Prim Care Companion CNS Disord 2021;23(3):20l02780
To cite: Smith CM, Komisar JR, Wasserman BR, et al. Got 2 good eyes but you still can’t see: an atypical case of Wernicke’s encephalopathy. Prim Care Companion CNS Disord. 2021;23(3):20l02780.
To share: https://doi.org/10.4088/PCC.20l02780
© Copyright 2021 Physicians Postgraduate Press, Inc.
aDepartment of Medicine, Duke University Medical Center, Durham, North Carolina
bDepartment of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, North Carolina
*Corresponding author: Colin M. Smith, MD, Department of Medicine, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, 2301 Erwin Rd, Durham, NC 27710 ([email protected]).
Wernicke’s encephalopathy was first described in 1881 as encephalopathy, ophthalmoplegia, and gait ataxia.1 Thiamine deficiency was later identified as the underlying cause.2 Today, Wernicke’s encephalopathy is most commonly identified in patients with alcohol use disorder, though eating disorders are also implicated.3,4 We present a case of atypical Wernicke’s encephalopathy in a woman with avoidant/restrictive food intake disorder (ARFID) presenting with bilateral ophthalmoplegia and normal serum thiamine levels.
Case Report
A 24-old-woman was brought to the hospital for acute onset of bilateral blurry vision. The deficit began 6 days prior to admission when she noticed worsening eyesight over hours. She was seen by an optometrist on the day of presentation, who urged her to seek care in the emergency department.
Information obtained later in her course revealed that she had a 70-lb weight loss over the past year after restricting her eating and a diagnosis of ARFID (DSM-5 criteria). She had presented to the emergency department multiple times over the past 2 years in the setting of starvation related to abdominal pain. Previous workup with abdominal film, computed tomography, esophagogastroduodenoscopy, ultrasound, and barium swallow had been unremarkable, leading to psychiatric evaluation and diagnosis of ARFID.
On presentation, her pulse was elevated at 113 bpm. She was oriented and attentive. The ophthalmologic examination was notable for near total restriction of all eye movement without nystagmus. She was blind in her right eye and had 20/800 vision in her left eye. Both eyes had normal ocular pressure, with edema and well perfused vessels. The neurologic examination was revealing for hyperalgesia over her lower extremities without gait ataxia.
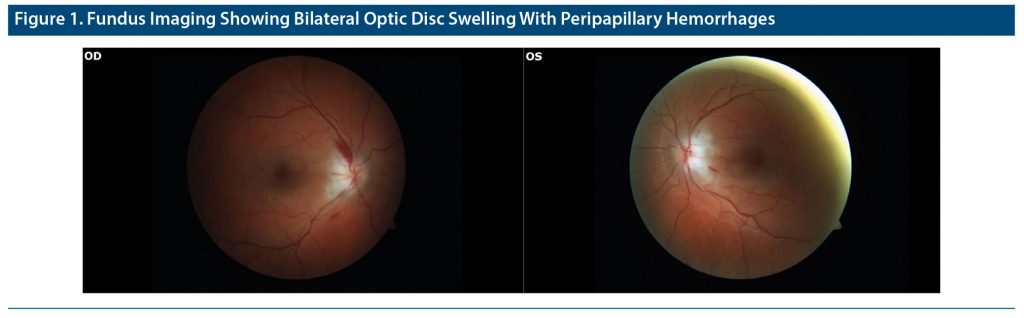
Blood chemistry showed a sodium level of 147 mmol/L and potassium level of 2.9 mmol/L, and blood count revealed a hemoglobin level of 10.3 g/dL. Renal and thyroid function and albumin, liver enzyme, copper, vitamin E, niacin, vitamin B12 (600 pg/mL), and serum thiamine (158.4 nmol/L) levels were all within normal limits. Toxicology was negative. Vitamin A (12.8 μg/dL), vitamin D (22 ng/mL), and folate (5.4 ng/mL) levels were low. Magnetic resonance imaging (MRI) of the brain and orbits was normal, but fundus imaging showed optic disc swelling with peripapillary hemorrhages (Figure 1). Cerebrospinal fluid studies, including venereal disease research laboratory, lactate, and cytology, were normal. Paraneoplastic panel, ganglioside antibody, anti-GQ1b, and HIV test results were negative, and angiotensin-converting enzyme level was normal.
Despite a normal serum thiamine level on initial evaluation, the patient’s history of ARFID, significant weight loss, and evidence of ophthalmoplegia led to empiric treatment with 500 mg of intravenous thiamine every 8 hours for 5 doses followed by 100 mg daily. Within 24 hours, her vision returned to 20/20 and her bilateral ophthalmoplegia resolved. She required prolonged hospitalization after medical stabilization to facilitate transfer to an inpatient eating disorder facility to treat ARFID.
Since her discharge, she had 1 additional admission requiring a gastrostomy tube for starvation and has since been seen in outpatient therapy for ARFID. She has had no return of return of Wernicke’s encephalopathy on maintenance thiamine 100 mg daily by gastrostomy tube.
Discussion
Wernicke’s encephalopathy is an acute life-threatening condition caused by thiamine deficiency that classically presents with the triad of encephalopathy, ophthalmoplegia, and gait ataxia.5 However, these 3 symptoms occur together in less than one-quarter of cases.6 Causes include alcohol use, nutritional deficiencies, and impaired gastrointestinal absorption.7 Most often, Wernicke’s encephalopathy is a clinical diagnosis and requires 2 of the following 4 signs: (1) dietary deficiency, (2) oculomotor abnormalities, (3) cerebellar dysfunction, and (4) altered mental state.8
This report represents the first published case, to our knowledge, of Wernicke’s encephalopathy in ARFID.9 Although Wernicke’s encephalopathy has been seen in eating disorders, the majority of these cases have presented with the classic clinical triad.4 Our patient presented with isolated bilateral ophthalmoplegia and optic disc swelling, a less recognized manifestation of Wernicke’s encephalopathy.10 This case also demonstrates that serum thiamine levels may not reflect brain levels of thiamine.11 Despite lacking many of the classic laboratory, imaging, or clinical sings, our patient met 2 of the 4 Caine criteria8 for Wernicke’s encephalopathy and responded clinically to empiric thiamine within 24 hours. Finally, this case highlights that clinical suspicion of Wernicke’s encephalopathy in all at-risk patients warrants immediate administration of high-dose intravenous thiamine.12,13
Published online: May 13, 2021.
Potential conflicts of interest: None.
Funding/support: None.
Disclaimer: The opinions expressed herein are those of the authors and do not necessarily reflect those of the US Government or any of its agencies.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (13)

- Wernicke C. Der acute haemorrhagische Polioencephalitis superior. In: Lehrbuch der Gehirnkrankheiten. Villengang, Germany: VEB Gustav Fischer Verlag; 1881:229–242.
- Campbell ACP, Biggart JH. Wernicke’s encephalopathy (polioencephalitis hæmorrhagica superior): its alcoholic and non-alcoholic incidence. J Pathol. 1939;48(2):245–262. CrossRef
- Harper C, Fornes P, Duyckaerts C, et al. An international perspective on the prevalence of the Wernicke-Korsakoff syndrome. Metab Brain Dis. 1995;10(1):17–24. PubMed CrossRef
- Oudman E, Wijnia JW, Oey MJ, et al. Preventing Wernicke’s encephalopathy in anorexia nervosa: a systematic review. Psychiatry Clin Neurosci. 2018;72(10):774–779. PubMed CrossRef
- Thomson AD, Cook CC, Guerrini I, et al. Wernicke’s encephalopathy revisited: translation of the case history section of the original manuscript by Carl Wernicke ‘Lehrbuch der Gehirnkrankheiten fur Aerzte and Studirende’ (1881) with a commentary. Alcohol Alcohol. 2008;43(2):174–179. PubMed CrossRef
- Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry. 1986;49(4):341–345. PubMed CrossRef
- Chamorro AJ, Rosón-Hernández B, Medina-García JA, et al; Wernicke-SEMI Group; Alcohol and Alcoholism Group; Spanish Society of Internal Medicine (SEMI). Differences between alcoholic and nonalcoholic patients with Wernicke encephalopathy: a multicenter observational study. Mayo Clin Proc. 2017;92(6):899–907. PubMed CrossRef
- Caine D, Halliday GM, Kril JJ, et al. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997;62(1):51–60. PubMed CrossRef
- Katzman DK, Norris ML, Zucker N. Avoidant restrictive food intake disorder. Psychiatr Clin North Am. 2019;42(1):45–57. PubMed CrossRef
- Bohnsack BL, Patel SS. Peripapillary nerve fiber layer thickening, telangiectasia, and retinal hemorrhages in wernicke encephalopathy. J Neuroophthalmol. 2010;30(1):54–58. PubMed CrossRef
- Davies SB, Joshua FF, Zagami AS. Wernicke’s encephalopathy in a non-alcoholic patient with a normal blood thiamine level. Med J Aust. 2011;194(9):483–484. PubMed CrossRef
- 12. Galvin R, Bråthen G, Ivashynka A, et al; EFNS. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17(12):1408–1418. PubMed CrossRef
- Thomson AD, Cook CC, Touquet R, et al; Royal College of Physicians, London. The Royal College of Physicians report on alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and emergency department. Alcohol Alcohol. 2002;37(6):513–521. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite