Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Sleep disturbance could be the initial manifestation of bipolar disorder. We report a case of undiagnosed bipolar II disorder in a patient who presented to the sleep clinic with complaints of insomnia. Objective testing with actigraphy detected an irregular sleep-wake schedule and very little sleep time with extended periods of wakefulness and activity in a 2-week period during the hypomanic phase of bipolar disorder.
Sleep Disturbances in a Patient With Bipolar Disorder
To the Editor: Sleep disturbance could be the initial manifestation of bipolar disorder. We report a case of undiagnosed bipolar II disorder in a patient who presented to the sleep clinic with complaints of insomnia. Objective testing with actigraphy detected an irregular sleep-wake schedule and very little sleep time with extended periods of wakefulness and activity in a 2-week period during the hypomanic phase of bipolar disorder. To our knowledge, this is the first actigraphic illustration of sleep disturbances occurring during a hypomanic or manic episode.
Case report. Mr A, a 22-year-old male professional athlete, was referred to the sleep clinic with a complaint of trouble falling asleep, which began when he was in high school. He noted that the only thing that had helped his insomnia was marijuana. Insomnia and the accompanying marijuana use had put his career as a professional athlete at risk.
On interview, he noted an irregular sleep-wake pattern and stated that it was common for him to have periods of up to 40 hours of being awake. He denied daytime sleepiness, and his history was not suggestive of restless legs syndrome, narcolepsy, or sleep apnea. He had tried trazodone and melatonin to help with his sleep with no benefit. He denied drinking excessive amounts of alcohol or using other recreational drugs. He claimed that his last use of cannabis was 45 days prior to the visit, and the urine toxicology result was negative for illicit drugs.
On further questioning, he endorsed 5 prior depressive episodes, each lasting 2 weeks or longer, during which he experienced anhedonia, low energy, worsening anxiety, difficulty concentrating, and negative thoughts and a pessimistic outlook toward life. He acknowledged at least 2 episodes of 4 days each during which he experienced elevated mood, irritability, decreased need for sleep (typically sleeping 3 to 4 hours per day), heightened thought and speech velocity, easy distractibility, and an increase in goal-directed activity. He had not been previously diagnosed with any medical or psychiatric disorders and was not taking any medications. His body mass index was 39 kg/m2 and neck circumference was 43 cm. His blood pressure was within normal range, his oropharynx Friedman palate position was grade II, and examination of his cardiovascular and respiratory systems revealed no abnormalities. His mood was euthymic, his affect was mood-congruent and reactive, and there was no indication of thought disorder.
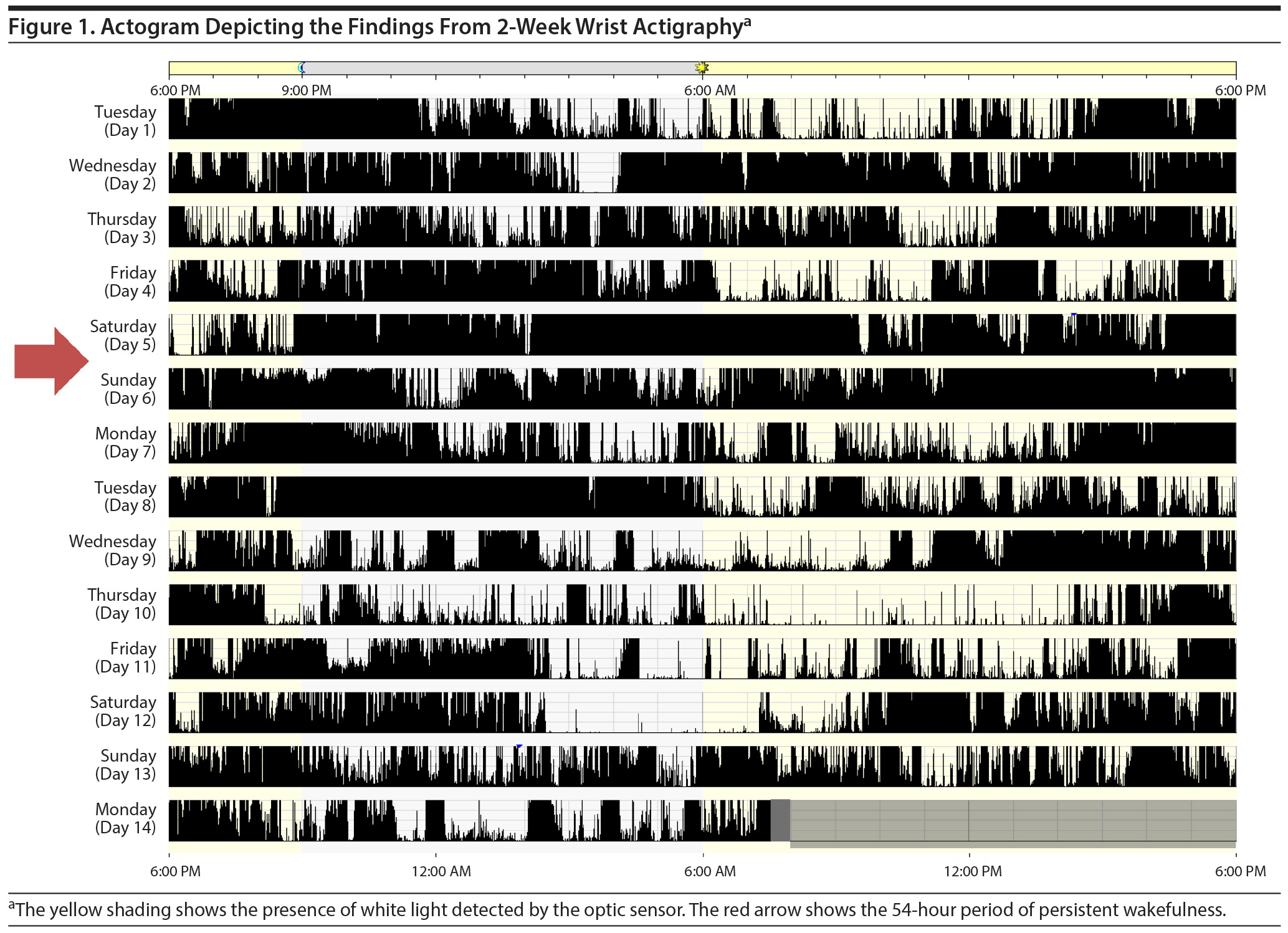
Two-week wrist actigraphy obtained just prior to the visit, as is customary at our tertiary-level sleep center for out-of-state referrals, revealed a mean sleep time of only 1 hour and 21 minutes (range, 0-8 hours and 7 minutes) and a very low sleep efficiency of 24.07% (range, 0%-95.47%; normal ≥ 85%) (Figure 1). The study demonstrated no consistent sleep time with some extended periods (including one of almost 54 hours’ duration) of continuous activity with no indication of sleep. In conjunction with the clinical history, it was thought that the erratic sleep schedule, significantly short sleep duration, and increased activity captured on actigraphy most likely represented a hypomanic episode.
Overnight polysomnography with the administration of zolpidem 10 mg conducted on the same date as the clinic visit to rule out sleep-disordered breathing and periodic limb movements of sleep revealed normal sleep with no evidence of these disorders. All laboratory tests including thyroid-stimulating hormone were within normal range. Following referral to a psychiatry mood clinic, the history was corroborated, and a diagnosis of bipolar II disorder was made on the basis of DSM-5 diagnostic criteria.1 The patient was started on medication and advised to follow up with his local psychiatrist.
We report the case of a patient with bipolar II disorder who presented to a sleep clinic with complaints of insomnia. Actigraphy detected decreased sleep time, prolonged wakefulness, and increased activity in a 2-week period during the hypomanic phase of bipolar disorder that helped confirm the diagnosis of bipolar II. To our knowledge, this has not been demonstrated on actigraphy before.
Subjective reports of sleep problems in patients with bipolar disorder are common, but objective assessments of sleep patterns are not widely performed in clinical practice.2 Actigraphy is a reliable and feasible method to evaluate sleep disturbances.3 Previous actigraphic studies4 of patients with bipolar disorder have not reported on the changes in sleep patterns associated with the manic or hypomanic phase of the disorder. A temporal association between sleep disturbance and mood changes has been noted in patients with bipolar disorder.5 A decrease in self-reported sleep duration, particularly by more than 3 hours from the usual sleep duration, has been shown to correlate with a shift toward mania or hypomania on the same or subsequent day. A systematic review6 of manic and depressive prodromes found that sleep disturbance is the most common prodrome of mania and is reported by approximately 77% of patients with bipolar disorder during the manic phase. However, insomnia and disrupted sleep patterns can persist between episodes as well. One study7 found a prevalence rate of 70% of clinically significant symptoms of sleep disturbance during the euthymic phase of bipolar disorder. Additionally, circadian alterations, commonly of an "evening" chronotype, have been described in patients with bipolar disorder.8 Finally, interventions that improve sleep such as interpersonal and social rhythm therapy have been shown to be effective in the management of bipolar disorder.9
Patients with bipolar II disorder could remain undiagnosed for years due to less severe symptom profiles. As in this case, patients may present to a sleep clinician first with complaints of sleep disturbance. A thorough investigation for a past history of symptoms suggestive of mania or hypomania or depression is warranted in these patients, as disrupted sleep could be a harbinger of a mood disorder. Although a detailed history remains the cornerstone of evaluation for mood disorders, the use of actigraphy to objectively evaluate sleep duration and physical activity may aid in the assessment of these patients.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders. Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
2. Bradley A, Webb-Mitchell R, Hazu A, et al. Sleep and circadian rhythm disturbance in bipolar disorder. Psychol Med. 2017;47(9):1678-1689. PubMed CrossRef
3. Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15(4):259-267. PubMed CrossRef
4. De Crescenzo F, Economou A, Sharpley AL, et al. Actigraphic features of bipolar disorder: a systematic review and meta-analysis. Sleep Med Rev. 2017;33:58-69. PubMed CrossRef
5. Bauer M, Grof P, Rasgon N, et al. Temporal relation between sleep and mood in patients with bipolar disorder. Bipolar Disord. 2006;8(2):160-167. PubMed CrossRef
6. Jackson A, Cavanagh J, Scott J. A systematic review of manic and depressive prodromes. J Affect Disord. 2003;74(3):209-217. PubMed CrossRef
7. Harvey AG, Schmidt DA, Scarn× A, et al. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. Am J Psychiatry. 2005;162(1):50-57. PubMed CrossRef
8. Melo MC, Abreu RL, Neto VBL, et al. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev. 2017;34:46-58. PubMed CrossRef
9. Crowe M, Beaglehole B, Inder M. Social rhythm interventions for bipolar disorder: a systematic review and rationale for practice. J Psychiatr Ment Health Nurs. 2016;23(1):3-11. PubMed CrossRef
aDepartment of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota
bCenter for Sleep Medicine, Mayo Clinic, Rochester, Minnesota
cDivision of Cardiovascular Diseases, Mayo Clinic, Rochester, Minnesota
Potential conflicts of interest: Dr Mansukhani is the principal investigator on a research grant funded by ResMed Corp that is unrelated to the current report. Drs Foroughi, Kolla, Saeidifard, and Altchuler report no conflicts of interest related to the subject of this report.
Funding/support: None.
Acknowledgment: This work was performed at Mayo Clinic, Rochester, Minnesota. Informed consent was obtained from the patient for use of the medical record for research, and research authorization is on file at Mayo Clinic. Information has been de-identified to protect anonymity.
Published online: June 14, 2018.
Prim Care Companion CNS Disord 2018;20(3):17l02213
To cite: Foroughi M, Kolla BP, Saeidifard F, et al. Sleep disturbances in a patient with bipolar disorder. Prim Care Companion CNS Disord. 2018;20(3):17l02213.
To share: https://doi.org/10.4088/PCC.17l02213
© Copyright 2018 Physicians Postgraduate Press, Inc.
Please sign in or purchase this PDF for $40.00.
Save
Cite