LESSONS LEARNED AT THE INTERFACE OF MEDICINE AND PSYCHIATRY
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(1):23f03549
Author affiliations are listed at the end of this article.
Have you ever been frustrated by patients whose distress over their physical symptoms is adversely impacting their ability to function? Have you ever been uncertain of the diagnosis in patients with multiple symptoms that appear out of proportion to diseases they may or may not have? Have you ever felt overwhelmed by patients who make frequent visits to the emergency department (ED) or your office due to their distress? If so, you may find the following case vignette and discussion both informative and useful for practice.
We present the concept of somatic symptom disorder (SSD), describe the diagnostic workup, and suggest ways to explain the diagnosis to the patient. Though a “standard of care” has yet to be established, several guiding principles and approaches are gaining traction. Through this article, we will share and expand upon these ideas. We suggest a close partnership between primary care and behavioral health as an optimal way to help these patients. Tactful explanation and management of the patient’s somatic symptoms and thoughtful timing of referral to behavioral health specialists are likely to strengthen therapeutic alliance and maximize chances for treatment success. In this article, we use the term primary care provider (PCP) since in many primary care practices, the evaluation and treatment of patients will be performed by nurse practitioners, physician assistants, and physicians (medical doctors).
CASE VIGNETTE
Ms A, a 40-year-old woman, was referred to the psychiatry clinic by her PCP for anxiety. She reported a long history of worrying about her health, frequently contacting her health care providers for reassurance. She stated that in the last 3 years, she has become increasingly preoccupied with palpitations that started soon after she began taking the antidepressant duloxetine for anxiety; these palpitations persisted with a switch to sertraline. She denied any significant life events at the time the palpitations began but did note that she started using a wearable heart rate monitor, which made her worries worse. The patient’s current medications are sertraline (50 mg daily), lorazepam (0.5 mg daily as needed), and propranolol (10 mg 3 times daily for palpitations). She is engaged in supportive psychotherapy. Ms A now requests a switch to a different antidepressant for anxiety about her health.
Ms A reported that low energy triggers concern about having cancer, and palpitations trigger concern that she is having side effects from her antidepressant. She reported fear of “never figuring out the causes” and that “a serious heart condition might be missed.” She felt angry and blamed herself for her inability to resolve her palpitations. She avoided trips to the grocery store and rarely socialized, as she was afraid to be away from home for more than 2 to 3 hours at a time. Ms A noted that on most days she spends significant time and energy dwelling on the source of her palpitations. Within the past year, Ms A had 3 ED visits for palpitations. At each visit, she had a normal physical examination and laboratory tests (including high-sensitivity troponins and electrocardiograms) and was discharged to receive follow-up care with her cardiologist.
As a child, she had difficulty being away from her mother due to worry about her mother’s health. She had high expectations for herself and was driven by a fear of failure. Since being diagnosed with illness anxiety disorder (IAD) in her 20s, she has tried multiple antidepressants including selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). Many trials lasted only 2 or 3 weeks with low doses due to her concern about palpitations. Her longest trial was with sertraline, chosen for low drug interaction potential and relative tolerability, which she has been taking for about 3 years. She admitted to making medication adjustments on her own, reducing the dose due to worry that it may be exacerbating her palpitations, and then resuming the previous dose to address her anxiety about having a serious illness. She has had individual psychotherapy on and off since her 20s with therapists using supportive therapy, cognitive-behavioral therapy (CBT), and dialectical-behavioral therapy.
Ms A denies a history of substance use disorders. She drinks socially 2–4 times a month, typically 1 to 2 drinks each time. She has not had thoughts of suicide, made suicide attempts, or engaged in self-injurious behaviors.
On mental status examination, Ms A was a well-groomed woman who appeared her stated age. She was calm and cooperative with direct and appropriate eye contact, and her speech had a normal rate and volume. She described her mood as “neutral” and “stable.” Affect was congruent and reactive. Memory, insight, and judgment were intact to observation. She denied suicidal or homicidal ideations.
Upon review of systems, Ms A disclosed palpitations and persistent fatigue. Her appetite and sleep were unremarkable. She reported a regular menstrual cycle and denied association with her symptoms. All other systems were reviewed and negative.
Laboratory results included complete blood count; basic metabolic panel; blood glucose level; and vitamin D, B12, folate, and thyroid function tests, which were all within normal range. Her body mass index was 21 kg/m2. She denied a history of COVID-19 infection, and her record showed that she has been fully vaccinated. An electrocardiogram (ECG) from 2 months ago showed a normal sinus rhythm with a single PVC.
Ms A’s medical history includes premature ventricular contractions (PVCs) and a distant history of anemia. She is followed by a cardiologist, who has completed a thorough workup of her palpitations including normal ECGs, echocardiograms, stress tests, and ambulatory remote cardiac monitoring that revealed normal sinus rhythm and infrequent (< 1%) PVCs. According to her cardiologist, her palpitations are due to her increased cardiac awareness of her ectopy, and she lacks clear risk factors for cardiovascular disease other than a family history of atrial fibrillation. Her mother, who is currently in stable health, has atrial fibrillation and was treated with surgery and chemotherapy for breast cancer. She denied a history of unexpected deaths in the family. She reported that her mother was prescribed sertraline for depression with moderate effectiveness.
What Is SSD?
SSD as a diagnosis was introduced in 2013 with the publication of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). SSD is characterized by intense psychological distress (thoughts, feelings, and behaviors) related to physical symptoms (bodily distress) that lasts for more than 6 months. SSD has replaced the DSM-IV diagnosis of somatization disorder, removing the criterion of “medically unexplained symptoms.”1 The core feature of this newly defined disorder is the degree of the patient’s psychological reaction to the symptoms, and the impact of that reaction on their ability to function, rather than on the presence or absence of a medical condition to explain the patient’s symptoms.2,3 The diagnostic criteria for SSD are straightforward compared to those for somatization disorder, which require a certain number of medically unexplained symptoms spread across several organ systems. This new conception of the illness as focusing on the psychological reaction to the symptoms rather than the cause of the symptoms is intended to reduce the stigma many patients have experienced with the diagnosis of somatization disorder and the commonly held interpretation that this means “it’s all in your head.” With a diagnosis of SSD, treatment will include techniques to address the thoughts, feelings, and behaviors of the patient in response to the somatic symptoms, with the goal of enabling the patient to engage in meaningful life activities despite having these sensations.
In response to having palpitations, Ms A exhibits thoughts (thinking it might be a side effect of the antidepressant or a serious medical condition), feelings (anxiety, fear, anger), and behaviors (avoiding the grocery store, avoiding social events) that interfere with normal life activities and relationships and are more intense and time-consuming than one would expect to see in someone with palpitations and reassuring cardiology exams. Since this has lasted over 6 months, Ms A meets criteria for the diagnosis of SSD.
Diagnosis: How Can SSD Be Differentiated From Other Disorders?
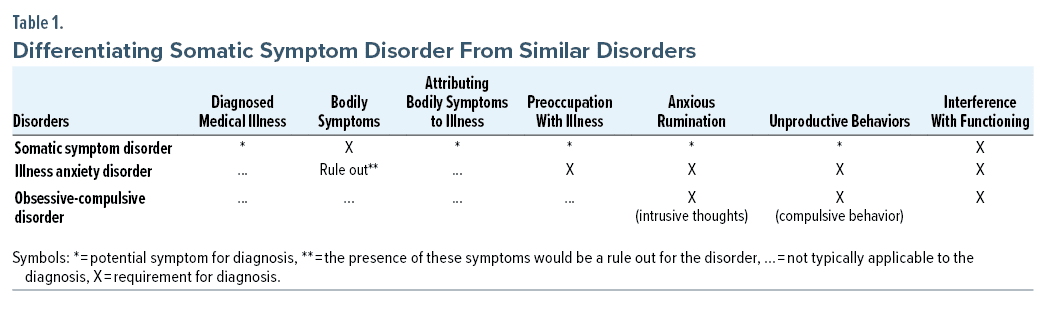
Experts have noted that for patients with SSD, anxiety is the driving force underlying the disproportionate reaction to their symptoms.3 Anxiety in the context of SSD can manifest as rumination, repetitive checking behaviors to manage the distress, and concerns about the implications of their bodily sensations. We must distinguish whether the patient is expressing a reaction to physical symptoms or having excessive concerns about potential physical symptoms that are not evident. The latter case would be better attributed to IAD. If the patient is focused on the potential for irrational consequences of the physical symptoms, then repeated requests for testing may be like the compulsions found in obsessive-compulsive disorder (OCD). Table 1 highlights the differences between SSD and related DSM-5 diagnoses, such as IAD and OCD, which have overlapping symptoms.
Although Ms A was previously diagnosed with IAD, her current condition is best characterized by the new diagnosis of SSD. Her previous general concerns about her health and her mother’s well-being have morphed into a new fear about the experience of specific bodily sensations. With this transition, the diagnosis of IAD is ruled out, and SSD becomes the most appropriate diagnosis.
Who Is at Risk of Becoming Preoccupied With Signs and Symptoms?
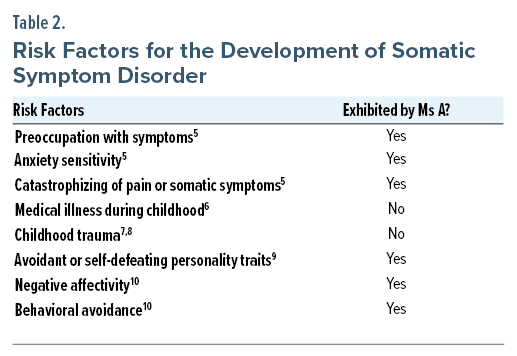
Risk factors for developing SSD include sociocultural, biological, genetic, psychiatric, and developmental contributors.4 Axelsson and colleagues5 investigated differences between patients diagnosed with fibromyalgia and those diagnosed with both fibromyalgia and SSD. In the comorbid group, patients were significantly more likely to be preoccupied with their symptoms, have anxiety sensitivity, and exhibit pain catastrophizing compared to those with fibromyalgia alone. A cross-sectional study of 116 medical outpatients found that an unusual or complicated medical illness during childhood was a risk factor for developing somatic preoccupation in adulthood.6 Several studies found that a history of childhood trauma or maltreatment was both a stand-alone risk factor and an antecedent to the later development of SSD.7,8 Studies investigating the interrelationship between psychiatric illness and SSD have found correlations between somatization, depression, and personality pathology.9,10 A recent review by Macina and colleagues9 investigated the overlap between personality pathology and the tendency to focus on somatic symptoms. They found that harm-avoidant and self-defeating personality traits were significantly associated with somatization.9 Mewes and colleagues10 found that negative psychological factors, such as catastrophizing, negative affectivity, and behavioral avoidance, can also perpetuate somatic symptoms. These risk factors are outlined in Table 2 and applied to our case to highlight relevant health history that might have alerted the PCP to a potential diagnosis of SSD during the initial assessment.
Cross-cultural studies have investigated whether individuals from non-White, non-Western cultures are more likely to somatize their emotional distress. Karasz and colleagues11 studied 2 groups of women from different cultural groups and found that physical symptoms tended to be more salient than psychological ones for South Asian participants as compared to White participants of European descent. In contrast, a recent study by Yeung and colleagues12 examined 57 Chinese immigrants with major depressive disorder (MDD) and found that roughly 70% described their symptoms with psychological terms instead of physical or “neutral” terms despite evidence that mental illnesses are highly stigmatized in Chinese society.13–18 Although research in the field is still evolving, PCPs should inquire about possible cultural meanings of somatic symptoms.
Ms A was referred to psychiatry after 3 years of preoccupation with her symptoms and frequent contact with her PCP and the ED. This type of dynamic is stressful for busy providers and their staff, unhelpful to the patient, and can be reduced with the early recognition of SSD risk factors and behaviors.
What Should the Workup Entail for Patients With SSD?
A patient’s preoccupation with their somatic symptoms will alert the clinician to a possible diagnosis of SSD, keeping in mind that SSD is not a diagnosis of exclusion and can co-occur with other medical diagnoses. When a diagnosis of SSD is suspected, it is especially important to inquire about substance use, trauma, major life events, psychosocial circumstances, and life stressors, in addition to the standard psychiatric and social history. The life context in which their symptoms first appeared should also be documented. The Somatic Symptom Disorder-1219 asks about thoughts, feelings, and behaviors associated with the somatic symptom(s) (criterion B in the DSM-5) and is a useful screening tool for SSD.
During the workup and follow-up, it is essential that PCPs avoid being pressured by their patient’s distress into ordering unnecessary tests.20 Research suggests that diagnostic tests do not produce meaningful reassurance in patients when their risk of severe disease is already low.21,22 Each subsequent test or procedure risks introducing false positives, incidental findings, additional follow-up testing, and increased costs and reinforcing the patient’s belief that their symptoms are due to an undiagnosed illness.22 Furthermore, unnecessary referrals will likely make the patient’s care more diffuse and can cause the patient to feel as though no one is willing to believe their lived experience.
It is frequently beneficial to explore the relationship between stress and the intensity of the patient’s symptoms during follow-up visits. The demonstration of the mind-body connection as an essential component of health sets the patient up for success with future treatments.3
In the post–COVID-19 era, the arrival of the new syndrome known as long COVID, or post COVID condition, can pose a challenge to the diagnosis of SSD in a patient. This is because the syndrome, by definition, can present with a myriad of symptoms both physical and mental, which can range in severity and degree of impact on the patient’s life and level of function.23 However, one has to remember the very definition of SSD when deciding whether to diagnose SSD in a long COVID patient, namely that it is the patient’s preoccupation with their somatic symptoms beyond what would be expected that should alert the clinician to a possible diagnosis of SSD. If the reaction itself is not making the symptoms worse, then it is not SSD. If the clinician has concerns that the patient’s thoughts or behaviors are hindering their recovery, then SSD and long COVID may be diagnosed simultaneously.
How Can SSD Be Explained to Patients?
Language and timing are essential elements of therapeutic communication with patients who suffer from SSD. It is helpful to first reassure the patient that their concerns are understood in scope and severity before giving a diagnosis of SSD. There is a considerable risk of harming the patient by delivering a diagnosis of SSD prematurely or using language that appears to dismiss the patient’s distress.
Considering that this critical inflection point can undermine the entire patient-provider relationship, it is important to begin considering SSD in the differential with the earliest signs of the patient’s preoccupation with their symptoms so that the concept of SSD (that our thoughts, feelings, and behaviors in reaction to a symptom can affect our perception of our symptom) may be introduced into the discussion before the medical workup is completed.
Once the medical workup is complete, the topic of SSD can be broached using the following phrase as a template: “We don’t yet know how to explain the cause or intensity of your symptoms, but we do know that sometimes your thoughts, emotions, and behaviors relating to the symptoms may cause additional distress.” We can then explore ways in which the patient’s emotional reactions intensify the symptoms. An ongoing search for a purely physical diagnosis and subsequent lack of answers often leads to frustration, anger, and feelings of being misunderstood or dismissed. With the diagnosis of SSD, a new direction of care is focused on developing positive coping strategies so that the patient can reclaim their ability to engage in meaningful and rewarding life activities.
Although there is no universal consensus on the mechanism underlying SSD, patients may benefit from hearing hypothesized pathways of symptom production. We can explain the physiologic fight-or-flight response and how persistent activation of the hypothalamic-pituitary axis (HPA) produces physical symptoms. Some patients may prefer the use of metaphors in understanding their condition, such as likening the patient’s symptoms to a software bug rather than a critical issue with their hardware.24 Henningsen3 describes SSD as a disorder of perception, in which the patient’s perception of their bodily sensations causes them alarm. Depending on their acceptance of the mind-body connection, some patients may resonate with the stress overload hypothesis in which our bodies produce somatic symptoms when holding on to too much stress. The explanation used will vary between patients and is ultimately dependent on the patient-provider relationship.
What Is the Role of Education and Compassionate Counseling When Treating People With SSD?
Continuous education and compassionate counseling are integral aspects of follow-up care. Adequate education empowers patients to self-monitor and manage their condition by engaging in healing behaviors between sessions. In a recent article, Pilipenko2 explained that even a single high-quality educational session on the patient’s condition can yield considerable improvements in the patient’s symptoms.
Patients will need to be reassured repeatedly that a thorough medical assessment has been completed and symptoms will continue to be assessed regularly. From this point of understanding, the focus can be on conveying that though distressing, their condition is not life-threatening; an artful blend of empathic concern and optimism for their condition can help to set SSD patients more at ease.25 A high level of trust is required to achieve a balance between reassuring patients that their current symptoms are not indicative of medical emergencies and educating patients about potential red-flag symptoms.
If Ms A had received education on the typical course of PVCs, she may have had less apprehension about her more benign symptoms. As a result, she may have had fewer worries about medication side effects, thus reducing the frequent changes in her antidepressant regimen. With this in mind, Ms A’s PCP would want to inform her that the palpitations were benign and then offer helpful management strategies for the palpitations.
What Do Treatment Strategies for SSD Involve?
Treatment of SSD is directed toward restoring functioning and learning how to cope with distressing somatic symptoms. Upon making the diagnosis of SSD, it is important to use the strength of the therapeutic relationship to elicit insight into the mind-body connection. Motivational interviewing techniques can be useful for this.26 A treatment frame with explicitly negotiated goals for functioning should be formulated. At the same time, PCPs will continue the equally important task of monitoring symptoms and pursuing additional workups as indicated.
Henningsen3 describes a stepped-care approach for SSD, beginning with healthy lifestyle interventions that can address contextual factors that may be perpetuating factors for SSD. Approaches such as meditation and acupuncture have proven useful for the management of stress. If alternative factors such as chronic social or traumatic stressors are present, additional resources and referrals (eg, domestic violence advocacy groups, substance use treatment) may be warranted.3
As described in the next section on pharmacotherapy, judicious use of medications can sometimes be helpful. Beyond physical interventions, psychotherapy can effectively reduce SSD symptoms in those who acknowledge that their thoughts, emotions, and behaviors can have both aggravating and ameliorating effects on their symptoms. Several evidence-based behavioral interventions have been validated for SSD including CBT, mindfulness-based stress reduction, stress management and resiliency training, and intensive short-term dynamic psychotherapy.27,28
What Types of Pharmacologic Management Can Be Used?
Pharmacologic treatment for SSD includes non-psychotropic medications, psychotropic medications, and herbs. Non-psychotropic medications are commonly used to alleviate somatic symptoms, regardless of their etiology.29,30 β-blockers (as in the case of Ms A), non-steroidal anti-inflammatory drugs, muscle relaxants, antiemetics, proton pump inhibitors, laxatives, antidiarrheal medications, antihistamines, and anticholinergics are often prescribed for symptom relief.31 These medications can provide meaningful symptom relief and, perhaps more importantly, communicate to the patient that their complaints are being heard and that solutions are being offered to them.
Psychotropic medications have also been shown to be effective in treating some somatic symptoms.30,32 Despite their mechanism of action being unknown, antidepressants have been effective for SSD; a promising hypothesis is that a substantial portion of patients with SSD have comorbid, undiagnosed anxiety, depression, or both. SSRIs (eg, escitalopram, fluoxetine), SNRIs (eg, venlafaxine), atypical antidepressants (eg, mirtazapine), and tricyclic antidepressants (eg, amitriptyline) have had positive effects in patients with somatization disorder, undifferentiated somatoform disorder, or multisomatoform disorder and may be considered for SSD before empirical evidence becomes available. Studies on the use of these agents have been limited by small sample sizes and short treatment durations. It remains unclear whether positive outcomes persist beyond 8 weeks, as studies with long-term follow-up are uncommon at this point. Limited data are available on the efficacy of antipsychotics and anticonvulsants for SSD. Levosulpiride (an antipsychotic used in Europe and Asia) and topiramate (an anticonvulsant) have improved the symptoms of somatoform disorder.32 Herbs are also used frequently in the treatment of SSD. The strongest evidence comes from studies on St John’s Wort, which was found to be efficacious in treating somatoform disorder.33 Though medications can be beneficial, it is important to be judicious in the use of pharmacologic treatments, as patients with SSD are often exquisitely sensitive to side effects.
When Should a Referral to a Mental Health Specialist Be Made?
When managing patients with SSD, an early “behind-the-scenes” consultation with a psychiatrist may be helpful in navigating any difficult dynamics in the patient-provider relationship. In some settings, this can be done as an “e-consult” (electronic consultation), which provides guidance from a psychiatrist to the PCP and does not involve having a psychiatrist see or evaluate the patient directly. A consultation with a psychiatrist may also facilitate the recognition of subtler psychosocial contributors or underlying, treatable mental health problems that the patient may have.29,34
For patients in whom symptoms do not improve, a referral to a psychotherapist or psychiatrist may be helpful. For some patients, this referral can be challenging, since they may inaccurately interpret this as indicating the PCP does not think the symptoms are real, or that a psychotherapist or psychiatrist is expected to “cure” the symptoms. Depending on the patient’s openness to a referral to behavioral health, it may take some time to prepare the patient for a referral. It may be necessary to repeat several times that the PCP will continue to follow the patient’s somatic symptoms, which at this point do not have an explanation, while the behavioral health clinician is a partner to help the patient cope with the symptoms and regain meaningful function in life. In patients who are more resistant to the referral, it can be helpful to have another behind-the-scenes consultation with a behavioral health specialist to discuss ways to frame the referral in a way that makes sense to the patient.
An embedded psychotherapist in the primary care practice is likely to be better received by the patient, as this treatment intervention occurs in a “safe” setting. With the wide availability of telehealth visits for psychotherapy, this option can be offered to patients, some of whom may find telehealth more comfortable. For treatment-resistant or severe cases, a referral to a psychiatrist, preferably the one behind the scenes early on, should be considered.
Despite many SSD patients initially feeling invalidated by a psychiatric referral, a systematic review of 6 randomized controlled trials including 449 patients with somatization revealed that even a 1-time consultation with a psychiatrist has been associated with a reduction in the severity of somatic symptoms, improved physical and social functioning, and, importantly, decreased medical costs.35
Collaborative Approach
As a disorder integrally rooted in both the mind and body, SSD poses a unique opportunity for primary care and behavioral health specialists to collaborate in an interdisciplinary care model. Successfully initiated collaboration with behavioral health should reduce the number of visits patients with SSD make to PCPs and EDs. As previously mentioned, psychopharmacotherapy can play a supportive role in the treatment of SSD and is particularly useful for the treatment of comorbid mood or substance use disorders. However, despite their usefulness, there remains a risk that medication side effects can confound the burden of somatic symptoms; therefore, a combination of physical interventions and psychotherapy remains the default treatment for SSD.29,34
What Happened to Ms A?
Sertraline was discontinued due to Ms A’s persistently high anxiety about whether the medication could be making her palpitations worse. Given the lack of clear benefits with multiple antidepressant trials and the substantial anxiety about potential side effects, the patient agreed to try psychotherapy with CBT targeted at modifying distressing thoughts and behaviors. Lorazepam as needed for anxiety and propranolol for palpitations were continued. In addition to CBT, Ms A incorporated relaxation techniques and mindfulness meditation into her daily routine with moderate effectiveness. Several weeks later, she informed her psychiatrist that she had restarted the sertraline 50 mg daily. She explained that she continued to experience palpitations despite stopping the sertraline, which indicated to her that sertraline was not the cause of her palpitations. Ms A continues to be treated in the psychiatry clinic. Although she continues to be anxious about being away from home for long periods, she has resumed trips to the grocery store, reconnected with friends, and enjoys occasional informal social activities.
Some missed opportunities and how they were addressed by the psychiatrist 3 years after the onset of SSD include the following:
- Delayed introduction of SSD as part of the clinical picture: Discussed with the PCP, acknowledged barriers including lack of familiarity with diagnosis of SSD, time constraints, and complexity of obtaining early consultation with a psychiatrist.
- Lack of coordinated team approach to patient: Communicated with the cardiologist and PCP about SSD so that the patient receives consistent feedback on the objective physical findings, reassurance that her symptoms are being monitored, and the importance of overcoming her disproportionate anxiety to pursue meaningful activities in her life.
- Psychoeducation on medication: An open dialogue with the patient about the hypothesized mechanisms of antidepressants in treating SSD and the potential risks of frequent medication changes while validating her concerns about the side effects could have brought better outcomes.
CONCLUSION
SSD differs from the past DSM-IV diagnosis of somatization in that it focuses on the disproportionate psychological reaction to the somatic symptoms rather than on the “medically unexplained” nature of the somatic symptoms. In fact, SSD can co-occur with a medical diagnosis. The diagnosis of SSD creates more room for a therapeutic alliance and the possibility of a treatment plan that helps the patient regain as much function and meaningful activity as possible. As SSD was only defined in 2013, it is important to incorporate SSD diagnosis and treatment into medical school and residency curricula.
Article Information
Published Online: January 23, 2024. https://doi.org/10.4088/PCC.23f03549
© 2024 Physicians Postgraduate Press, Inc.
Submitted: April 25, 2023; accepted November 10, 2023.
To Cite: Tuttle MC, Ciampa DJ, Godena E, et al. The evaluation and treatment of somatic symptom disorder in primary care practices. Prim Care Companion CNS Disord. 2024;26(1):23f03549.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, Boston (Tuttle, Kim, Vanwort-Meng, Verma, Stern, Yeung); Connell School of Nursing, Boston College, Chestnut Hill, Massachusetts (Ciampa); Department of Neurology, Massachusetts General Hospital, Harvard Medical School, Boston (Godena); Department of Medicine, Massachusetts General Hospital, Harvard Medical School, Boston (Sakmar).
Author Contributions: Drs Stern and Yeung are co-senior authors.
Corresponding Author: Margaret Cheng Tuttle, MD, Massachusetts General Hospital, Department of Psychiatry, 15 Parkman St, WAC815, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Somatic symptom disorder (SSD) is characterized by a psychological reaction (thoughts, feelings, behaviors) that is out of proportion to the somatic symptoms.
- When a diagnosis of SSD is suspected, a detailed psychosocial history, focusing on the patient’s major life stressors and the context in which their symptoms originated, should be obtained.
- Before giving a diagnosis and treatment plan for SSD, the provider should assure the patient that their concerns about somatic symptoms have been heard and evaluated according to medical guidelines and will continue to be monitored regularly.
- A close partnership between primary care and behavioral health is an optimal way to help patients with SSD; a behind-the-scenes consultation with behavioral health about suitability and timing of psychotherapy initiation could pave the way for a successful referral.
References (35)

- Association AP. Diagnostic and Statistical Manual of Mental Disorders, DSM-5. Fifth Edition. American Psychiatric Publishing; 2013.
- Pilipenko N. Somatic symptom disorder in primary care: a collaborative approach. J Fam Pract. 2022;71(3):E8–E12. PubMed CrossRef
- Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. 2018;20(1):23–31. PubMed CrossRef
- Battle DE. Diagnostic and statistical manual of mental disorders (DSM). Codas. 2013;25(2):191–192. PubMed CrossRef
- Axelsson E, Hedman-Lagerlöf M, Hedman-Lagerlöf E, et al. Symptom preoccupation in fibromyalgia: prevalence and correlates of somatic symptom disorder in a self-recruited sample. Psychosomatics. 2020;61(3):268–276. PubMed CrossRef
- Sansone RA, Buckner VR, Tahir NA, et al. Early family environment, borderline personality symptoms, and somatic preoccupation among internal medicine outpatients. Compr Psychiatry. 2009;50(3):221–225. PubMed CrossRef
- Sansone RA, Wiederman MW, Sansone LA. Adult somatic preoccupation and its relationship to childhood trauma. Violence Vict. 2001;16(1):39–47. PubMed CrossRef
- Sansone RA, Gaither GA, Barclay J. Childhood trauma and somatic preoccupation in adulthood among a sample of psychiatric inpatients. Psychosomatics. 2002;43(1):86. PubMed CrossRef
- Macina C, Bendel R, Walter M, et al. Somatization and somatic symptom disorder and its overlap with dimensionally measured personality pathology: a systematic review. J Psychosom Res. 2021;151:110646. PubMed CrossRef
- Mewes R, Feneberg AC, Doerr JM, et al. Psychobiological mechanisms in somatic symptom disorder and depressive disorders: an ecological momentary assessment approach. Psychosom Med. 2022;84(1):86–96. PubMed CrossRef
- Karasz A, Dempsey K, Fallek R. Cultural differences in the experience of everyday symptoms: a comparative study of South Asian and European American women. Cult Med Psychiatry. 2007;31(4):473–497. PubMed CrossRef
- Yeung A, Norton R, Dean T, et al. Depressed Chinese Americans present predominantly psychological symptoms: a new trend or different outcomes due to methodological differences? Asian J Psychiatr. 2021;61:102684. PubMed CrossRef
- Chan B, Parker G. Some recommendations to assess depression in Chinese people in Australasia. Aust N Z J Psychiatry. 2004;38(3):141–147. PubMed CrossRef
- Chung KF, Wong MC. Experience of stigma among Chinese mental health patients in Hong Kong. Psychiatr Bull. 2004;28(12):451–454. CrossRef
- Lin KM, Kleinman A, Lin TY. Overview of mental disorders in Chinese cultures: review of epidemiological and clinical studies. In: Kleinman A, Lin TY, eds. Normal and Abnormal Behavior in Chinese Culture. Culture, Illness, and Healing. Springer Netherlands; 1981:237–272. doi:10.1007/978-94-017-4986-2_13
- Parker G, Gladstone G, Chee KT. Depression in the Planet’s Largest Ethnic Group. Depression in the planet’s largest ethnic group: the Chinese. Am J Psychiatry. 2001;158(6):857–864. PubMed CrossRef
- Ryder AG, Alden LE, Paulhus DL. Is acculturation unidimensional or bidimensional? a head-to-head comparison in the prediction of personality, self-identity, and adjustment. J Pers Soc Psychol. 2000;79(1):49–65. PubMed CrossRef
- Lee E, Mock MR. Asian families: an overview. In: Ethnicity and Family Therapy. 3rd ed. The Guilford Press; 2005:269–289.
- Toussaint A, Murray AM, Voigt K, et al. Development and Validation of the Somatic Symptom Disorder-B Criteria Scale (SSD-12). Psychosom Med. 2016;78(1):5–12. PubMed CrossRef
- Kroenke K. Diagnostic testing and the illusory reassurance of normal results: comment on “reassurance after diagnostic testing with a low pretest probability of serious disease”. JAMA Intern Med. 2013;173(6):416–417. PubMed CrossRef
- van Ravesteijn H, van Dijk I, Darmon D, et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3–8. PubMed CrossRef
- Rolfe A, Burton C. Reassurance after diagnostic testing with a low pretest probability of serious disease: systematic review and meta-analysis. JAMA Intern Med. 2013;173(6):407–416. PubMed CrossRef
- Soriano JB, Murthy S, Marshall JC, et al; WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–e107. PubMed CrossRef
- Aybek S, Perez DL. Diagnosis and management of functional neurological disorder. BMJ. 2022;376:o64. PubMed CrossRef
- Yeung A, Deguang H. Somatoform disorders. West J Med. 2002;176(4):253–256. PubMed
- Tolchin B, Baslet G, Martino S, et al. Motivational interviewing techniques to improve psychotherapy adherence and outcomes for patients with psychogenic nonepileptic seizures. J Neuropsychiatry Clin Neurosci. 2020;32(2):125–131. PubMed CrossRef
- Williams C, Carson A, Smith S, et al. Overcoming Functional Neurological Symptoms: A Five Areas Approach. 1st ed. CRC Press; 2017.
- Abbass MA, Schubiner MH. Hidden From View: A Clinician’s Guide to Psychophysiologic Disorders. 1st ed. Psychophysiologic Press, LLC; 2018.
- Kurlansik SL, Maffei MS. Somatic symptom disorder. Am Fam Physician. 2016;93(1):49–54. PubMed
- O’Malley PG, Jackson JL, Santoro J, et al. Antidepressant therapy for unexplained symptoms and symptom syndromes. J Fam Pract. 1999;48(12):980–990. PubMed
- Hede V, Devillé C. Treating psychiatric symptoms and disorders with non-psychotropic medications . Dialogues Clin Neurosci. 2019;21(2):193–201. PubMed CrossRef
- Somashekar B, Jainer A, Wuntakal B. Psychopharmacotherapy of somatic symptoms disorders. Int Rev Psychiatry. 2013;25(1):107–115. PubMed CrossRef
- Müller T, Mannel M, Murck H, et al. Treatment of somatoform disorders with St. John’s Wort: a randomized, double-blind and placebo-controlled trial. Psychosom Med. 2004;66(4):538–547. PubMed CrossRef
- Croicu C, Chwastiak L, Katon W. Approach to the patient with multiple somatic symptoms. Med Clin North Am. 2014;98(5):1079–1095. PubMed CrossRef
- Hoedeman R, Blankenstein AH, van der Feltz-Cornelis CM, et al. Consultation letters for medically unexplained physical symptoms in primary care. Cochrane Database Syst Rev. 2010;(12):CD006524. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite