her current situation. She denied mood, psychotic, or lethality symptoms. The Confusion Assessment Method2 was scored as negative, while her Montreal Cognitive Assessment (MoCA)3 score was 22, losing 5, 2, and 1 point on delayed recalled, orientation, and attention, respectively. Notably, while being able to remember autobiographical information from her childhood, she was unable to recall where she currently lived or name any of the past 4 presidents.
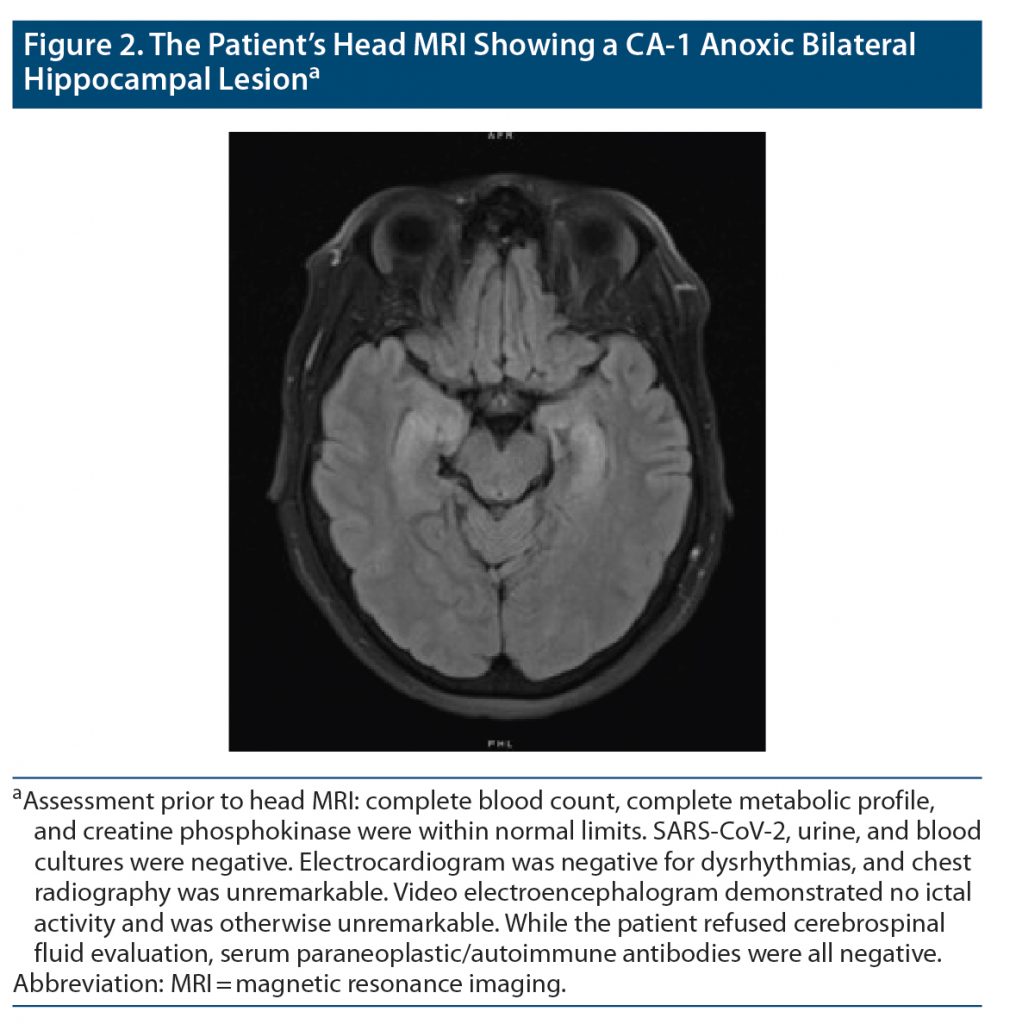
Magnetic resonance imaging (MRI) of the head without contrast was notable for bilateral symmetric restricted diffusion of hippocampal formations (Figure 2) indicative of in situ ischemia caused by toxic (ie, opiate/cocaine) insults rather than an embolic/cerebrovascular accident. Due to the symmetry of lesions, the radiology department added that it was unlikely lesions were related to cerebritis/encephalitis.
Five days after our initial evaluation, the patient’s MoCA score improved to 25, still losing 5 points on delayed recall. Seven days after our initial evaluation, retrograde amnesia resolved, and the patient was discharged. The patient’s AA ultimately resolved 9 months after hospital discharge.
Discussion
Since 2012, substance (primarily opiate)–induced, sudden-onset amnesia accompanied by bilateral injury to the hippocampus has been increasingly reported,4–7 resulting in a proposed opioid-associated amnestic syndrome (OAAS).8 The acuity of our patient’s AA prompted an evaluation for its etiology (see Figure 1).9–11 MRI of the head demonstrated complete and symmetric ischemic lesions in both hippocampi and the ultimate determination of OAAS as its etiology. While AA was the most overt symptom, our patient presented with associated deficits in orientation, attention/dysexecutive syndrome,12 and a transient global amnesia-type repetition of questions.13 Although AA is transient in most cases, alterations may last for months (as in our patient) or even years. Interestingly, non-memory cognitive deficits did improve within 1 week of AA onset.14
While a complete mechanistic review of AA is beyond the scope of this report, data suggest that opioids may inhibit γ-aminobutyric acidergic inhibitory interneurons in the hippocampus, thereby disinhibiting excitatory neurons. Additionally, focal increases in the rate of metabolism/glucose utilization in portions of the hippocampus (notably, ventral cornu ammonis 1 and 3) have been reported. Nonetheless, as in our patient, respiratory depression in an opiate-induced intoxicated state could result in hypoxemia, further amplifying the impact of excessive metabolic demands in vulnerable tissue.4
In closing, adding to an evolving evidence base, we recommend that substance use/disorder (especially opiates and cocaine) be assessed and the diagnosis of OAAS be strongly considered in relatively young patients who present with acute-onset AA associated with bilateral complete hippocampal lesions and no other identifiable etiology.
Published online: May 9, 2023.
Relevant financial relationships: Dr Spiegel is in the speaker’s bureau for Allergen, Alkermes, Otsuka, and Intra-Cellular Therapies but has no conflict of interest in preparation of this manuscript. The remainder of the authors have no disclaimer/conflict of interest to report.
Funding/support: There was no direct funding, other financial support (including drug company support), or material support received for this work.
Patient consent: Consent was verbally received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (14)

- Barash JA, Somerville N, DeMaria A Jr. Cluster of an unusual amnestic syndrome - Massachusetts, 2012-2016. MMWR Morb Mortal Wkly Rep. 2017;66(3):76–79. PubMed CrossRef
- Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method: a new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948. PubMed CrossRef
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. PubMed CrossRef
- Barash JA, Kofke WA. Connecting the dots: an association between opioids and acute hippocampal injury. Neurocase. 2018;24(2):124–131. PubMed CrossRef
- Barash JA, Ganetsky M, Boyle KL, et al. Acute amnestic syndrome associated with fentanyl overdose. N Engl J Med. 2018;378(12):1157–1158. PubMed CrossRef
- Small JE, Butler PM, Zabar Y, et al. Complete, bilateral hippocampal ischemia: a case series. Neurocase. 2016;22(5):411–415. PubMed CrossRef
- Duru UB, Pawar G, Barash JA, et al. An unusual amnestic syndrome associated with combined fentanyl and cocaine use. Ann Intern Med. 2018;168(10):747–748. PubMed CrossRef
- Barash JA, Whitledge J, Watson CJ, et al. Opioid-associated amnestic syndrome: description of the syndrome and validation of a proposed definition. J Neurol Sci. 2020;417:117048. PubMed CrossRef
- Förster A, Griebe M, Gass A, et al. Diffusion-weighted imaging for the differential diagnosis of disorders affecting the hippocampus. Cerebrovasc Dis. 2012;33(2):104–115. PubMed CrossRef
- Kang EG, Jeon SJ, Choi SS, et al. Diffusion MR imaging of hypoglycemic encephalopathy. AJNR Am J Neuroradiol. 2010;31(3):559–564. PubMed CrossRef
- Sili U, Kaya A, Mert A; HSV Encephalitis Study Group. Herpes simplex virus encephalitis: clinical manifestations, diagnosis and outcome in 106 adult patients. J Clin Virol. 2014;60(2):112–118. PubMed CrossRef
- Alessandro L, Ricciardi M, Chaves H, et al. Acute amnestic syndromes. J Neurol Sci. 2020;413:116781. PubMed CrossRef
- Owen D, Paranandi B, Sivakumar R, et al. Classical diseases revisited: transient global amnesia. Postgrad Med J. 2007;83(978):236–239. PubMed CrossRef
- Butler PM, Barash JA, Casaletto KB, et al. An opioid-related amnestic syndrome with persistent effects on hippocampal structure and function. J Neuropsychiatry Clin Neurosci. 2019;31(4):392–396. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite