ABSTRACT
Objective: The number of prescriptions for antidepressants in England has almost doubled in the past decade. The objective of this study was to examine if this growth and seasonal variation in prescribing rates of different antidepressants by general practice are linked.
Method: The number of prescriptions and quantity of antidepressants prescribed each month between January 1, 2014, and December 31, 2019 from the general practice prescribing data reports for each British National Formulary code and practice were analyzed. The data were aggregated to obtain the monthly total and analyzed to identify patterns by medication.
Results: We included all oral antidepressant medications prescribed in England in 2019 for a total of 74 million prescriptions, which was equivalent to 2.36 billion defined daily doses. Monthly variation in daily prescribing percentage of the annual average over the year in total and antidepressant medications showed small but generally consistent seasonal variation, an average of up to 1.61% in total items and 1.47% in defined daily dose (highest prescribing in November/December). The seasonality varied by agents, with agents having highest seasonality also showing the most growth (r2 = 0.5, P = .002). This relation was strongest for mirtazapine and sertraline. There was a clear relation between average seasonality and year on year growth in antidepressant medication prescribing for 2016–2019 (r2 = .536, P = .002).
Conclusions: The study confirmed seasonal variation in antidepressant prescribing with a peak in November/December. Growth in the antidepressant prescribing year on year was related to seasonality and requires further scrutiny in terms of understanding the factors that underlie the seasonal variation seen.
Prim Care Companion CNS Disord 2021;23(2):20m02790
To cite: Heald A, Stedman M, Farman S, et al. Seasonal variation in antidepressant prescribing: year on year analysis for England. Prim Care Companion CNS Disord. 2021;23(2):20m02790.
To share: https://doi.org/10.4088/PCC.20m02790
© Copyright 2021 Physicians Postgraduate Press, Inc.
aThe School of Medicine and Manchester Academic Health Sciences Centre, Manchester University, Manchester, United Kingdom
bRes Consortium, Research, Andover, United Kingdom
cMersey Deanery Psychiatry Rotation, United Kingdom
dSaint Petersburg State University, St Petersburg, Russia
eInstitute of Psychiatry, London, United Kingdom
*Corresponding author: Adrian Heald, DM, Department of Diabetes and Endocrinology, Salford Royal Hospital, Salford, UK M68HD ([email protected]).
Antidepressant medication is widely used in primary care. In a recent article,1 we considered how the quality of the patient-practice relationship influences the antidepressant prescribing rate in a primary care general practice in England. One factor not considered was the variation of use within the year, the “seasonality,” which may be a significant factor for local levels of prescribing to treat relatively short-term mood disorders.2,3 Seasonality is in the context of antidepressant prescribing increasing by an average of 4% each year.4
Previous work4 has described month-by-month antidepressant prescribing. Here, we provide an update in relation to the latest available data from England. Some mood disorders can be linked to reduced access to daylight, and our question was whether such seasonal changes link to the volume of antidepressants prescribed. For this analysis, we calculated the seasonality factor for each medication and determined if it could be used to describe the growth in their prescribing.
METHODS
We examined the way that agents licensed to treat major depressive disorder were prescribed in primary care between January 1, 2014, and December 31, 2019 (the National Health Service publishes these data monthly). The analysis was at a general practice level not at the level of individual patient data. Our focus was the month-to-month variation and to determine any patterns.
Monthly general practice prescribing data reports5 for each British National Formulary (BNF) code and practice6 and the prescriptions, quantity, and costs prescribed were examined for all general practices in England. Data from the Quality Outcomes Framework7 returns were utilized. We used the BNF drug name. The amount of active chemical in each item of the prescribed quantity was identified. Defined daily dose,8 which is the assumed average maintenance dose per the World Health Organization Annual Therapeutic Classification,8 was used to estimate the number of individuals on each therapy month on month during that period.
Data are collected from all registered primary care practices in England including some “dummy” practices, which are created to identify prescribing in environments or circumstances outside of general practice, such as specialist clinics, hospices, prisons, out-of-hours services, and training units. Other channels including hospital prescribers are not captured.
All items with a BNF code beginning with 04 (central nervous system) and 03 (antidepressant drugs) were included. To adjust for length of each month, we standardized the prescribing rate by the total number of days in each month including the 29 days in February of 2016 (leap year). To ensure that growth or decline was not a factor, the monthly amount was adjusted by the appropriate proportion of annual change to make all amounts equivalent to a midyear month.
Annual seasonality was then defined as the sum of prescribing in low daylight months in the calendar year (January to March + October to December)/days in the period (182) divided by long daylight months (April to September)/days in period (183). This method was applied to the total in each year and to the individual medications over the whole period. Since average annual growth compounds up over the 5-year period, it was calculated for each medication by dividing the number of prescriptions written in 2019 by those in 2014, taking the fifth root of this ratio and then subtracting 1 to give an annual average percentage increase. No ethics approval was needed, as all data are available and in the public domain.
RESULTS
We considered in detail the medication being prescribed in items, quantity, and defined daily doses during the study period from between 7,876 and 8,568 locations each month. There was little difference between the seasonality calculated using 3 measures, so items (number of prescriptions) was used as the metric.
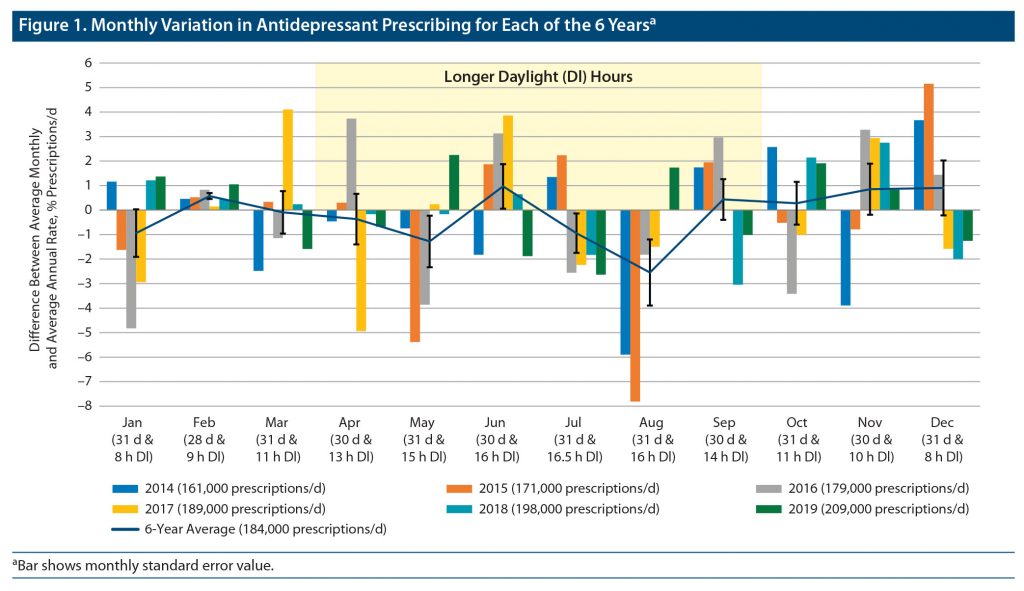
Monthly variation (Figure 1) was seen in daily prescribing, with the greatest number of prescriptions issued in November and December of each year and the consistent least number in August and July.
The overall average seasonal variation over the 6 years was 1% and was present in all years except 2016 (Figure 2A), wherein April and June were unusually high and January and October unusually low, which requires further investigation.
The top 15 antidepressants out of a total of 31 different medications included 99% of the total amount prescribed. The seasonality was apparent in all agents (Figure 2B). The greatest seasonality was apparent for mirtazapine (1.4%) and sertraline, with low seasonality for paroxetine and dosulepin.
There was a clear relation between average seasonality and year on year growth in antidepressant medication prescribing for 2014–2019, which is shown in Figure 3. The univariate analysis resulted in r2 = .536 (P = .002). The relation was strongest for mirtazapine and sertraline. Over the period examined, there was a decline in prescribing for clomipramine, dosulepin, and lofepramine.
DISCUSSION
Our study shows seasonal variation in antidepressant prescribing, with the peak in November/December and consistent trough in July/August, but also troughs in January and April/May. The seasonal variation was strongest for mirtazapine and sertraline and, if anything, is less than might be expected.
We recently described the pattern of antidepressant prescribing at the general practice (family doctor) level in England and found that selective serotonin reuptake inhibitors were the most prescribed class of antidepressants, with sertraline the most prescribed,9 in keeping with National institute for Health and Social Care Excellence10 guidance. Many factors may relate to the seasonal variation that we have seen, such as return to work after the summer vacation, start of the academic year in the United Kingdom (influencing not just students but their parents as well), and shortening in the length of the day and less clement weather in November/December in the United Kingdom.
We were unable to see new prescriptions, only all prescriptions. Thus, we cannot differentiate prescribing for new presentations versus longer-term prescribing. The small degree of seasonality that we have seen in overall prescribing may point to much greater seasonal variation in new prescriptions. One might expect more initiations in autumn and winter and more discontinuations in the lighter months. Also, something that may be relevant to look at would be light box sales—sales of light boxes to reduce the impact of seasonal affective disorder (SAD) may peak in September/October.
Our findings concerning the seasonal rise in antidepressant prescribing accord with the report of Gardarsdottir et al2 from the Netherlands. In a study population composed of adult patients initiating antidepressants, they found significant seasonality of initiating antidepressant use (higher in the winter months) in all patient groups, except within the age groups 18–30 years and > 60 years.2
The best evidence in terms of antidepressant use for the treatment of SAD is for the use of sertraline, citalopram, or fluoxetine.11 In SAD, it is usual to start antidepressants in the autumn and discontinue them in the spring, as we have seen here. Cochrane has recently reported that the best evidence for prevention of SAD symptoms is bupropion, although this agent is associated with a greater risk of headaches.12 We were unable to review new antidepressant prescriptions for this study. A recent Cochrane review13 looked at psychological therapy versus no treatment, or any other type of psychological therapy, light therapy, second-generation antidepressants, melatonin, agomelatine, or lifestyle changes to determine efficacy and safety of interventions to prevent SAD and determined that the evidence on psychological therapies to prevent the onset of a new depressive episode in people with a history of SAD is inconclusive. The review13 concluded that the treatment selected should be strongly based on patient preferences.
The relation between growth in the prescribing of antidepressants year on year and seasonality in prescribing has not been described previously. We speculate that this seasonal variation may occur because patients self-modulate their requirement for repeat prescriptions in the spring and summer months if they feel that things are going in the right direction
Limitations
We analyzed national prescribing data. However, this is at the general practice level, not the individual level. We were unable to view new prescriptions from England’s prescribing register. This capability would enhance the visibility of what is happening month to month in the general practices in relation to new presentations of depression or depression/anxiety of such nature and degree as to require pharmacologic intervention.
CONCLUSION
The results of this study confirm seasonal variation in antidepressant prescribing with a peak in November/December. The growth in antidepressant prescribing year on year and how this relates to the seasons merit further exploration.
Submitted: August 5, 2020; accepted October 30, 2020.
Published online: April 1, 2021.
Potential conflicts of interest: None.
Funding/support: None.
Additional information: Any requests for data extracts will be considered by Dr Heald ([email protected]) as the corresponding author. As publicly available and general practice–level data were used, with no individual patient data, it was not deemed necessary to seek ethics approval for this study.
Clinical Points
- The number of prescriptions for antidepressants in England has almost doubled in the past decade.
- Year on year, there was a small but generally consistent seasonal variation in antidepressant prescribing.
- The seasonality varied by medication, with agents having the highest seasonality also showing the most growth in the numbers of prescriptions.
References (13)

- Heald AH, Stedman M, Davies M, et al. Quantifying the impact of patient-practice relationship quality on the levels of the average annual antidepressant practice prescribing rate in primary care in England. Prim Care Companion CNS Disord. 2020;22(1):19m02528. PubMed CrossRef NLM
- Gardarsdottir H, Egberts TC, van Dijk L, et al. Seasonal patterns of initiating antidepressant therapy in general practice in the Netherlands during 2002-2007. J Affect Disord. 2010;122(3):208–212. PubMed CrossRef NLM
- Øverland S, Woicik W, Sikora L, et al. Seasonality and symptoms of depression: a systematic review of the literature. Epidemiol Psychiatr Sci. 2019;29:e31. PubMed CrossRef NLM
- Iacobucci G. NHS prescribed record number of antidepressants last year. BMJ. 2019;364:l1508. PubMed CrossRef NLM
- GP Practice Prescribing Presentation-level Data. NHS Digital. Accessed January 23, 2020. https://digital.nhs.uk/data-and-information/publications/statistical/practice-level-prescribing-data/december-2019
- British National Forumlary. National Institute for Health and Care Excellence. Accessed January 24, 2020. https://bnf.nice.org.uk/
- Quality and Outcomes Framework. NHS Digital. Accessed January 24, 2020. https://qof.digital.nhs.uk/
- ATC/DDD Index 2021. WHO Collaborating Centre for Drug Statistics Methodology. Accessed January 23,2020. https://www.whocc.no/atc_ddd_index/
- Heald AH, Stedman M, Davies M, et al. Antidepressant prescribing in England: patterns and costs. Prim Care Companion CNS Disord. 2020;22(2):19m02552. PubMed CrossRef NLM
- Depression Guidelines. National Institute for Health and Care Excellence. Accessed March 20, 2020. https://cks.nice.org.uk/depression
- Melrose S. Seasonal affective disorder: an overview of assessment and treatment approaches. Depress Res Treat. 2015;2015(S):178564. PubMed PubMed NLM
- Gartlehner G, Nussbaumer-Streit B, Gaynes BN, et al. Second-generation antidepressants for preventing seasonal affective disorder in adults. Cochrane Database Syst Rev. 2019;3(3):CD011268. PubMed NLM
- Forneris CA, Nussbaumer-Streit B, Morgan LC, et al. Psychological therapies for preventing seasonal affective disorder. Cochrane Database Syst Rev. 2019;5(5):CD011270. PubMed NLM
Please sign in or purchase this PDF for $40.
Save
Cite