Abstract
Objective: Sexual dysfunction (SD) can interfere with sexual desire and satisfaction and is associated with an impairment in one’s emotional, mental, physical, and social function. Despite its importance, SD remains understudied in Lebanon, possibly due to its sensitive nature. Therefore, this research aimed to address this gap by examining the relationship between SD and certain psychological and behavioral factors. The objective was to investigate the relationship between SD and eating attitudes, depression, anxiety, and mindfulness among university students in Lebanon using a cluster analysis approach.
Methods: This cross-sectional study was carried out between July and September 2021. Using the snowball technique, a sample of 363 Lebanese university students was recruited. SD was measured using the Sexual Dysfunction Questionnaire, with higher scores indicating higher sexual arousal/desire. Eating attitudes, anxiety, depression, and mindfulness were measured using the Eating Attitude Test, Lebanese Anxiety Scale, Patient Health Questionnaire, and Freiburg Mindfulness Inventory, respectively.
Results: Participants were divided into 3 clusters: cluster 1 “moderate well being” (n = 109, 30.0%) was characterized by moderate eating attitudes, anxiety, depression, and mindfulness; cluster 2 “positive well-being” (n = 186, 51.2%) was characterized by having the lowest mean eating attitude, anxiety, and depression scores, while having the highest mean mindfulness score; and cluster 3 “negative well-being” (n = 68, 18.7%) was characterized by the highest mean eating attitude, anxiety, and depression scores, while having the lowest mean mindfulness score. Females compared to males (β = −0.87) and belonging to cluster 2 (β = −1.32) or cluster 3 (β = −1.32) were significantly associated with less sexual arousal.
Conclusion: The results align with previous findings suggesting that mindfulness has a role in SD. The current study highlights the importance of taking into consideration factors that interplay with SD. Mental health providers should consider integrating aspects of mindfulness into their practice when working with patients with SD. Additionally, addressing the taboo surrounding sexual health will be crucial to destigmatize this topic. The findings emphasize the need for accessible campaigns by sexual health organizations to raise awareness.
Prim Care Companion CNS Disord 2024;26(3):23m03682
Author affiliations are listed at the end of this article.
Sexual dysfunction (SD) can be defined as perturbations in sexual desires and one’s ability to feel sexual pleasure. It can be one of many different disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), such as delayed ejaculation, erectile disorder, female orgasmic disorder, and female sexual interest/arousal disorder.1 In a US representative sample, it was previously reported that SD is more prevalent among women (43%) compared to men (31%).2 Women with SD are more likely to have a lower quality of life and may suffer from both emotional and physical distress and a compromised social life.3 Furthermore, males suffering from erectile disorders have reported several psychosocial problems such as anxiety, depression, anger, frustration, poor self-esteem, guilt, lack of confidence, and limited intimacy.4
The 2 aspects of SD assessed in this study are arousal and desire. Sexual arousal can be explained by a subjective or physiological term; the first term refers to the individual’s personal perception of their level of sexual excitement in response to specific sexual stimuli, and the second would be, for example, genital vasocongestion. In men, physiological arousal starts with an erection.5 In women, the glands located on the sides of the vaginal orifice secrete mucus that makes intercourse more comfortable.6 Sexual desire can be described as when an individual thinks of or fantasizes about sexual behavior or is motivated to engage in sexual behavior regardless of immediate arousal.7 These 2 terms are present in 2 different disorders in the DSM-5-TR.1 Women with low desire experience a lack or decrease in sexual fantasies, which could cause distress. Those with low arousal would have a reduction in vaginal lubrication as well as genital warmth related to blood flow.8
SEXUALITY AMONG UNIVERSITY STUDENTS IN LEBANON
In Middle Eastern societies, most discussions of sexual health are considered taboo.9 Furthermore, inadequate sex education, religious restrictions, and sociocultural factors tend to affect views on sexuality.10 As a result, young people are not always equipped with the knowledge they need to take charge of their sexual health,11 since they attain their sexual knowledge from their peers and the media rather than older individuals.12,13 Additionally, they perceive risk differently than older adults14 and start engaging in risky behaviors at an early age.15
Data about sexual behavior among youth in Lebanon are scarce. In a previous survey conducted in 2007 among Lebanese university students,16 the majority of men (73.3%) and a small number of women (21.8%) disclosed having engaged in sexual interactions. The majority of men (86.1%) had used condoms, whereas the majority of women (75.6%) had not used any kind of contraception.16 It is important to interpret these results with caution. The higher percentage of male students engaging in sexual interactions and using contraceptive methods may reflect cultural factors that could have influenced the participants’ responses. Moreover, most women in the 2007 survey were from public universities, and lower socioeconomic status tends to be associated with higher levels of religiosity among young Lebanese adults. According to a prior study from 2016, a sizable fraction of university students in Lebanon had engaged in sexual behavior either once or frequently (20%).17 Additionally, males are more involved in sexual activity,16 since female virginity is generally considered more important both worldwide18 and in Arab countries.19
Due to the sensitivity of the topic in Lebanon, the lack of clinical time among professionals, and the scarcity of effective treatments, sexual health is a difficult subject to address among mental health providers.20 However, it is crucial to be aware of sexual health/SD, particularly among university students, since inadequate education and care could result in both physical and psychological problems later on in life.21 Therefore, studies on sexual function as such are crucial since they increase awareness, which then allows for the establishment of SD prevention strategies and treatment modalities.22
SD AND EATING DISORDERS
A decrease in sexual interest may be prevalent in people with eating disorders such as anorexia nervosa.23 People diagnosed with eating disorders may use inappropriate eating behaviors to stabilize or reduce body weight.24 Inappropriate eating behaviors can be expressed by restricting diets for prolonged periods, using laxatives, self-induced vomiting, etc.25 Eating habits change interindividually wherein inappropriate habits can also vary from dieting to eating excessively.26 In Lebanon, 23.8% of adults27 and 47.6% of male adolescents28 presented inappropriate eating attitudes. It is an established understanding within the field of psychology and psychiatry that these behaviors can be indicators of underlying eating disorders or disordered eating patterns.
Concerning gender differences, SD is higher in women with anorexia nervosa compared to those without eating disorders.29 Previous research suggests that women diagnosed with eating disorders have lower levels of sexual arousal, orgasm, and satisfaction in comparison with healthy women. Additionally, the multiple linear regression analysis revealed that body image concerns were associated with SD in individuals with anorexia nervosa restricting type.30 Research on sexuality and eating pathology in males is relatively nonexistent. There is evidence to suggest that nonheterosexual men are at a greater risk of developing an eating disorder.31–33 Men who are confused about their sexual orientation may seek refuge in weight loss and restricted eating. Physiological changes can occur in men after losing weight in which testosterone levels can decrease, leading in some cases to asexuality, which in turn helps them avoid the sexual orientation confusion.34
Literature suggests that eating disorders such as anorexia nervosa are usually accompanied by psychological interferences affecting biological drives, such as sexual desire, making one more vulnerable to experiencing SD.35 Hence, concerns about sexuality might exist in people with eating disorders, and higher levels of SD might be present in that population.36,37 Sexual experience includes a synergy of psychological, social, and biological factors.38 As individuals with anorexia lose more weight, they are more likely to have decreased sexual satisfaction and face difficulties in their sexual relationships.39,40 Furthermore, women with eating disorders such as anorexia nervosa and bulimia nervosa had lower levels of sexual arousal and satisfaction and had more sexual pain compared to control women.30 Difficulties in sexual functioning, sexual pain, and distress were associated with eating disorders.41
SD, ANXIETY, AND DEPRESSION
SD and sexual problems have been associated with many psychological disorders, such as major depressive disorder,42 panic disorder,43 obsessive-compulsive disorder,44 and posttraumatic stress disorder.45 A high prevalence of SD and a decrease in sexual desire have been found among patients with major depressive disorder.46 Additionally, reduced sexual activity and satisfaction can trigger depressive symptoms.47 Patients have attributed depression and suicidal ideation to the fact that they have SD and that they feel they cannot satisfy their partners.48 Furthermore, Kendurkar and Kaur49 found that subjects with a generalized anxiety disorder had lower sexual desire. Additionally, subjects with social phobia were more likely to suffer from SD.50
Due to limited specific research, further tailored studies are necessary to shed light on the actual mechanisms linking SD to depression and anxiety. However, lowered libido is part of the clinical presentation in depression.51 This indicates that sexual desire is impacted, aligning with the discovery of hypoactive dopaminergic mesolimbic circuits in individuals experiencing depression.52 Finally, an increased amygdala and medial orbitofrontal cortex activity, coupled with a decreased activity in the hypothalamus found in depressed patients, could potentially explain their lowered sexual desire and arousal.53–55
Imaging studies in patients suffering from anxiety consistently reveal an overactive amygdala response to threats and a reduced connectivity between emotion processing and regulatory areas such as the medial and dorsolateral prefrontal cortex, rostral anterior cingulate cortex, and hippocampus.56 These patients will suffer from marked distraction from arousing cues and fantasies, often favoring intrusive thoughts such as concerns about erection in men, even without affecting penile tumescence.57 Moreover, previous research has established a connection between anxiety and psychogenic erectile dysfunction, as well as premature ejaculation, primarily attributed to the peripheral sympathetic flow responsible for the fight-or-flight response, which leads to increased smooth muscle tone and vasoconstriction.58
SD AND MINDFULNESS
Mindfulness might contribute to healthy sexual outcomes, as living in the present moment and being aware of the surroundings activate effective emotional regulation and intentional actions.59 Mindfulness refers to a mental stage in which all attention is focused on the here and now or the present moment in a nonjudgmental attitude.60 The contributions of mindfulness-based therapies are believed to help individuals with SD in regard to their negative beliefs about sexuality,61 and those who practiced mindfulness were shown to score higher on SD scales.62 Thus, mindfulness interventions could reduce sexual distress.63,64
SD AND SOCIODEMOGRAPHIC CHARACTERISTICS
Little to no empirical evidence exists about the association of socioeconomic status with SD. Lower socioeconomic status has been associated with lower sexual frequency,65 but data to date are limited to studies in the West, and the scientific literature has not addressed this association in youth specifically in Middle Eastern countries.
Women with anorexia nervosa often express difficulties in their sexual encounters.40 These worries are not yet prioritized in the Lebanese community, as in a study conducted in Lebanon, women found it difficult to talk about their sexual desires or problems because they did not have the confidence or awareness to do so.66 In youth, studies on sexual health have primarily focused on risk reduction and prevention. This is especially true for the Lebanese youth since addressing sexual topics is often considered a sensitive conversation.67
CURRENT STUDY
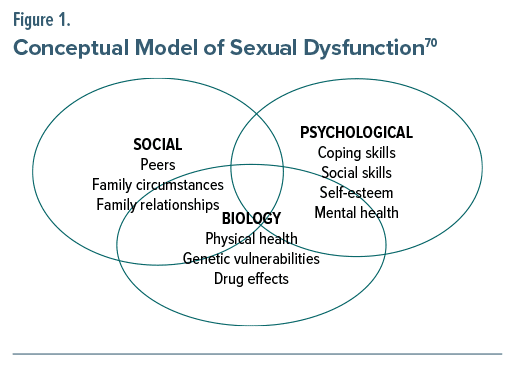
McCarthy and McDonald68 proposed that the treatment of SD should employ a “psychobiosocial model” that “emphasizes that sexuality is a multi-causal, multi dimensional, complex phenomenon,” warranting psychological, social, and biological treatment strategies.68 This model inspired us to take into consideration psychological aspects to explain the association between SD and psychological and behavioral factors such as (1) mental health, including psychological distress (depression and anxiety) and disordered eating (inappropriate eating attitude), and (2) coping skills such as mindfulness69 (Figure 1).
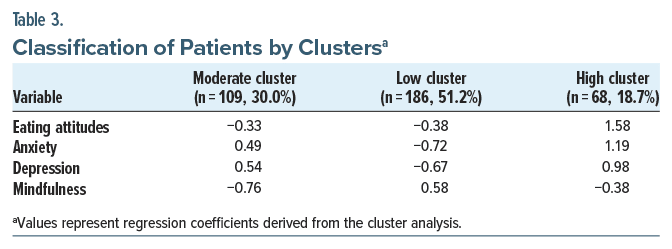
We divided the sample into 3 clusters ranging from the low cluster with the lowest eating attitude, anxiety, and depression scores, but the highest mindfulness score, to the high cluster with the highest eating attitude, anxiety, and depression scores, but the lowest mindfulness score. This is the first study, to our knowledge, to gather these factors into distinct groups, leading to reduced complexity of the available SD data. Our analysis provides a structured approach to decision making. By grouping these psychological factors, it became easier to analyze and make decisions based on the characteristics and behavior of each cluster.
To date, the data are scarce when it comes to studying risk factors in young adults since SD is often regarded as a condition that affects those who are older.40 On a mental health level, a high level of stigmatizing behaviors and attitudes has been found among a sample of Lebanese citizens toward mental illness.71 In a previous Lebanese study evaluating interpretations of sexual difficulties in women, several participants shared that they have difficulties communicating about their sexual desires because of a lack of awareness or confidence. Not being prepared for sexual life was also a concern for several women, who stated they did not learn about sexual arousal before marriage,66 hence the reason the current study evaluated both sexual desire and arousal in Lebanese students. Pre-COVID studies highlighted the high prevalence of mental health issues among Lebanese adults.72–74 The COVID pandemic increased anxiety in general,75 and at the same time, Lebanon is facing an economic crisis that has been associated with both anxiety and stress.76 The investigation of the associated factors with SD would help break new ground in Lebanon regarding sexual health, whereas in a representative adult sample in the United States, sexual health was rated as being important to the quality of life for 50% and 40% of sexually active men and women, respectively.77
Factors associated with SD have previously been investigated in Lebanon where anxiety and disordered eating attitudes were associated with lower sexuality composite scores in pregnant women.78 Another study17 aimed to investigate attitudes toward sexuality as well as sexual practices among Lebanese university students. However, no research has assessed associative factors of SD among Lebanese university students. With that being said, the current study aimed to examine the association of SD with eating attitudes, depression, anxiety, and mindfulness among Lebanese university students.
METHODS
Study Design and Participants
This cross-sectional study was carried out between July and September 2021. A total of 363 students from several universities were recruited through convenience sampling from all governorates in Lebanon (Beirut, Mount Lebanon, South, North, and Beqaa). Participants received an online link to the survey and were encouraged to visit a website that would guide them to the consent form, information form (purpose of the current study, anonymity, voluntariness of consent to research, and contact information in case they need to talk to someone outside the research), and questionnaire. The participants responded willingly to the anonymous survey, and no monetary compensation was given in exchange for participation. The respondents were informed about the objectives of the study and the right to withdraw at any time. The Psychiatric Hospital of the Cross Ethics and Research Committee approved this study protocol (HPC-007-2021). Informed consent to participate was obtained from all participants upon submission of the form online. All experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki).
All sexually active university students aged ≥18 years were eligible to participate in this study. Excluded were those aged <18 years, those who refused to participate in the study, and those who were not sexually active in the last 12 months.79–81 A minimum of 316 students was deemed necessary to have adequate statistical power, based on a 5% risk of error, 80% power, f2 = 2.5%, and 10 factors to be entered in the multivariable analysis.
Demographic and Physical Activity Questionnaire
The Arabic self-administered questionnaire included closed-ended questions and required approximately 20 minutes to be completed. The questionnaire consisted of several sections. The first part included questions about sociodemographic characteristics such as age, gender, marital status, educational level, and household crowding index (HCI). The purpose of the HCI was to reflect socioeconomic status of the participant and was calculated by dividing the number of people living in the home by the number of rooms in the home, excluding the bathrooms and kitchen.82 The physical activity index was calculated by multiplying the intensity by the frequency by the duration of physical activity.83 The body mass index was calculated by dividing weight by height squared, using the self-reported weight and height. Questions about history of COVID-19 infection and vaccination were recorded as well. The second part of the questionnaire included the following scales.
Sexual Dysfunction Questionnaire. Permission was obtained to use the Sexual Dysfunction Questionnaire (SDQ) in the study. The SDQ was forward and back translated. The forward translation (English to Arabic) was performed by 1 translator, whereas the back translation from Arabic to English was performed by a second translator. Minor discrepancies were solved by consensus. The SDQ consists originally of 19 questions rated on a 5-point Likert scale: always, often, sometimes, rarely, and never.84 Subjects were required to answer the statements based on experiences from the previous 12 months. We recoded the items so that higher scores would indicate higher sexual arousal/desire.
Eating Attitude Test. The Eating Attitude Test (EAT), validated in Lebanon,27 is used to assess disordered food attitude.85 The questionnaire comprises 26 questions each with 6 response options, varying from infrequently/almost never/never (0) to always (3). A score ≥20 indicates possible disordered eating attitudes85 (Cronbach α=0.943).
Lebanese Anxiety Scale. The Lebanese Anxiety Scale is a 10-item instrument measuring the severity of anxiety symptoms among Lebanese adults86 and adolescents.87 Higher scores indicate higher anxiety levels. The Cronbach α for the scale in this study was 0.89.
Patient Health Questionnaire-9. The Patient Health Questionnaire-9 is a short 9-item questionnaire used to screen for major depressive disorder.88 Higher scores indicate more severe depressive symptoms.88 The Arabic version of the scale was previously validated in Lebanon.89 The Cronbach α for this scale was 0.90.
Freiburg Mindfulness Inventory. The Freiburg Mindfulness Inventory, validated in Lebanon,90 is composed of 14 items describing all aspects of mindfulness such as attention to the present moment; nonjudgmental attitude; openness to one’s sensations, emotions, and thoughts; and insightful understanding.91 This instrument is used to characterize the person’s experience of mindfulness. Each item is scored based on a 4-point Likert scale with 1=rarely and 4=always. Higher total score indicates more mindfulness.92 The Cronbach α for this questionnaire was 0.91.
Statistical Analysis
SPSS software version 23 was used to conduct data analysis. We had no missing data since all questions were required to be answered via Google form. Cronbach α values were recorded for reliability analysis for all scales and subscales. A factor analysis using the “principal component analysis” technique of the SDQ items was conducted. The promax rotation was applied. The Kaiser-Meyer-Olkin (KMO) value and the Bartlett sphericity test ensured sampling adequacy. Factors with eigenvalues >1 were kept. Items with a factor loading <0.4 were removed.
As the current study has an exploratory design, we first conducted a hierarchical cluster analysis based on the Z scores for the scores on the whole sample, using the Ward method with Euclidean distance. The Ward method was suggested to be more appropriate for various types of data structures compared to other hierarchical algorithms, and the Euclidean distance, a commonly used distance measure, is known to be more suitable for numerical variables. The optimal number of clusters has been identified based on information from both agglomeration schedule and dendrogram. After the number of clusters was identified, K-means clustering was used to assign each individual to the identified clusters.93 The sexual desire/arousal scores were normally distributed, with their skewness and kurtosis values varying between −1 and +1.94 The Student t test and analysis of variance were used to compare 2 and 3 or more means, respectively, whereas the Pearson correlation test was used to compare 2 continuous variables. Two linear regressions were conducted afterward to check for correlates associated with sexual desire/arousal while adjusting the models over variables with a P < .25 as independent variables. Significance was set at P < .05.
RESULTS
Sociodemographic and Other Characteristics of the Participants
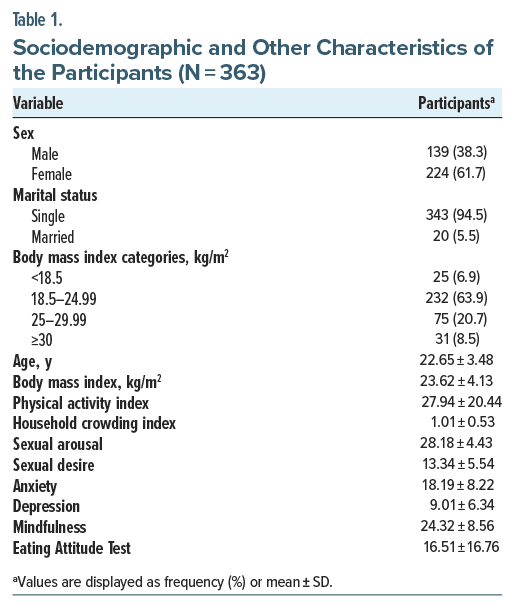
A total of 363 students participated in this study; their mean age was 22.65 ± 3.48 years, with 61.7% being female. Other characteristics are summarized in Table 1.
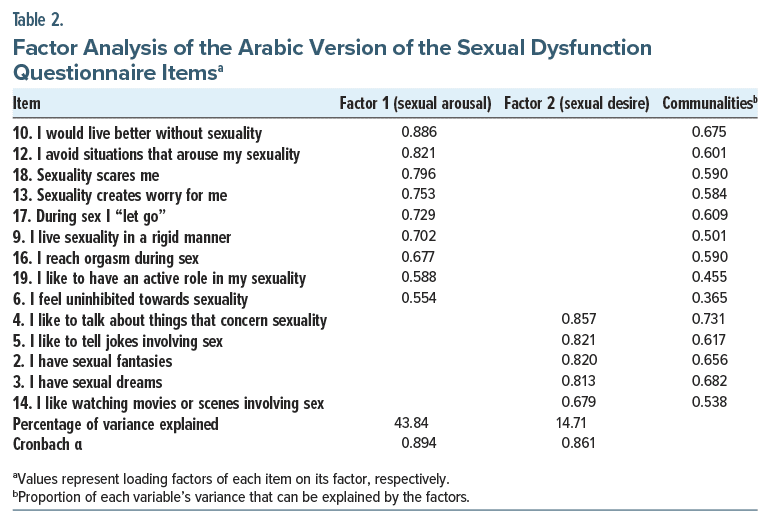
Factor Analysis
Items 7, 8, 11, and 15 were removed because of low factor loading (<0.4) in the original article.84 Item 1 was removed in this study because of low communality (<0.3). The other items converged over a solution of 2 factors (factor 1 = sexual arousal and factor 2 = sexual desire; total variance explained = 58.55%, KMO = 0.893; Bartlett test of sphericity P < .001). The Cronbach α in this study for sexual arousal was 0.894 and for sexual desire was 0.861 (Table 2).
Clusters
Data revealed the following groups. Cluster 1 or “moderate well-being” (n=109, 30.0%) was characterized by moderate eating attitudes, anxiety, depression, and mindfulness. Cluster 2 (n=186, 51.2%) had the lowest mean eating attitude, anxiety, and depression scores, while having the highest mindfulness mean score; this group was called “positive well-being.” The third cluster (n=68, 18.7%) was characterized by the highest mean eating attitude, anxiety, and depression scores, while having the lowest mindfulness mean score; thus, this group was labelled “negative well-being” (Table 3).
Bivariate Analysis
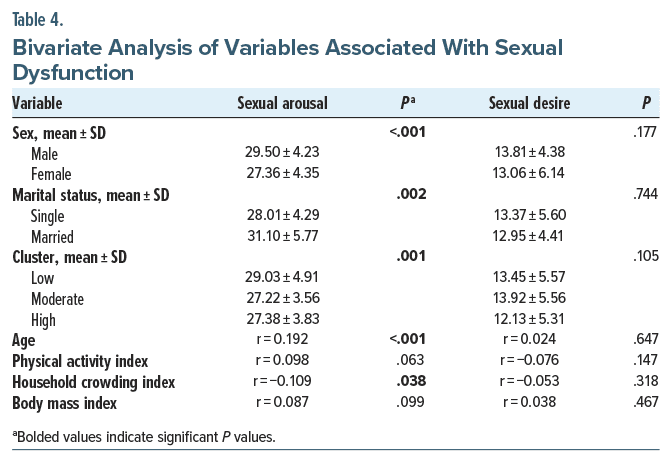
Males versus females and married versus single participants scored higher on sexual arousal. Older age and more mindfulness were significantly associated with more sexual arousal, whereas higher HCI, anxiety, and depression were significantly associated with less sexual arousal. Finally, higher EAT scores (more inappropriate eating) were significantly associated with less sexual desire (Table 4).
Multivariable Analysis
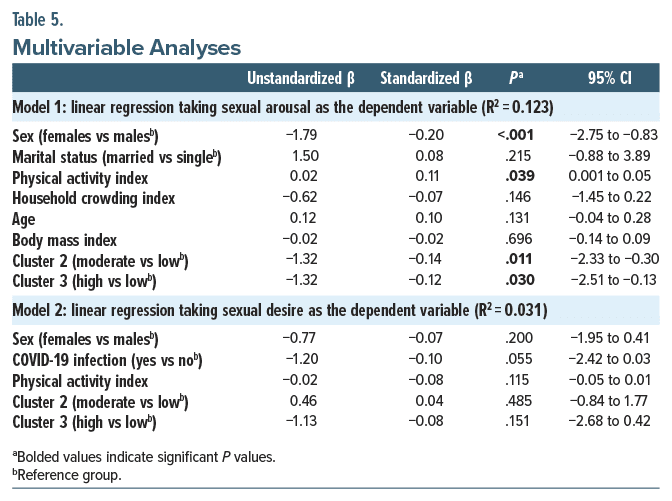
Females compared to males (β=−1.87) and belonging to cluster 2 (β=−1.32) or cluster 3 (β=−1.32) were significantly associated with less sexual arousal (Table 5, model 1). None of the variables was significantly associated with sexual desire (Table 5, model 2).
DISCUSSION
The present study investigated associations between inappropriate eating attitudes, anxiety, depression, and students. The results of this study indicate that older age and higher mindfulness scores were significantly correlated with more sexual arousal, whereas being a woman was associated with less sexual arousal. Higher EAT scores were associated with less sexual desire.
Mindfulness
In our study, a higher level of mindfulness was positively associated with sexual arousal. This is in line with the results of a meta-analysis of 11 publications that showed that mindfulness techniques can influence the reduction of SD symptoms.95 Moreover, another study96 showed that mindfulness can be an efficient treatment for sexual problems, and the results suggested that mindfulness could help individuals become more in tune with their body sensations. In this same study,96 women who underwent a mindfulness practice showed an improvement in their psychological barriers to interoceptive awareness wherein they enhanced their scores on self-judgment and attention. Moreover, these women showed an increase in self-acceptance and a decrease in judgment. This capability of being able to look at oneself or at their partner in a nonjudgmental way can be associated with healthier sexual well-being, which in turn contributes to sexual satisfaction.97 Previous research showed that mindfulness-based cognitive therapy was efficient in sexual functioning, desire, and arousal. The intervention was divided into 3 parts; the first 2 sessions were based on psychoeducation and relaxation training and body awareness, and the third session was being able to identify negative beliefs that individuals have about sexual image. The skills learned in the intervention were later used by the participants of the study to manage their SD.98 Additionally, the effects of mindfulness can be visible on a physiological level; mindfulness increases some neurotransmitters involved in regulating sexual behaviors. Hypoactive sexual desire disorder is characterized by an underactive activity of dopamine, which inhibits the activity of the latter to promote and facilitate sexual desire and arousal,99–102 and dopamine itself can increase to about 65% in limbic brain regions while using relaxation meditation.103
Eating Attitudes
Higher eating attitude scores were significantly associated with less sexual desire, which aligns with the findings of Pinheiro et al40 stating that SD is quite common among eating disorder patients. Additionally, research36 revealed that participants with bulimia nervosa were found to have an increase in their sexual drive while going through weight restoration. On another note, individuals with binge eating disorder were found to have lower sexual functioning than control subjects or people who do not have this disorder, where concerns about emotional eating and body shape were correlated with low sexual function.104 These difficulties in sexual functioning experienced by people with eating disorders can be explained by restrictive caloric dieting resulting in endocrine changes that can decrease vaginal lubrication, which would eventually cause painful penetration and distress.105
Age
Older age was positively associated with sexual arousal in the present study. A review of population-based studies found that sexual difficulties or dysfunctions decreased with age.106 There is no negative effect of biological aging on sexual desire when people are sexually healthy and satisfied.107 A previous survey revealed an increase in the proportion of sexually active 70-year-old individuals who consider sexuality as a positive force and are satisfied with their sexual life.108 No prior literature has evaluated the direct association of old age with sexual arousal, but previous data suggested a decrease in the prevalence of sexual arousal difficulties among sexually active women aged between 80 and 90 years.109 As previous research has found that the prevalence of erectile dysfunction treatment or diagnosis decreases in very old age,110 we hypothesize that the decrease of SD in old age can be explained by the increase in sexual arousal, a hypothesis that needs to be confirmed in future studies.
Gender
Women had less sexual arousal according to our results. This is in agreement with previous findings that showed that hypersexuality, characterized by sexual behavior beyond the normative range, occurred more frequently in males, with a male-to-female ratio of 5:1.111
Furthermore, it is worth noting that women were found to report lower levels of concern about sexual function.109 This can be explained by women being more likely to consider or report sex as not being crucial in their lives.112,113 It is important to note that, as already mentioned before, women’s comfort in reporting sexual arousal and desire is influenced by societal factors.
SD and Cultural Differences
As this study was conducted in a sample of Lebanese university students, results cannot be generalized to the entire Lebanese population nor to other Arab countries. The prevalence of SD may vary from one country to another, based on the findings of El-Sakka,114 where each country had a different prevalence of SD as well as different risk factors. In Egypt, smoking and the use of drugs were risk factors for SD. In Jordan, age, obesity, and smoking were found to be the main risk factors.114 The discrepancy in results may be due to cultural differences between each country. The same can be said about non-Arab cultures, especially as in Arab countries, such as in Lebanon, sexual topics are not often discussed in public or in private settings. Individuals tend to avoid discussing sexual difficulties with their partners, and this avoidance is also present between patients and their health care providers. In a Lebanese study,115 participants reported the avoidance attitude of discussing erectile dysfunction with their partner. The same study115 highlighted that only one-third (31%) of health providers initiated sexual health topics with their patients. In contrast, an American study116 showed that 79% of physicians felt comfortable asking about sexual history with their patients, and more than half of the participants asked about sexual activities. To further showcase cultural differences in sexual topics, a study117 conducted in Trinidad and Tobago showed that 50% of their participants would not ask patients about topics related to their sexuality. With that being said, one can hypothesize that sexual difficulties in Lebanon may be due to sociocultural aspects and not only biological factors.
Clinical Implications
The current study highlights the importance of taking into consideration factors that interplay with SD. Mental health providers might consider integrating aspects of mindfulness into their practice when working with patients with SD. As sexual health topics are still considered taboo, awareness sessions should be implemented to destigmatize them. Furthermore, based on the findings of the current study, organizations that deal with sexual health should implement accessible campaigns to raise awareness.
Limitations
Both information bias and selection bias were possible limitations in this study since the sample consisted of only university students. Furthermore, the SDQ was not previously validated in Arabic in Lebanon. Moreover, we cannot draw causalities due to the cross-sectional nature of this study. This study’s consideration of gender as binary without taking into account cisgender versus transgender identity is also a limitation. For a more thorough understanding of SD, future studies should acknowledge varied gender identities. Another limitation to be noted is that a residual confounding bias may be present given that some factors associated with SD such as medication intake118 were not considered in this study. Therefore, it would be highly recommended that future studies incorporate comprehensive assessments that encompass a range of factors and sociodemographic characteristics related to SD. Specifically, including questions to evaluate aspects such as the frequency of sexual intercourse, engagement in masturbation activities, and sexual orientation would be particularly valuable. This addition would shed light on the influence of these variables and contribute to a more comprehensive understanding of SD. However, the recruitment process was done anonymously, which may have allowed honest responses on sensitive topics in a conservative population.
CONCLUSION
Our study revealed significant findings regarding the relationships between mindfulness, age, and sexual arousal, indicating a positive correlation. We also found that women had reduced sexual arousal when compared to men. On another note, a negative association was found between inappropriate eating attitudes and sexual desire. The current study may be the first in Lebanon to evaluate factors associated with SD in university students. While acknowledging the limitations of our research, including the exclusion of certain factors associated with SD, we believe it will incite mental health practitioners to integrate mindfulness into their therapeutic approach when working with patients experiencing SD. Moreover, we hope our study will contribute to the implementation of awareness campaigns tackling sexual health, especially SD. Longitudinal studies that implement therapeutic techniques, such as mindfulness to manage SD, are warranted in the Lebanese population. Finally, future studies should consider evaluating other factors associated with SD such as religion119 and emotional intelligence.120
Article Information
Published Online: May 30, 2024. https://doi.org/10.4088/PCC.23m03682
© 2024 Physicians Postgraduate Press, Inc.
Submitted: December 14, 2023; accepted February 21, 2024.
To Cite: Sfeir M, Haidar S, El Khoury N, et al. Profiles of university students in terms of sexual dysfunction: the role of anxiety, depression, eating attitudes, and mindfulness. Prim Care Companion CNS Disord. 2024;26(3):23m03682.
Author Affiliations: Department of Clinical Psychology, University of Mons, Mons, Belgium (Sfeir); Department of Nutrition and Food Sciences, Faculty of Arts and Sciences, Lebanese International University, Beirut, Lebanon (Haidar); School of Medicine and Medical Sciences, Holy Spirit University of Kaslik, Jounieh, Lebanon (El Khoury, Hallit); Applied Science Research Center, Applied Science Private University, Amman, Jordan (Hallit); Social and Education Sciences Department, School of Arts and Sciences, Lebanese American University, Jbeil, Lebanon (Obeid).
Corresponding Authors: Souheil Hallit, PhD, Holy Spirit University of Kaslik, PO Box 446, Jounieh, Lebanon ([email protected]); Sahar Obeid, PhD, Social and Education Sciences Department, School of Arts and Sciences, Lebanese American University, Jbeil, Lebanon ([email protected]).
Drs Hallit and Obeid are last coauthors.
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors would like to thank all participants who helped us during this project.
Additional Information: All data generated or analyzed during this study are not publicly available due to the restrictions from the ethics committee (data are owned by a third-party organization). The dataset supporting the conclusions is available upon request to the corresponding author (Obeid).
ORCID: Suzan Haidar: https://orcid.org/0000-0001-7117-599X; Nour El Khoury: https://orcid.org/0009-0008-3815-4837; Souheil Hallit: https://orcid.org/0000-0001-6918-5689; Sahar Obeid: https://orcid.org/0000-0002-0735-4704
Clinical Points
- Females (compared to males), moderate well-being (cluster 2), and negative well-being (cluster 3) were significantly associated with less sexual arousal.
- The current study highlights the importance of taking into consideration factors that interplay with sexual dysfunction.
- Mental health providers should consider integrating aspects of mindfulness into their practice when working with patients with sexual dysfunction.
References (120)

- Cortés AS. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, Universidad Complutense de Madrid; 2022:339.
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281(6):537–544. PubMed CrossRef
- Giami A. Sexual health: the emergence, development, and diversity of a concept. Annu Rev Sex Res. 2002;13:1–35. PubMed
- Guest JF, Das Gupta R. Health-related quality of life in a UK-based population of men with erectile dysfunction. Pharmacoeconomics. 2002;20(2):109–117. PubMed CrossRef
- Calabrò RS, Cacciola A, Bruschetta D, et al. Neuroanatomy and function of human sexual behavior: a neglected or unknown issue? Brain Behav. 2019;9(12):e01389. PubMed
- Yucel S, De Souza A, Jr, Baskin LS. Neuroanatomy of the human female lower urogenital tract. J Urol. 2004;172(1):191–195. PubMed
- Buss DM, Schmitt DP. Sexual strategies theory: an evolutionary perspective on human mating. Psychol Rev. 1993;100(2):204–232. PubMed CrossRef
- Krakowsky Y, Grober ED. A practical guide to female sexual dysfunction: an evidence-based review for physicians in Canada. Can Urol Assoc J. 2018;12(6):211–216. PubMed CrossRef
- El-Kashif MML, El-tahry SE. A study of sexual dysfunction and its associated factors among women in childbearing age, Egypt. J Nurs Educ Pract. 2019;9(3):95–108.
- Hassanin IMA, Helmy YA, Fathalla MMF, et al. Prevalence and characteristics of female sexual dysfunction in a sample of women from Upper Egypt. Int J Gynaecol Obstet. 2010;108(3):219–223. PubMed CrossRef
- Lally K, Nathan-V Y, Dunne S, et al. Awareness of sexually transmitted infection and protection methods among university students in Ireland. Ir J Med Sci. 2015;184(1):135–142. PubMed CrossRef
- Salamé J, Barbour B, Salameh P. Do personal beliefs and peers affect the practice of alcohol consumption in university students in Lebanon. East Mediterr Health J. 2013;19(4):340–347. PubMed
- Primack BA, Switzer GE, Dalton MA. Improving measurement of normative beliefs involving smoking among adolescents. Arch Pediatr Adolesc Med. 2007;161(5):434–439. PubMed CrossRef
- Quadrel MJ, Fischhoff B, Davis W. Adolescent (in)vulnerability. Am Psychol. 1993;48(2):102–116. PubMed CrossRef
- Ismael AS, Sabir Zangana JM. Knowledge, attitudes and practice of condom use among males aged (15-49) years in Erbil Governorate. Glob J Health Sci. 2012;4(4):27–36. PubMed CrossRef
- Barbour B, Salameh P. Knowledge and practice of university students in Lebanon regarding contraception. East Mediterr Health J. 2009;15(2):387–399. PubMed
- Salameh P, Zeenny R, Salamé J, et al. Attitudes towards and practice of sexuality among university students in Lebanon. J Biosoc Sci. 2016;48(2):233–248. PubMed CrossRef
- Wilson KL, Smith ML, Menn M. Abstinence-related word associations and definitions of abstinence and virginity among Missouri High School Freshmen. J Sch Health. 2013;83(11):787–794. PubMed CrossRef
- AlQuaiz AM, Kazi A, Al Muneef M. Determinants of sexual health knowledge in adolescent girls in schools of Riyadh-Saudi Arabia: a cross sectional study. BMC Womens Health. 2013;13:19. PubMed CrossRef
- Wright JJ, O’Connor KM. Female sexual dysfunction. Med Clin North Am. 2015;99(3):607–628. PubMed CrossRef
- Higgins JA, Mullinax M, Trussell J, et al. Sexual satisfaction and sexual health among university students in the United States. Am J Public Health. 2011;101(9):1643–1654. PubMed CrossRef
- Halle-Ekane GE, Timti LF, Tanue EA, et al. Prevalence and associated factors of female sexual dysfunction among sexually active students of the University of Buea. Sex Med. 2021;9(5):100402. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disroders. 5th ed. American Psychiatric Association; 2013.
- Rodgers R, Chabrol H, Paxton SJ. An exploration of the tripartite influence model of body dissatisfaction and disordered eating among Australian and French college women. Body Image. 2011;8(3):208–215. PubMed CrossRef
- Gonçalves SF, Gomes AR. Exercising for weight and shape reasons vs. health control reasons: the impact on eating disturbance and psychological functioning. Eat Behav. 2012;13(2):127–130. PubMed
- Scaglioni S, De Cosmi V, Ciappolino V, et al. Factors influencing children’s eating behaviours. Nutrients. 2018;10(6):706. PubMed
- Haddad C, Khoury C, Salameh P, et al. Validation of the Arabic version of the Eating Attitude Test in Lebanon: a population study. Public Health Nutr. 2021;24(13):4132–4143. PubMed CrossRef
- Berro J, Akel M, Hallit S, et al. Relationships between inappropriate eating habits and problematic alcohol use, cigarette and waterpipe dependence among male adolescents in Lebanon. BMC Public Health. 2021;21(1):140. PubMed
- Price T, Zebitz M, Giraldi A, et al. Sexual function and dysfunction among women with anorexia nervosa: a systematic scoping review. Int J Eat Disord. 2020;53(9):1377–1399. PubMed CrossRef
- Castellini G, Lelli L, Lo Sauro C, et al. Anorectic and bulimic patients suffer from relevant sexual dysfunctions. J Sex Med. 2012;9(10):2590–2599. PubMed CrossRef
- Brown TA, Keel PK. The impact of relationships, friendships, and work on the association between sexual orientation and disordered eating in men. Eat Disord. 2013;21(4):342–359. PubMed CrossRef
- Boisvert JA, Harrell WA. Homosexuality as a risk factor for eating disorder symptomatology in men. J Mens Stud. 2010;17(3):210–225.
- Russell CJ, Keel PK. Homosexuality as a specific risk factor for eating disorders in men. Int J Eat Disord. 2002;31(3):300–306. PubMed CrossRef
- Morgan JF. The Invisible Man: A Self-Help Guide for Men With Eating Disorders, Compulsive Exercise and Bigorexia. Routledge; 2008.
- Zemishlany Z, Weizman A. The impact of mental illness on sexual dysfunction. Adv Psychosom Med. 2008;29:89–106. PubMed CrossRef
- Morgan JF, Lacey JH, Reid F. Anorexia nervosa: changes in sexuality during weight restoration. Psychosom Med. 1999;61(4):541–545. PubMed CrossRef
- Raboch J, Faltus F. Sexuality of women with anorexia nervosa. Acta Psychiatr Scand. 1991;84(1):9–11. PubMed
- Rösing D, Klebingat KJ, Berberich HJ, et al. Male sexual dysfunction: diagnosis and treatment from a sexological and interdisciplinary perspective. Dtsch Arztebl Int. 2009;106(50):821–828. PubMed
- Beumont PJ, Abraham SF, Simson KG. The psychosexual histories of adolescent girls and young women with anorexia nervosa. Psychol Med. 1981;11(1):131–140. PubMed CrossRef
- Pinheiro AP, Raney TJ, Thornton LM, et al. Sexual functioning in women with eating disorders. Int J Eat Disord. 2010;43(2):123–129. PubMed CrossRef
- Dunkley CR, Gorzalka BB, Brotto LA. Associations between sexual function and disordered eating among undergraduate women: an emphasis on sexual pain and distress. J Sex Marital Ther. 2020;46(1):18–34. PubMed
- Atlantis E, Sullivan T. Bidirectional association between depression and sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2012;9(6):1497–1507. PubMed CrossRef
- Figueira I, Possidente E, Marques C, et al. Sexual dysfunction: a neglected complication of panic disorder and social phobia. Arch Sex Behav. 2001;30(4):369–377. PubMed CrossRef
- Aksaray G, Yelken B, Kaptanoğlu C, et al. Sexuality in women with obsessive compulsive disorder. J Sex Marital Ther. 2001;27(3):273–277. PubMed CrossRef
- Letourneau EJ, Schewe PA, Frueh BC. Preliminary evaluation of sexual problems in combat veterans with PTSD. J Trauma Stress. 1997;10(1):125–132. PubMed CrossRef
- Williams K, Reynolds MF. Sexual dysfunction in major depression. CNS Spectr. 2006;11(8 Suppl 9):19–23. PubMed CrossRef
- Nicolosi A, Moreira ED, Jr, Villa M, et al. A population study of the association between sexual function, sexual satisfaction and depressive symptoms in men. J Affect Disord. 2004;82(2):235–243. PubMed CrossRef
- Rajkumar RP, Kumaran AK. Depression and anxiety in men with sexual dysfunction: a retrospective study. Compr Psychiatry. 2015;60:114–118. PubMed CrossRef
- Kendurkar A, Kaur B. Major depressive disorder, obsessive-compulsive disorder, and generalized anxiety disorder: do the sexual dysfunctions differ? Prim Care Companion J Clin Psychiatry. 2008;10(4):299–305. PubMed CrossRef
- Tignol J, Martin-Guehl C, Aouizerate B, et al. Social phobia and premature ejaculation: a case-control study. Depress Anxiety. 2006;23(3):153–157. PubMed CrossRef
- Laurent SM, Simons AD. Sexual dysfunction in depression and anxiety: conceptualizing sexual dysfunction as part of an internalizing dimension. Clin Psychol Rev. 2009;29(7):573–585. PubMed CrossRef
- Friedman A, Deri I, Friedman Y, et al. Decoding of dopaminergic mesolimbic activity and depressive behavior. J Mol Neurosci. 2007;32(1):72–79. PubMed CrossRef
- Anand A, Li Y, Wang Y, et al. Reciprocal effects of antidepressant treatment on activity and connectivity of the mood regulating circuit: an FMRI study. J Neuropsychiatry Clin Neurosci. 2007;19(3):274–282. PubMed CrossRef
- Opel N, Redlich R, Grotegerd D, et al. Prefrontal brain responsiveness to negative stimuli distinguishes familial risk for major depression from acute disorder. J Psychiatry Neurosci. 2017;42(5):343–352. PubMed CrossRef
- Yang J-C. Functional neuroanatomy in depressed patients with sexual dysfunction: blood oxygenation level dependent functional MR imaging. Korean J Radiol. 2004;5(2):87–95. PubMed CrossRef
- Pietrini F, Godini L, Lazzeretti L, et al. Neuroimaging and neurobiology of social anxiety. Riv Psichiatr. 2010;45(6):349–360. PubMed
- Beck JG, Barlow DH. The effects of anxiety and attentional focus on sexual responding--II. cognitive and affective patterns in erectile dysfunction. Behav Res Ther. 1986;24(1):19–26. PubMed CrossRef
- Corona G, Mannucci E, Petrone L, et al. Psycho-biological correlates of free floating anxiety symptoms in male patients with sexual dysfunctions. J Androl. 2006;27(1):86–93. PubMed CrossRef
- Karremans JC, Schellekens MP, Kappen G. Bridging the sciences of mindfulness and romantic relationships. Pers Soc Psychol Rev. 2017;21(1):29–49. PubMed CrossRef
- Bishop SR, Lau MA, Shapiro SL, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11(3):230–241.
- Jaderek I, Lew-Starowicz M. A systematic review on mindfulness meditation based interventions for sexual dysfunctions. J Sex Med. 2019;16(10):1581–1596. PubMed CrossRef
- Sánchez-Sánchez LC, Rodríguez MFV, García-Montes JM, et al. Mindfulness in sexual activity, sexual satisfaction and erotic fantasies in a non-clinical sample. Int J Environ Res Public Health. 2021;18(3):1161. PubMed
- Silverstein RG, Brown A-CH, Roth HD, et al. Effects of mindfulness training on body awareness to sexual stimuli: implications for female sexual dysfunction. Psychosom Med. 2011;73(9):817–825. PubMed CrossRef
- Brotto LA, Erskine Y, Carey M, et al. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol Oncol. 2012;125(2):320–325. PubMed CrossRef
- Kim JI, Zhu D, Davila J, et al. Female sexual dysfunction as measured by low sexual frequency is associated with lower socioeconomic status: an analysis of the National Health and Nutrition Examination Survey (NHANES), 2007-2016. J Sex Med. 2022;19(1):90–97. PubMed
- Azar M, Bradbury-Jones C, Kroll T. Middle-aged Lebanese women’s interpretation of sexual difficulties: a qualitative inquiry. BMC Womens Health. 2021;21(1):203. PubMed CrossRef
- Abu Ali RM, Al Hajeri RM, Khader YS, et al. Factors associated with sexual dysfunction in Jordanian women and their sexual attitudes. Ann Saudi Med. 2009;29(4):270–274. PubMed CrossRef
- McCarthy BW, McDonald DO. Psychobiosocial versus biomedical models of treatment: semantics or substance. Sex Relatsh Ther. 2009;24(1):30–37.
- Gibbons C, Morgan H. Mindfulness–as a coping strategy. Eisteach. 2015;15(2):14–18.
- Berry MD, Berry PD. Contemporary treatment of sexual dysfunction: reexamining the biopsychosocial model. J Sex Med. 2013;10(11):2627–2643. PubMed CrossRef
- El Hayek S, Cherro M, El Alayli A, et al. Stigma towards mental illness at an academic tertiary care center in Lebanon. Acad Psychiatry. 2021;45(6):725–732. PubMed CrossRef
- Obeid S, Akel M, Haddad C, et al. Factors associated with alexithymia among the Lebanese population: results of a cross-sectional study. BMC Psychol. 2019;7(1):80. PubMed CrossRef
- Obeid S, Akel M, Haddad C, et al. Factors associated with alcohol use disorder: the role of depression, anxiety, stress, alexithymia and work fatigue-a population study in Lebanon. BMC Public Health. 2020;20(1):245. PubMed CrossRef
- Obeid S, Lahoud N, Haddad C, et al. Factors associated with depression among the Lebanese population: results of a cross-sectional study. Perspect Psychiatr Care. 2020;56(4):956–967. PubMed CrossRef
- Sfeir M, Akel M, Hallit S, et al. Factors associated with general well-being among Lebanese adults: the role of emotional intelligence, fear of COVID, healthy lifestyle, coping strategies (avoidance and approach). Curr Psychol. 2022:1–10.
- El Othman R, Touma E, El Othman R, et al. COVID-19 pandemic and mental health in Lebanon: a cross-sectional study. Int J Psychiatry Clin Pract. 2021;25(2):152–163. PubMed CrossRef
- Flynn KE, Lin L, Bruner DW, et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. Adults. J Sex Med. 2016;13(11):1642–1650. PubMed CrossRef
- Gerges S, Obeid S, Hallit S. Associations between eating attitudes, mental health, and sexual dysfunction during pregnancy. J Sex Marital Ther. 2023;49(5):517–532. PubMed CrossRef
- Fekih-Romdhane F, Haddad P, Roukoz R, et al. Does loneliness mediate the association between social media use disorder and sexual function in Lebanese university students?. Int J Environ Health Res. 2024;34(3):1835–1846. PubMed
- Awad E, Hallit S, Obeid S. Does self-esteem mediate the association between perfectionism and mindfulness among Lebanese university students? BMC Psychol. 2022;10(1):256. PubMed CrossRef
- Fekih-Romdhane F, Sawma T, Obeid S, et al. Self-critical perfectionism mediates the relationship between self-esteem and satisfaction with life in Lebanese university students. BMC Psychol. 2023;11(1):4. PubMed
- Melki IS, Beydoun HA, Khogali M, et al. Household crowding index: a correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J Epidemiol Community Health. 2004;58(6):476–480. PubMed CrossRef
- Weary-Smith KA. Validation of the Physical Activity Index (PAI) As a Measure of Total Activity Load and Total Kilocalorie Expenditure During Submaximal Treadmill Walking, University of Pittsburgh; 2007.
- Infrasca R. Sexual Dysfunction Questionnaire: scale development and psychometric validation. J Psychopathol. 2011;17:253–260.
- Garner DM, Garfinkel PE. The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9(2):273–279. PubMed CrossRef
- Hallit S, Obeid S, Haddad C, et al. Construction of the Lebanese Anxiety Scale (LAS-10): a new scale to assess anxiety in adult patients. Int J Psychiatry Clin Pract. 2020;24(3):270–277. PubMed CrossRef
- Merhy G, Azzi V, Salameh P, et al. Anxiety among Lebanese adolescents: scale validation and correlates. BMC Pediatr. 2021;21(1):288. PubMed
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Dagher D, Samaha S, Mhanna M, et al. Depressive symptoms among a sample of Lebanese adolescents: scale validation and correlates with disordered eating. Arch Pediatr. 2023;30(6):401–407. PubMed CrossRef
- Bitar Z, Fekih Romdhane F, Rogoza R, et al. Psychometric properties of the short form of the Freiburg Mindfulness Inventory in the Arabic language. Int J Environ Health Res. 2023:1–12.
- Buchheld N, Grossman P, Walach H. Measuring mindfulness in insight meditation (Vipassana) and meditation-based psychotherapy: the development of the Freiburg Mindfulness Inventory (FMI). J meditation meditation Res. 2001;1(1):11–34.
- Walach H, Buchheld N, Buttenmüller V, et al. Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI). Personal Individ Differ. 2006;40(8):1543–1555.
- Yakın E, Obeid S, Fekih-Romdhane F, et al. “In-between orthorexia” profile: the co-occurrence of pathological and healthy orthorexia among male and female non-clinical adolescents. J Eat Disord. 2022;10(1):155–155. PubMed
- Hair JF, Jr, Hult GTM, Ringle CM, et al. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). Sage Publications; 2021.
- Stephenson KR, Kerth J. Effects of mindfulness-based therapies for female sexual dysfunction: a meta-analytic review. J Sex Res. 2017;54(7):832–849. PubMed CrossRef
- Arora N, Brotto LA. How does paying attention improve sexual functioning in women? A review of mechanisms. Sex Med Rev. 2017;5(3):266–274. PubMed CrossRef
- Leavitt C, Lefkowitz ES, Waterman EA. The role of sexual mindfulness in sexual wellbeing, relational wellbeing, and self-esteem. J Sex Marital Ther. 2019;45(6):497–509. PubMed CrossRef
- Bober SL, Recklitis CJ, Bakan J, et al. Addressing sexual dysfunction after risk reducing salpingo-oophorectomy: effects of a brief, psychosexual intervention. J Sex Med. 2015;12(1):189–197. PubMed CrossRef
- Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatr Clin. 2010;33(2):323–338.
- Pfaus JG. Reviews: pathways of sexual desire. J Sex Med. 2009;6(6):1506–1533. PubMed CrossRef
- Simon JA. Low sexual desire--is it all in her head? Pathophysiology, diagnosis, and treatment of hypoactive sexual desire disorder. Postgrad Med. 2010;122(6):128–136. PubMed CrossRef
- Stahl SM. Circuits of sexual desire in hypoactive sexual desire disorder. J Clin Psychiatry. 2010;71(5):518–519. PubMed CrossRef
- Kjaer TW, Bertelsen C, Piccini P, et al. Increased dopamine tone during meditation-induced change of consciousness. Brain Res Cogn Brain Res. 2002;13(2):255–259. PubMed CrossRef
- Castellini G, Mannucci E, Mazzei C, et al. Sexual function in obese women with and without binge eating disorder. J Sex Med. 2010;7(12):3969–3978. PubMed CrossRef
- Silva PD, Todd G. Sexual dysfunction in women with anorexia nervosa: nature and treatment. Sex Marital Ther. 1998;13(1):21–36.
- Hayes R, Dennerstein L. The impact of aging on sexual function and sexual dysfunction in women: a review of population-based studies. J Sex Med. 2005;2(3):317–330. PubMed CrossRef
- Kontula O, Haavio-Mannila E. The impact of aging on human sexual activity and sexual desire. J Sex Res. 2009;46(1):46–56. PubMed CrossRef
- Beckman N, Waern M, Ostling S, et al. Determinants of sexual activity in four birth cohorts of Swedish 70-year-olds examined 1971-2001. J Sex Med. 2014;11(2):401–410. PubMed
- Lee DM, Nazroo J, O’Connor DB, et al. Sexual health and well-being among older men and women in england: findings from the English longitudinal study of ageing. Arch Sex Behav. 2016;45(1):133–144. PubMed
- Mulhall JP, Luo X, Zou KH, et al. Relationship between age and erectile dysfunction diagnosis or treatment using real-world observational data in the USA. Int J Clin Pract. 2016;70(12):1012–1018. PubMed CrossRef
- Kafka MP. The paraphilia-related disorders: nonparaphilic hypersexuality and sexual addiction/compulsivity. In: Lieblum SR, Rosen RC, eds. Principles and practice of sex therapy. New York: Guilford Press; 2000:471–503.
- Bancroft J, Loftus J, Long JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32(3):193–208. PubMed CrossRef
- Laumann EO, Paik A, Glasser DB, et al. A cross-national study of subjective sexual well-being among older women and men: findings from the Global Study of Sexual Attitudes and Behaviors. Arch Sex Behav. 2006;35(2):145–161. PubMed CrossRef
- El-Sakka AI. Erectile dysfunction in Arab countries. Part I: prevalence and correlates. Arab J Urol. 2012;10(2):97–103. PubMed CrossRef
- El-Kak F, Jurdi R, Kaddour A, et al. Gender and sexual health in clinical practice in Lebanon. Int J Gynaecol Obstet. 2004;87(3):260–266. PubMed CrossRef
- Wimberly YH, Hogben M, Moore-Ruffin J, et al. Sexual history-taking among primary care physicians. J Natl Med Assoc. 2006;98(12):1924–1929. PubMed
- Rabathaly P, Chattu V. Sexual healthcare knowledge, attitudes, and practices among primary care physicians in Trinidad and Tobago. J Fam Med Prim Care. 2019;8(2):614–620. PubMed CrossRef
- Francis ME, Kusek JW, Nyberg LM, et al. The contribution of common medical conditions and drug exposures to erectile dysfunction in adult males. J Urol. 2007;178(2):591–596. PubMed CrossRef
- Che Ya SN, Muhamad R, Mohd Zain N, et al. Coping strategies for sexual problems and sexual dysfunction amongst Malay women with breast cancer. A qualitative study. Sex Med. 2021;9(3):100336. PubMed CrossRef
- Asadi L, Bokaie M, Khavari F, et al. Evaluation of the relationship between emotional intelligence and sexual function of reproductive age women. J Educ Health Promot. 2020;9:93. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite