In the United States, the death toll from opioid-related incidents escalated from 21,088 in 2010 to nearly 70,000 in 2020, primarily due to the influence of fentanyl and its analogs.1,2 This growing problem led to a staggering 1.68 million years of life lost in 2016 alone.3 Furthermore, the crisis disproportionately impacts younger adults, posing a significant public health challenge.3
Addressing acute opioid use disorder (OUD) and associated overdoses has become a pivotal concern for practitioners in emergency medicine.4 Medications for OUD initiated in emergency departments (EDs) have been increasingly effective, exhibiting enhanced patient retention rates in the short and long term.5–7 The ED is a distinct health care setting that often caters to a demographic especially susceptible to social and economic vulnerabilities.8,9 Implementing buprenorphine treatments for OUD in this context, complemented by subsequent outpatient referrals, has been shown to reduce morbidity and mortality.10
A recent study11 reveals increased buprenorphine prescriptions in EDs between 2002 and 2017. However, the study did not isolate prescriptions intended for OUD, encompassing those for other indications.11 A significant knowledge gap exists in trends concerning the diagnosis of OUD, the application of buprenorphine for its treatment, patient outcomes, and the distribution patterns of naloxone in the ED setting.
This study’s objectives were to examine trends in OUD and associated ED visits from 2016 to 2021, evaluate buprenorphine and naloxone prescribing patterns within these visits, and analyze the sociodemographic features and clinical outcomes of patients presenting for OUD.
Methods
Data source and study sample. We conducted a secondary analysis of data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) spanning the period 2016–2021.12 Administered annually by the National Center for Health Statistics (NCHS), NHAMCS is a nationally representative survey of outpatient visits to nonfederal, general, and short-stay hospitals across the United States. The survey’s methodology for its ED segment encompasses 3-tiered stages: (1) geographically based primary sampling units selected through a probabilistic approach, (2) individual hospitals within these primary sampling units, and (3) patient visits within the EDs of the selected hospitals.
The NHAMCS dataset includes a wide range of variables such as patient demographics, reasons for visits, vital signs, injury etiologies, diagnoses, administered diagnostic tests, executed procedures, medications administered or prescribed in the ED, care providers involved, and the ultimate disposition of the visit, including hospitalization details if applicable. Between 2016 and 2021, an annual average of 474 hospitals were selected for the survey. Of these, an average of 373 hospitals were deemed eligible, with 294 ultimately participating, resulting in an average unweighted response rate of 78.5%. The NCHS Ethics Review Board approves NHAMCS each year, waiving the need for obtaining patients’ informed consent and the authorization to disclose medical records by health care providers. Our study focused on the visits of patients aged ≥18 years. We adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines specifically designed for cross-sectional studies.13 This study was exempt from institutional review board approval owing to the utilization of de-identified, publicly available data.
Measures. OUD visits. We included all visits of patients aged ≥18 years with the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code F11, F11.1–F11.9 and created an indicator variable for OUD visits.
Opioid-related visits. We defined opioid-related visits by including all OUD visits (F11, F11.1–F11.9) along with the code for adverse effect/overdose of opioids (T40.0–T40.4 and T40.6) following the diagnosis code groupings of the Clinical Classifications Software Refined (CCSR) system, maintained by the Healthcare Cost and Utilization Project.14,15
Buprenorphine visits. Visits involving opioid prescriptions are identified using the Drug Therapeutic Category Level 3 codes for narcotic analgesics (code 060) and narcotic analgesic combinations (code 191). Buprenorphine visits were further specified into visits involving accompanying diagnosis of OUD ICD-10-CM codes used above.
Naloxone at discharge in OUD visits. Naloxone was defined by medication codes 20310 and 60995; all visits with OUD in which naloxone was prescribed at discharge were included in this measure.
Sociodemographic attributes and disposition. Sociodemographic variables of visits with the ICD-10-CM diagnostic code for OUD (F11 series) for the period 2016–2021 included the following:
- Age (18–44, 45–64, or 65+), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), and census region of residence (Northeast, Midwest, South, or West).
- Primary source of health insurance coverage (private, Medicare, Medicaid, self-pay, or other).
Furthermore, the disposition of the visits was also extracted. Sociodemographic data were presented as an unweighted number in the sample and a weighted percentage.
Data analysis. For 2016–2021, the survey data were divided into 3 periods: 2016–2017, 2018–2019, and 2020–2021. We combined data from 2 consecutive years to enhance the reliability of population estimates. Total adult visits, visits associated with OUD, opioid-related visits, visits with opioid prescriptions, buprenorphine visits, and visits where naloxone was administered at discharge for OUD were compared within the periods 2016–2017, 2018–2019, and 2020–2021 using chi-square tests with the Rao and Scott adjustment at a significance level of 0.05. Post hoc pairwise group comparisons were made using the Bonferroni correction.
Subsequently, we analyzed all opioid-related visits from 2016 to 2021 for their sociodemographic characteristics, reporting both the unweighted numbers and weighted percentages. The survey data were analyzed using the sample weight, adjusted for factors such as survey nonresponse, geographic region, and whether the location was urban or rural. This adjustment, carried out by the NCHS, aimed to provide unbiased national estimates of the frequency, percentages, and characteristics of ED visits.
Given the complexity of the survey’s sampling design, we used IBM SPSS version 28, which includes a complex sampling module, to calculate sampling errors and confidence intervals. This approach considers the clustered nature of the sample. Population estimates were produced only when there was a minimum of 30 unweighted sample visits, a relative standard error of less than 30%, and an item nonresponse rate of below 30%. As per the NCHS guidelines for analyzing NHAMCS data, all numerical estimates were rounded to the nearest thousand.
Results
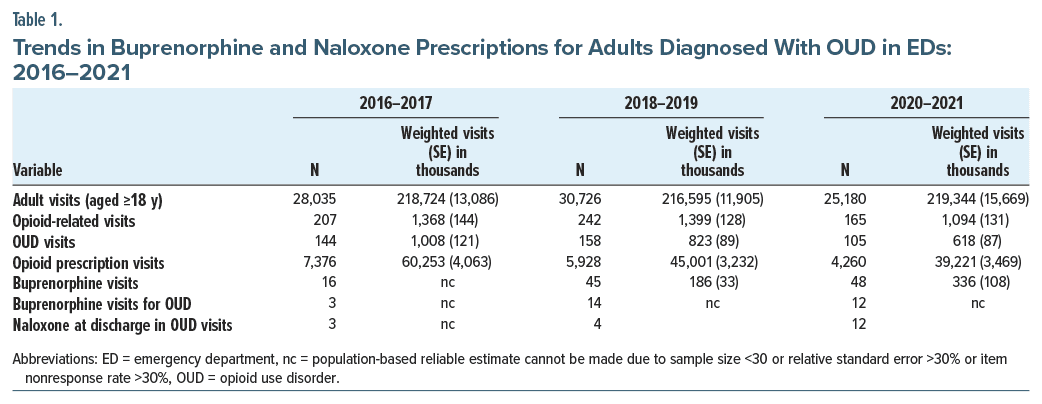
Between 2016 and 2021, the study examined 83,941 sampled medical visits involving adults aged ≥18 years, representing an estimated 655 million health care encounters. Of these, 407 visits were diagnosed with OUD, translating to approximately 2.4 million weighted visits. A statistically significant decline in visits diagnosed with OUD was observed in 2020–2021 compared with 2016–2017 (P = .009, adjusted P value after Bonferroni correction = .017). However, there was no statistically significant decline in opioid-related visits in 2020–2021 compared with previous years (Table 1).
During the study period, there was a notable decline in opioid prescription visits that reached statistical significance. Concurrently, there was a marked escalation in the issuance of buprenorphine prescriptions within the sample population. Specifically, the count of visits involving buprenorphine prescriptions increased 3-fold, from 16 visits in the period 2016–2017 to 48 visits in 2020–2021 (Table 1). Additionally, within visits categorized under OUD, buprenorphine prescriptions rose from 3 visits in the period 2016–2017 to 12 visits in 2020–2021 (Table 1).
Regarding the proportion of weighted buprenorphine visits within the overall opioid visits, the data indicate an increment from 0.4% in the period 2018–2019 to 0.8% in 2020–2021. Although this increase did not achieve statistical significance.
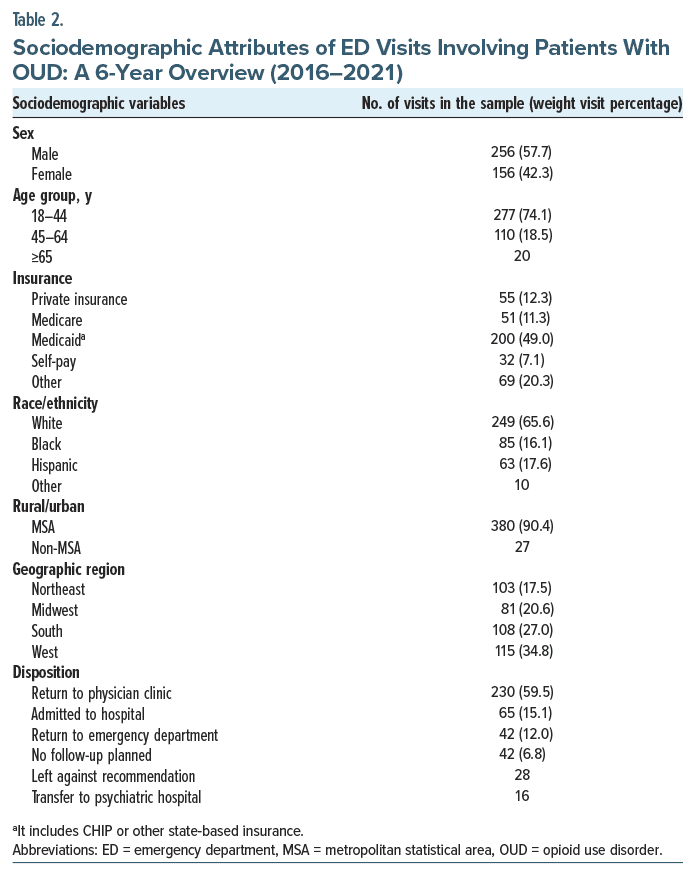
Additionally, among the 407 visits diagnosed with OUD, only 19 had naloxone prescribed at discharge. Demographically, 57.7% of the visits diagnosed with OUD involved males. Approximately 75% of the cases were individuals aged between 18 and 44 years. Further, 90% of these visits occurred in metropolitan statistical areas (Table 2). As per the NCHS guidelines, population estimates or weighted percentages were not calculated where the sample size was less than 30.
Discussion
Our study reveals a puzzling discrepancy: a decline in ED visits for OUD between 2016 and 2021, contrasting starkly with the escalation in opioid overdose fatalities, a crisis worsened by the COVID-19 pandemic.16,17 Previous research indicated an increase in fatal overdoses, most of which were opioid-related during the COVID-19 pandemic.18 We hypothesize that several factors may contribute to this incongruity. First, the COVID-19 pandemic substantially altered health care delivery worldwide, presenting unprecedented challenges in 2020–2021 that may have compromised the efficacy of OUD screenings in the ED. Additionally, the high-stress nature of EDs could impede comprehensive OUD screening and diagnosis. As previously reported, all-cause ED visits and substance use disorder–related visits initially decreased during the pandemic, which may have accounted for our findings.14
Our data indicate that although OUD-specific visits decreased in 2020–2021, overall opioid-related visits (combined OUD and overdose cases) did not significantly decline. This suggests that the reduction in OUD visits might have been counterbalanced by a surge in opioid overdose visits, resulting in a stable rate of overall opioid-related ED interactions.
Prior research suggests that a staggering 80% of patients with OUD remain untreated due to factors such as restricted access to health care providers, societal stigma, and inflexible insurance policies.19,20 EDs often serve as the initial health care touchpoint for this underserved population, who commonly face additional challenges such as limited health care access, underinsurance, and co-occurring mental or housing issues.21 These patients generally present with more severe conditions requiring intensive treatment.7 Alarmingly, approximately 5% of patients admitted to EDs for nonfatal overdoses succumb within a year, with one-fifth of these fatalities occurring within the first month.4 These findings emphasize the critical need for enhancing OUD screening, detoxification, and treatment initiation protocols in ED settings.
Evidence supports medication-based treatment for OUD with or without counseling.22–24 Initiating buprenorphine therapy in the ED and ensuring treatment continuity has been strongly correlated with improved patient outcomes.5,9,25,26 Despite proven benefits, buprenorphine prescription in EDs remains low.11 However, an in-depth analysis of the trend of buprenorphine prescriptions, particularly in the ED context in OUD, had not been previously conducted.
Buprenorphine prescription visits increased in 2020–2021 compared with 2018–2019. In the sample, buprenorphine prescriptions among OUD patients increased from 1 in 48 in 2016–2017 to roughly 1 in 9 in 2020–2021. However, the limited sample size often prevented reliable trend analysis at the population level. It is also important to note that several confounding factors could influence these results. For example, patients with mild OUD or those already on opioid antagonist treatments may not qualify for buprenorphine. Moreover, contraindicating factors such as recent methadone use, liver disease, altered mental status, impending surgeries, or concurrent use of alcohol or benzodiazepines add complexity to the clinician’s decision-making process in EDs. These factors necessitate an in-depth patient assessment to weigh the risks and benefits of initiating buprenorphine treatment, particularly given the often severe conditions encountered in the ED.
Initiating buprenorphine for eligible OUD patients, followed by consistent follow-up, is crucial for relapse prevention. In our study, about 7% of OUD patients had no planned follow-up, and 12% were instructed to return to the ED if necessary. Additionally, 28 patients left either before completing treatment or against medical advice. These statistics indicate an unmet need that could reduce recurrent ED visits for OUD or overdose if addressed. Moreover, around 60% of patients were advised to follow up with an outpatient provider. Implementing a system to ensure such follow-up could significantly aid in the long-term care of these patients. These measures can help minimize opioid-related repeat ED visits. These issues highlight the need for targeted strategies to expand ED-initiated buprenorphine treatment.
The distribution of naloxone in EDs is a scientifically validated harm reduction measure that is practical to implement and generally accepted by patients.27–29 However, its widespread adoption in EDs remains constrained.30 Our study indicates that among our sample, the rate of naloxone prescriptions upon discharge for patients diagnosed with OUD increased from 3 visits in the period 2016–2017 to 12 visits in 2020–2021. Despite this increase, the overall rate remains suboptimal: 19 of 407 patients with OUD in the sample studied between 2016 and 2021 were discharged with naloxone.
Our study also found demographic trends to be broadly consistent with existing literature. Most patients were male (approximately 57%), and 90% were from urban or metropolitan areas. The predominant age group for presentation was 18–44 years.
It is crucial to recognize the limitations of our study to gain a nuanced understanding of its scope and potential implications. One primary limitation concerns generalizability, as our study’s results apply exclusively to patients treated in nonfederal, general, and short-stay hospitals in the United States. Therefore, the findings may not apply to populations seeking health care in federal hospitals, specialized clinics, or health care systems in other nations. Additionally, the restricted sample size in specific subgroups limits our capacity to produce statistically significant national estimates, warranting larger datasets in future research. Another constraint arises from the characteristics of the NHAMCS dataset, which registers visits rather than individual patients, potentially leading to data duplication and confounding results. Our dataset also lacks details about the dosage of buprenorphine and its association with specific diagnoses, making it unclear whether the medication was prescribed for conditions such as pain or OUD in cases featuring comorbidities. Lastly, there is a need for targeted research to identify specific patient demographics that could most benefit from buprenorphine induction in EDs. Addressing these limitations in future research could significantly enhance the comprehensiveness and robustness of analyses on self-harm in ED settings.
Conclusion
Our study highlights key trends in OUD management in EDs, including a rise in buprenorphine and naloxone use. However, the unmet need remains substantial, especially given the decrease in OUD-related ED visits amid rising opioid fatalities. These findings urgently call for improved OUD screening and diagnosis in EDs.
Article Information
Published Online: April 2, 2024. https://doi.org/10.4088/PCC.23br03659
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(2):23br03659
Submitted: October 16, 2023; accepted November 22, 2023.
To Cite: Rizvi A, Nolte CL, Chumber P, et al. Emerging trends in opioid use disorder management: a 6-year analysis of emergency department visits, buprenorphine prescriptions, and naloxone distribution (2016–2021). Prim Care Companion CNS Disord. 2024;26(2):23br03659.
Author Affiliations: Department of Behavioral Medicine and Psychiatry, West Virginia University, Morgantown, West Virginia (Rizvi, Nolte, Chumber, Yadava, Wallace); Burrell Behavioral Health, Springfield, Missouri (Jagtiani).
Corresponding Author: Abid Rizvi, MD, Department of Behavioral Medicine and Psychiatry, West Virginia University, 936 Sharpe Hospital Rd, Weston, WV 26452 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Additional Information: The original dataset for the National Hospital Ambulatory Medical Care Survey (NHAMCS) is available from the National Center for Health Statistics and can be assessed at https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHAMCS/.
ORCID: Paramjit Chumber: https://orcid.org/0009-0009-3468-0124; Deep Yadava: https://orcid.org/0009-0001-2640-5001; Issaiah Wallace: https://orcid.org/0009-0003-1434-3442; Amit Jagtiani: https://orcid.org/0000-0001-9510-888X
References (30)

- Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001–2021. NCHS Data Brief. 2022;(457):1–8. PubMed CrossRef
- Drug overdose death rates. National Institutes of Health. Updated June 30, 2023. Accessed September 10, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
- Gomes T, Tadrous M, Mamdani MM, et al. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217. PubMed CrossRef
- Weiner SG, Baker O, Bernson D, et al. One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Ann Emerg Med. 2020;75(1):13–17. PubMed CrossRef
- D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–1644. PubMed CrossRef
- Initiating buprenorphine treatment in the emergency department. National Institutes of Health. Updated March 17, 2023. Accessed September 10, 2023. https://nida.nih.gov/nidamed-medical-health-professionals/discipline-specific-resources/emergency-physicians-first-responders/initiating-buprenorphine-treatment-in-emergency-department
- Herring AA, Vosooghi AA, Luftig J, et al. High-dose buprenorphine induction in the emergency department for treatment of opioid use disorder. JAMA Netw Open. 2021;4(7):e2117128. PubMed CrossRef
- Bitterman RA. EMTALA and the ethical delivery of hospital emergency services. Emerg Med Clin North Am. 2006;24(3):557–577. PubMed CrossRef
- Carroll C, Hand D, Covington W, et al. Emergency-department initiated buprenorphine: impact on quality of life. Drug Alcohol Depend Rep. 2023;9:100191. PubMed CrossRef
- Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Substance Abuse and Mental Health Services Administration. Accessed September 10, 2023. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf
- Rhee TG, D’Onofrio G, Fiellin DA. Trends in the use of buprenorphine in US emergency departments, 2002–2017. JAMA Netw Open. 2020;3(10):e2021209. PubMed CrossRef
- National Hospital Ambulatory Medical Care Survey (NHAMCS). Centers for Disease Control and Prevention. Accessed September 15, 2023. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/dataset_documentation/nhamcs/spss/
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147(8):W163–W194. PubMed CrossRef
- Venkatesh AK, Janke AT, Kinsman J, et al. Emergency department utilization for substance use disorders and mental health conditions during COVID-19. PLoS One. 2022;17(1):e0262136. PubMed CrossRef
- Clinical Classifications Software Refined (CCSR) for ICD-10-CM diagnoses. Healthcare Cost & Utilization Project. Accessed September 15, 2023. https://hcup-us.ahrq.gov/toolssoftware/ccsr/dxccsr.jsp#download
- Opioid facts. U.S. Department of Justice. Updated November 28, 2022. Accessed September 10, 2023. https://www.justice.gov/opioidawareness/opioid-facts
- Drug overdose deaths in the U.S. top 100,000 annually. Centers for Disease Control and Prevention. Updated November 17, 2021. Accessed September 10, 2023. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
- Soares WE 3rd, Melnick ER, Nath B, et al. Emergency department visits for nonfatal opioid overdose during the COVID-19 pandemic across six US health care systems. Ann Emerg Med. 2022;79(2):158–167. PubMed CrossRef
- Wu LT, Zhu H, Swartz MS. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117–127. PubMed CrossRef
- Mojtabai R, Mauro C, Wall MM, et al. Medication treatment for opioid use disorders in substance use treatment facilities. Health Aff (Millwood). 2019;38(1):14–23. PubMed CrossRef
- Guo CZ, D’Onofrio G, Fiellin DA, et al. Emergency department-initiated buprenorphine protocols: a national evaluation. J Am Coll Emerg Physicians Open. 2021;2(6):e12606. PubMed CrossRef
- Schackman BR, Leff JA, Polsky D, et al. Cost-effectiveness of long-term outpatient buprenorphine-naloxone treatment for opioid dependence in primary care. J Gen Intern Med. 2012;27(6):669–676. PubMed CrossRef
- Thomas CP, Fullerton CA, Kim M, et al. Medication-assisted treatment with buprenorphine: assessing the evidence. Psychiatr Serv. 2014;65(2):158–170. PubMed CrossRef
- Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–2066. PubMed CrossRef
- Thomas CP, Stewart MT, Tschampl C, et al. Emergency department interventions for opioid use disorder: a synthesis of emerging models. J Subst Abuse Treat. 2022;141:108837. PubMed CrossRef
- D’Onofrio G, McCormack RP, Hawk K. Emergency departments – a 24/7/365 option for combating the opioid crisis. N Engl J Med. 2018;379(26): 2487–2490. PubMed CrossRef
- Devries J, Rafie S, Ajayi TA, et al. Results of a naloxone screening quality-improvement project in an academic emergency department. J Emerg Med. 2019;56(4):378–385. PubMed CrossRef
- Kestler A, Buxton J, Meckling G, et al. Factors associated with participation in an emergency department-based take-home naloxone program for at-risk opioid users. Ann Emerg Med. 2017;69(3):340–346. PubMed CrossRef
- Gunn AH, Smothers ZPW, Schramm-Sapyta N, et al. The emergency department as an opportunity for naloxone distribution. West J Emerg Med. 2018;19(6):1036–1042. PubMed CrossRef
- O’Brien DC, Dabbs D, Dong K, et al. Patient characteristics associated with being offered take home naloxone in a busy, urban emergency department: a retrospective chart review. BMC Health Serv Res. 2019;19(1):632. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite