Prim Care Companion CNS Disord 2023;25(2):22cr03287
To cite: Alli-Balogun O, Singh G, Korenis P. Intentional foreign body ingestion in a patient with borderline personality disorder and other comorbidities. Prim Care Companion CNS Disord. 2023;25(2):22cr03287.
To share: https://doi.org/10.4088/PCC.22cr03287
© 2023 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry, Bronx Care Hospital System, New York, New York
bSri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India
*Corresponding author: Omobolanle Alli-Balogun, MD, MPH, BronxCare Health System, 1276 Fulton Ave, Bronx, New York, NY 10456 ([email protected]).
Intentional foreign body ingestion (IFBI) is rarely seen among the psychiatric population and is a form of self-destructive behavior. Objects most commonly ingested include, but are not limited to, pens, nuts and screws, toothbrushes, eating utensils, razor blades, and various other metal objects.1 The presence of foreign bodies found in patients’ intestines was first reported by Baudamont in 1779,2 being seen in psychiatric patients and in those with no psychiatric history. A study by Palta et al3 involving 262 cases of foreign body ingestions found 92% of cases were intentional, 85% were psychiatric patients, and 84% of cases were seen in individuals who had a previous history of ingestion.
Research has shown an association of IFBI with a diagnosis of borderline personality disorder (BPD),4 which carries an estimated lifetime prevalence of 1% in the general population and 22% in the inpatient psychiatric population.5 For a definitive diagnosis of BPD, the DSM-5 requires at least 5 of the following criteria to be present: unstable interpersonal relationships, attempts to avoid abandonment, recurrent suicidal or self-destructive behavior, reckless impulsivity, unstable mood or affect, persistent unstable self-image, chronic feelings of emptiness, struggling with anger management, or transient paranoia or dissociative symptoms.4 Patients with BPD commonly exhibit self-harming behavior, with 80% of patients acting upon eventual self-harm and over two-thirds making at least one suicide attempt.6 This association of personality disorder with repeated ingestion of foreign objects and self-mutilation was first described in 1950 by Carp.7
IFBI can be challenging to treat because these patients can place a considerable burden on hospital resources and time. A retrospective case study of 33 patients was conducted in which 305 cases of IFBI were identified.8 Of these patients, 79% were psychiatrically diagnosed, resulting in a total cost of over $2 million.8 The average cost of a single patient with IFBI per hospital visit is $6,616 in the US and $2,305 in Canada, with an average inpatient admission duration of stay of 5.66 days.9
A lot of consideration is required from various specialties that partake in the management of a patient with IFBI, including emergency, psychiatry, surgery, nursing, and other hospital staff. The removal of foreign bodies ultimately falls on gastroenterologists. It is believed that 80%–90% of ingested foreign objects spontaneously pass through the gastrointestinal tract; however, 10%–20% require endoscopic intervention. In a few instances, surgery may be necessary.10,11
Furthermore, there is a lack of medical literature available discussing extensive evaluation and management of patients who continuously ingest foreign body objects from an in-depth psychiatric perspective in relation to psychiatric disorders. We present a case identifying BPD as the primary contributing factor associated with IFBI by a patient and demonstrate the psychiatric complexities associated with diagnostic treatment of self-injurious behavior.
Case Report
An 18-year-old homeless White female patient with a past psychiatric history of BPD, posttraumatic stress disorder, and major depressive disorder with anxious features and a past medical history of unspecified seizure disorder presented to the emergency department (ED) admitting to an attempted suicide overdose. She had taken 28 tablets of lithium 300 mg and 14 tablets of duloxetine 60 mg in front of shelter home staff, presenting to the ED 1 hour later. While in the ED she stated, “I have borderline personality disorder. I do impulsive things all the time. This wasn’t my first time, and it won’t be my last.”
Over the years, the patient had ingested razor blades, toothbrushes, pens, and paperclips. She had undergone multiple inpatient hospitalizations, repeated x-rays, and 6 endoscopic foreign body removals within the gastrointestinal tract.
The patient had a family history of substance abuse in her father, mother, and sister and had a younger brother diagnosed with cerebral palsy and autism. She had a history of sexual and physical abuse by her father. She reported a long history of sexual abuse by her father during her formative years. The patient required sutures to her genitalia for severe sexual trauma when she was age 10 and was removed from her home and placed in group homes until the age of 19.
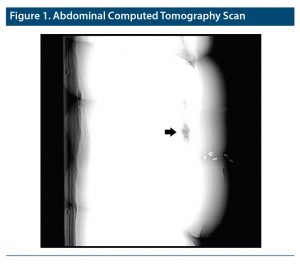
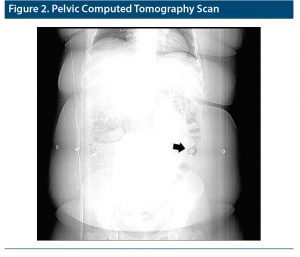
Over the course of the admission, the patient engaged in multiple episodes of swallowing objects. On one occasion after a physical altercation with a peer, she swallowed her toothbrush, which necessitated further medical evaluation. Blood panel results were consistent with microcytic anemia, and abdominal and pelvic computed tomography (Figure 1 and Figure 2) confirmed an obliquely oriented linear radiolucent structure within the gastric lumen measuring approximately 9 cm in length. Adjacent to the distal end of the radiolucent structure within the gastric body, a small linear metallic foreign body measuring 1.5 cm in length was also found.
The patient was prepared for endoscopy, during which a toothbrush was retrieved. She was stabilized and sent back to the unit. She was subsequently placed on 1:1 constant arm’s length supervision when she returned to her room.
The patient was subsequently stabilized and maintained on constant observation until the day of her discharge. She was prescribed oral levetiracetam 1,000 mg twice daily and ziprasidone 20 mg daily. No other form of recommended treatment, including dialectical behavior therapy or psychotherapy aimed at emotional regulation, was initiated due to patient noncompliance.
The DSM-5 criteria for BPD and the Zanarini Rating Scale for BPD12 were used to reassess the diagnosis for this patient. She met 5 of the 9 criteria and scored an 8 on the Zanarini scale, strongly indicating BPD. The patient exhibited the following: recurrent feelings of emptiness, inappropriate intense anger with recurrent physical fights with peers on the unit, past history of multiple hospital admissions for recurrent suicidal and self-mutilating behavior as seen with multiple scars in various stages of healing on the patient and actively inflicting self-harm while on admission, a pattern of unstable and interpersonal relationships with her peers and staff, and affective instability due to a marked reactivity of mood on the floor by constant irritability and splitting of staff.
Any additional information was gathered from past medical records and review of PSYCKES, a HIPAA-compliant web-based application service. The confirmation of BPD was critical and used in tandem with the patient’s IFBI to further solidify the diagnosis.
Discussion
When attempting to understand a patient with IFBI, all potential pathophysiologies must be considered and explored. IFBI is considered a form of self-injurious behavior and is parasuicidal—not with the intent of death but due to other underlying psychological conditions.13 It was suggested that self-harm behavior was used as a mechanism to relieve negative emotions or stress when the individual was not capable of doing so.14 This may explain self-harm that is nonsuicidal and be an underlying factor for seeking help or an attempt at a form of nonverbal communication.15 This might be a plausible explanation as to why our patient took an overdose in front of caregivers and would self-report her maladaptive behaviors. This repeated behavior can be linked to a history of childhood physical/sexual abuse and a history of abandonment,6 which was present in our patient.
IFBI can be categorized under the following diagnostic subgroups of psychiatric diagnoses: personality disorder, pica, psychosis, and malingering.16 Other psychiatric disorders can also be implicated in this behavior, such as autism spectrum disorder and obsessive-compulsive disorder.17,18
IFBI can be associated with personality disorders (ie, BPD, posttraumatic stress disorder),16 often alongside a history of physical and/or sexual abuse during childhood.16 The patient presented here had a repeated history of sexual abuse/trauma from the age of 3 until 10, requiring sutures to her genital area. Individuals with BPD demonstrate specific immature defenses based on Vaillant’s classification system: acting out, hypochondriasis, passive aggression, and projection.19 These immature defenses can bring about the following clinical behavior: impulsivity, demandingness, masochism, and suspiciousness,19 which can perpetuate the already established self-harming tendencies. Our patient presented all of the aforementioned symptoms and continues to demonstrate the need to seek attention and self-harm by informing the medical/shelter staff during the procedural act of ingestion.
Pica is defined as persistent eating of nonnutritive, nonfood substances over a period of 1 month that is inappropriate to the developmental level of the individual and part of a socially or culturally normative practice according to the DSM-5.20 It is often seen in micronutrient deficiencies (ie, iron deficiency anemia) or during pregnancy or is associated with intellectual disability. These nonnutritive foods include ice, dirt, clay, chalk, starch, hair, and metallic-made items.21,22 Treatment of pica must primarily focus on the correction of the nutritional deficiency and implementing behavioral interventions in those with developmental disabilities.23 Micronutrient deficiencies (iron) could be another plausible reason for our patient to ingest foreign substances but seems less likely in this case.
Psychosis can manifest as delusions, and the act of IFBI can be the result of a response to a command hallucination.24 Our patient conveyed no present or previous history of hallucinations, nor did any past medical records suggest otherwise.
Malingering is falsification or profound exaggeration of illness (physical or mental) with motivation usually being external.24 Potential external motivation, stimulated by seeking secondary gains, could include attempts to transfer to desired medical facilities or attempts to receive sympathetic treatment from the ward floor staff. Malingering is seen in populations of institutionalized psychiatric patients and does account for foreign body ingestion behavior.14 This could also be the case in our patient, as she repeatedly stated she wanted to be in a different hospital that met her socioeconomic demands and was more affiliated with her race.
Not every case of IFBI can be caused by an underlying psychiatric disorder. A differential diagnosis must be considered and is imperative to promptly address the possible cause. Potential nonpsychiatric diagnoses can include developmental disorders such as intellectual learning disability. People with learning disabilities are at greater risk of harm from putting non-nutritious items in their mouth, as it often leads to choking and in some instances death.25 Our patient did not present with any form of developmental disorder.
Management of patients with IFBI should focus on a multidisciplinary approach: developing and implementing a standardized protocol system when the patient is brought to the medical/psychiatric department, therapy-based treatment, and pharmacotherapy. A protocol must first be developed and implemented by treatment personnel to provide an effective streamlined approach to safe and effective management of the patient. These procedures must be in place once the patient is admitted to the unit floor. Some potential protocols that should be considered include the following:
- Patients should be labeled as high risk as soon as they are admitted to the unit.
- All objects that could be a potential for swallowing should be removed, and only food that does not require utensils should be served to patients on the unit.
- Patients should be placed on constant 1:1 arm’s length supervision.
- Complete blood workup for any micronutrient deficiencies and lead levels and treat accordingly.
- Regular precautional meetings with health care personnel including janitorial staff on the unit with routine reminders about the patient’s unpredictability.
Patients with BPD should be considered for dialectical behavior therapy (DBT). The American Psychological Association has recommended DBT treatment of more than 1 year for patients with BPD,26 with studies showing the most promise in individuals with self-injurious behavior.26 DBT focuses on reduction of posttraumatic stress, a sense of self-respect and achievement of life goals, and stability and security.27
Treatment of IFBI should also aim at decreasing impulsivity and frequency of self-harm.28 It has been suggested that self-harming behavior can be attributed to the involvement of the endogenous opioid system. A long-acting opiate antagonist (ie, naltrexone) would have a favorable outcome and show effective reduction of recurrent self-injurious behavior.28 The use of antipsychotics (ie, ziprasidone) has shown favorable results in patients who exhibit difficulty with impulse regulation29 and in the management of cognitive perceptual symptoms in individuals with BPD.30
Conclusion
This case highlights the complexities in managing patients that exhibit self-harming parasuicidal behavior in the form of IFBI. Establishing protocols and initiating effective pharmacotherapeutic treatment can assist patients in the management of their behavioral tendencies. Close monitoring allows for appropriate timely intervention and can help in reducing potential risk for the patient.
Published online: April 20, 2023.
Relevant financial relationships: None.
Funding/support: None.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (30)

- Yang ZM, Postma GN. Unlocking dysphagia: intentional ingestion of foreign bodies. Ear Nose Throat J. 2022;101(1):36–37. PubMed CrossRef
- Teimourian B, Cigtay AS, Smyth NP. Management of ingested foreign bodies in the psychotic patient. Arch Surg. 1964;88(6):915–920. PubMed CrossRef
- Palta R, Sahota A, Bemarki A, et al. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69(3 Pt 1):426–433. PubMed CrossRef
- Bangash F, Megna JL, Leontieva L. Deliberate foreign body ingestion in a 35-year-old woman with borderline personality disorder and several psychiatric comorbidities. Cureus. 2021;13(2):e13179. PubMed CrossRef
- Ellison WD, Rosenstein LK, Morgan TA, et al. Community and clinical epidemiology of borderline personality disorder. Psychiatr Clin North Am. 2018;41(4):561–573. PubMed CrossRef
- Navinés R, Gutierrez F, Arranz B, et al. Long-term and bizarre self-injurious behavior: an approach to underlying psychological mechanisms and management. J Psychiatr Pract. 2013;19(1):65–71. PubMed CrossRef
- Carp L. Foreign bodies in the gastrointestinal tracts of psychotic patients. Arch Surg (1920). 1950;60(6):1055–1075. PubMed CrossRef
- Huang BL, Rich HG, Simundson SE, et al. Intentional swallowing of foreign bodies is a recurrent and costly problem that rarely causes endoscopy complications. Clin Gastroenterol Hepatol. 2010;8(11):941–946. PubMed CrossRef
- Poynter BA, Hunter JJ, Coverdale JH, et al. Hard to swallow: a systematic review of deliberate foreign body ingestion. Gen Hosp Psychiatry. 2011;33(5):518–524. PubMed CrossRef
- Smith MT, Wong RK. Esophageal foreign bodies: types and techniques for removal. Curr Treat Options Gastroenterol. 2006;9(1):75–84. PubMed CrossRef
- Schwartz GF, Polsky HS. Ingested foreign bodies of the gastrointestinal tract. Am Surg. 1976;42(4):236–238. PubMed
- Zanarini MC, Weingeroff JL, Frankenburg FR, et al. Development of the self-report version of the Zanarini Rating Scale for Borderline Personality Disorder. Pers Ment Health. 2015;9(4):243–249. PubMed CrossRef
- Atluri D, Veluru C, Chopra A, et al. Recurrent intentional foreign body ingestion: an endoscopist’s dilemma. Gastroenterol Hepatol (N Y). 2012;8(7):482–484. PubMed
- O’Sullivan ST, Reardon CM, McGreal GT, et al. Deliberate ingestion of foreign bodies by institutionalised psychiatric hospital patients and prison inmates. Ir J Med Sci. 1996;165(4):294–296. PubMed CrossRef
- Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115(3):616–623. PubMed CrossRef
- Gitlin DF, Caplan JP, Rogers MP, et al. Foreign-body ingestion in patients with personality disorders. Psychosomatics. 2007;48(2):162–166. PubMed CrossRef
- Te Wildt BT, Tettenborn C, Schneider U, et al. Swallowing foreign bodies as an example of impulse control disorder in a patient with intellectual disabilities: a case report. Psychiatry (Edgmont). 2010;7(9):34–37. PubMed
- Stein DJ, Bouwer C, van Heerden B. Pica and the obsessive-compulsive spectrum disorders. S Afr Med J. 1996;86(suppl):1586–1588, 1591–1592. PubMed
- Zanarini MC, Weingeroff JL, Frankenburg FR. Defense mechanisms associated with borderline personality disorder. J Pers Disord. 2009;23(2):113–121. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. American Psychiatric Association; 2013.
- Mishori R, McHale C. Pica: an age-old eating disorder that’s often missed. J Fam Pract. 2014;63(7):E1–E4. PubMed
- Matson JL, Hattier MA, Belva B, et al. Pica in persons with developmental disabilities: approaches to treatment. Res Dev Disabil. 2013;34(9):2564–2571. PubMed CrossRef
- Klein CA. Intentional ingestion and insertion of foreign objects: a forensic perspective. J Am Acad Psychiatry Law. 2012;40(1):119–126. PubMed
- Alozai Uu, McPherson PK. Malingering. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- Thacker A, Abdelnoor A, Anderson C, et al. Indicators of choking risk in adults with learning disabilities: a questionnaire survey and interview study. Disabil Rehabil. 2008;30(15):1131–1138. PubMed CrossRef
- Petti TA, Blitsch M, Blix S, et al. Deliberate foreign body ingestion in hospitalized youth: a case series and overview. Adolesc Psychiatry. 2005;29:249–287.
- Griengl H, Sendera A, Dantendorfer K. Naltrexone as a treatment of self-injurious behavior: a case report. Acta Psychiatr Scand. 2001;103(3):234–236. PubMed CrossRef
- Scheltema Beduin A, de Haan L. Off-label second generation antipsychotics for impulse regulation disorders: a review. Psychopharmacol Bull. 2010;43(3):45–81. PubMed
- Wasylyshen A, Williams AM. Second-generation antipsychotic use in borderline personality disorder: what are we targeting? Ment Health Clin. 2016;6(2):82–88. PubMed CrossRef
- Wasylyshen A, Williams AM. Second-generation antipsychotic use in borderline personality disorder: what are we targeting? Ment Health Clin. 2016;6(2):82–88. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite