Clarke and Kissane1 interpret Jerome Frank’s concept of demoralization not only as “nonspecific distress” but also as a “clearly defined syndrome of existential distress” affecting patients with physical and mental illness, of the caliber to affect “life or integrity of being.”(p733) While most who experience major depressive disorder (MDD) have anhedonia—diminished interest, desire, effort, and consummatory pleasure2—demoralized patients have feelings of subjective “incompetence, hopelessness, and helplessness.”3 Multiple studies demonstrate that in those with psychiatric and medical illness, hopelessness is more strongly associated with suicidal intent instead of depression.4,5 Chronic, prolonged physical illness that requires persistent, scheduled treatment such as hemodialysis may threaten a patient’s autonomy, slowly decoupling a patient’s sense of self-efficacy and self-esteem, and deprives them of participation in efforts to find meaning in their daily life (eg, physical activities that may help improve their mental health).
Psychiatrists are sometimes tasked with assessing demoralized and suicidal patients with decision-making capacity, whose wishes and values go against the established medical ethos. In this case report, we detail how psychiatrists can remain steadfast in respecting the wishes and values of patients who have a desire to withdraw care within an established ethical framework.
Case Report
Ms A, a 27-year-old patient with granulomatosis with polyangiitis and end-stage renal disease on 7 years of hemodialysis, presented to the emergency department with passive suicidal ideation and abdominal pain after missing a week of hemodialysis. Her psychiatric history included MDD, posttraumatic stress disorder, and tobacco, cannabis, and cocaine use disorders. She repeatedly declined medications, diagnostic laboratory testing/imaging, and dialysis, stating, “I do not want to live like this anymore,” referencing chronic illness and hemodialysis dependence.
The psychiatry team was consulted for MDD exacerbation and determined she had decision-making capacity to decline dialysis; the patient’s distress and wishes to withdraw treatment did not originate from MDD exacerbation but were rooted in demoralization from declining health over 5 years. An interdisciplinary team collaborated to understand her goals of care leading to a do-not-resuscitate order aligned with her values of independence and comfort. Ms A, supported by her mother, was discharged to hospice.
Discussion
The psychiatry team assessed the patient’s emotional distress, suicidal ideation, and decision-making capacity in tandem with the ethics consultant addressing the decision of withdrawing dialysis and pursuing hospice care. Ethics teams are often underutilized at most medical centers and offer an opportunity to share uncertainty, as complex dilemmas need to be shared and delegated for proper resolution.
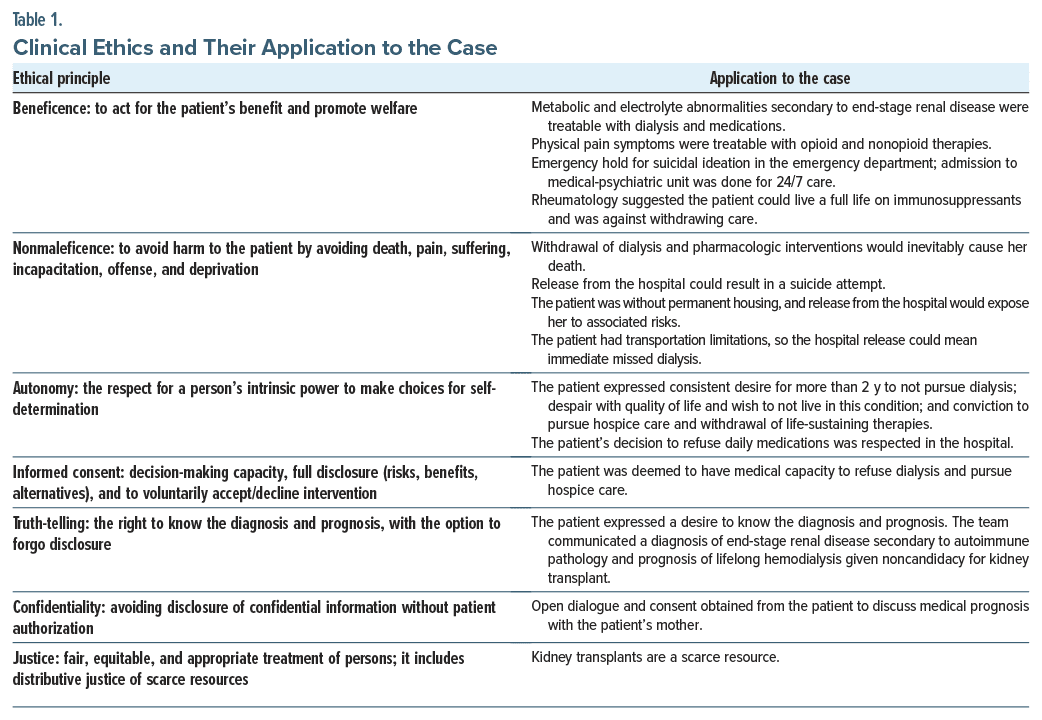
We differentiated demoralization from anhedonia by weighing her feelings of “subjective incompetence,” self-reproach, and having a death wish. Using the ethical framework provided in Table 1, within the ethical principle of autonomy, we established the patient’s persistent despair and multiple-year desire not to pursue dialysis and honored her decision to refuse daily medication and her conviction to pursue hospice care after withdrawing hemodialysis. While grappling with the principle of nonmaleficence, we established that release from the hospital would expose her to unstable transport and housing and continued worsening of pathology, with missed dialysis sessions leading to death; however, conversely, forced interventions would expose her to significant psychological trauma.
Medical beneficence focuses on minimizing risk and maximizing longevity, so treatment refusal can seem irrational to physicians. Notably, the value proposition of “health” is different for each patient and is not the only core value that patients consider. This rational decision takes precedence over emotion, which is championed by scientists and philosophers alike. Beneficence cannot override our patient’s autonomy, the principle of nonmaleficence, and the demonstrated principle of informed consent.6 In our patient’s case, it was morally permissible to afford her palliative medication and withdrawal of dialysis, as our intent was to relieve her existential/psychological pain and not cause her demise.7,8
In decisions involving life sustaining treatment withdrawal, psychiatrists play an important role in assisting with decision-making capacity assessment, mood disorder symptoms, and interdisciplinary discussions. These decisions may promote “moral distress,” when physicians must respect a patient’s autonomy to withdraw from life sustaining treatment, effectively ending life and requiring careful and compassionate debrief.9 We recommend having a low threshold to involving ethical committees in such cases. Future complex ethical dilemmas would benefit from our proposed ethical framework, which we used to make a patient-centered informed decision.
Article Information
Published Online: July 9, 2024. https://doi.org/10.4088/PCC.24cr03715
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(4):24cr03715
Submitted: February 3, 2024; accepted March 27, 2024.
To Cite: Gaba A, Munjal S. “I don’t want to live like this anymore”: the role of psychiatry and clinical ethics in withdrawing life-sustaining treatment. Prim Care Companion CNS Disord. 2024;26(4):24cr03715.
Author Affiliations: Wake Forest University School of Medicine, Winston-Salem, North Carolina (Gaba, Munjal); Department of Psychiatry, Wake Forest University School of Medicine, Winston-Salem, North Carolina (Munjal).
Corresponding Author: Arlen Gaba, BS, Wake Forest University School of Medicine, 1 Medical Center Blvd, Winston-Salem, NC 27157 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Additional Information: Patient identity has been anonymized, and details have been modified in the text such that patient anonymity remains preserved.
References (9)

- Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry. 2002;36(6):733–742. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision. American Psychiatric Association Publishing; 2022.
- de Figueiredo JM. Depression and demoralization: phenomenologic differences and research perspectives. Compr Psychiatry. 1993;34(5):308–311. PubMed CrossRef
- Wetzel RD, Margulies T, Davis R, et al. Hopelessness, depression, and suicide intent. J Clin Psychiatry. 1980;41(5):159–160. PubMed
- Breitbart W, Rosenfeld B, Pessin H, et al. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA. 2000;284(22):2907–2911. PubMed CrossRef
- Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17–28. PubMed
- Quinn WS. Actions, intentions, and consequences: the doctrine of double effect. Philos Public Aff. 1989;18(4):334–351. PubMed
- McLachlan HV. The ethics of killing and letting die: active and passive euthanasia. J Med Ethics. 2008;34(8):636–638. PubMed CrossRef
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite