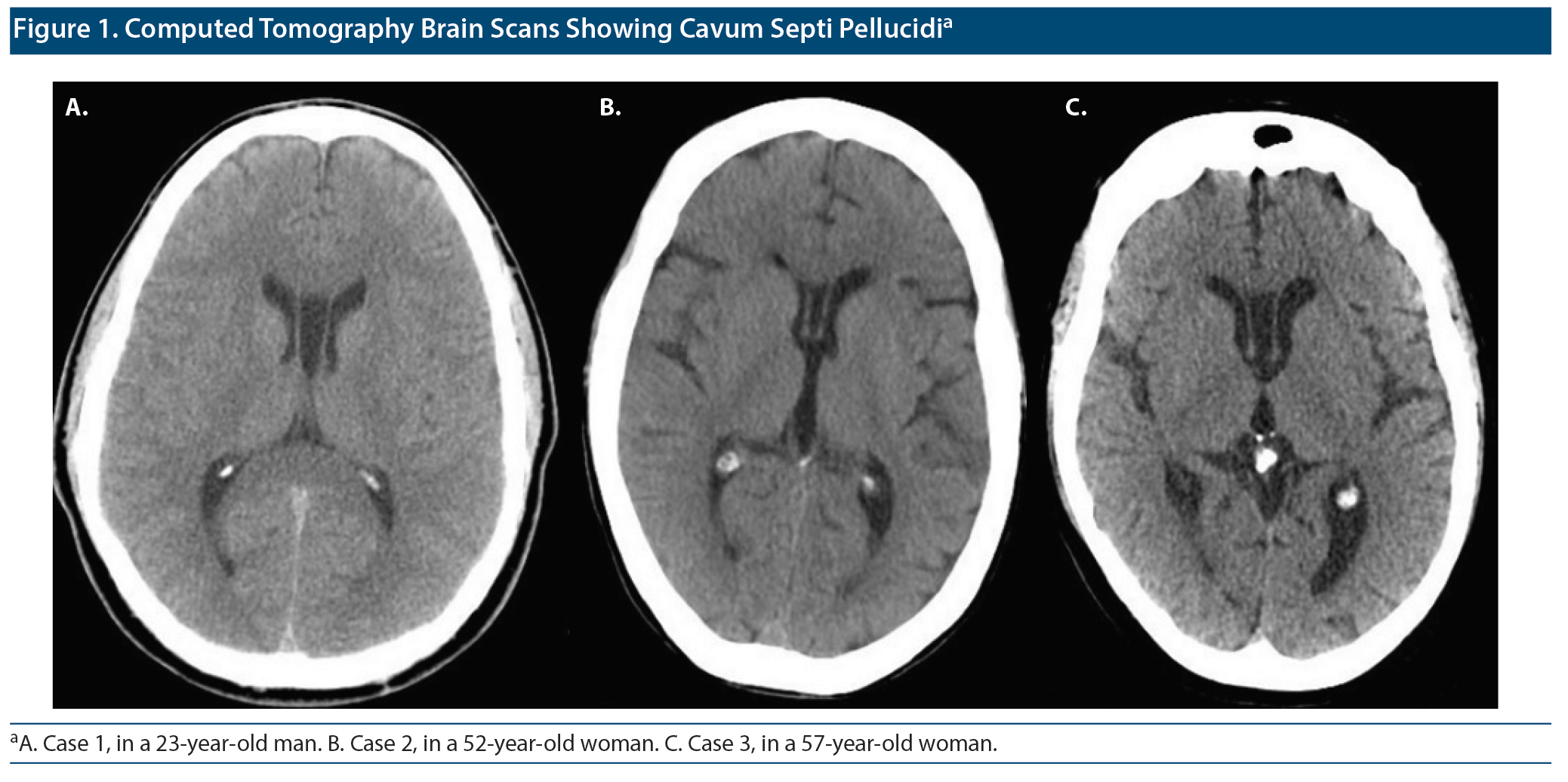
The prevalence of cavum septi pellucidi (CSP) is significantly higher in individuals with mental illness when compared with healthy subjects, with no apparent difference between patients with schizophrenia spectrum versus mood disorders.1 This report presents the cases of 3 patients with CSP and temporal lobe epilepsy (TLE)-related psychosis previously misdiagnosed as schizoaffective disorder.
Case Report 1
A 23-year-old man was seen in an outpatient appointment for mood swings, obsessive bathmophobia, auditory hallucinations, persecutory and thought insertion delusions, and Truman syndrome. He had one psychiatric admission and follow-up since age 18 years, with diagnoses of attention-deficit/hyperactivity disorder (ICD-9, 314.01), bipolar disorder (ICD-9, 296.7), and schizophrenia (ICD-9, 295.9) at different times by various physicians. We found information compatible with episodes of both nonaffective and affective psychotic episodes, suggesting a diagnosis of schizoaffective disorder (ICD-9, 295.7). His mother suffered from recurrent depression after his father, who had bipolar disorder and/or epilepsy, died by suicide by drug ingestion. The patient had been on treatment with different psychostimulants, antidepressants, and antipsychotics besides lithium carbonate, but never achieved full remission of symptoms. Blood work and urinalysis showed no significant changes. Brain computed tomography (CT) bscan disclosed CSP (Figure 1A). Electroencephalography (EEG) showed left frontotemporal slowing with sparse paroxysms. Diagnosis was changed to secondary psychotic syndrome (ICD-11, 6E61) related to temporal lobe epilepsy due to structural condition (ICD-11, 8A60), and after psychoeducation, psychopharmacologic treatment was adjusted to sodium valproate 500 mg twice daily, aripiprazole 7.5 mg twice daily, bupropion 300 mg each day, fluoxetine 40 mg each day, and olanzapine 5 mg each day. After 6 months of follow-up, the patient’s illness was in full remission, and he was free of neuropsychiatric symptoms. He finished university studies, moved to live with his girlfriend, and started working in engineering. As we were able to find paroxysms in the EEG of this patient, it was believed this case might be of postictal psychosis, so sodium valproate seemed to be a good option for the management of epilepsy and mood swings. On the other hand, although fluoxetine and bupropion contributed to the treatment of obsessive bathmophobia, aripiprazole and olanzapine surely helped in the treatment of the aforementioned psychotic symptoms.
Case Report 2
A 52-year-old woman was seen in an outpatient appointment for depressive mood and suicide ideation with craving for alcohol abuse. She had been living as homeless, having had 18 psychiatric admissions and follow-up since age 19 years, with diagnoses of borderline personality disorder (ICD-9, 301.03), alcohol abuse (ICD-9, 305.0), and drug addiction at different times by various physicians. We found information compatible with episodes of both nonaffective and affective psychotic episodes, suggesting a diagnosis of schizoaffective disorder (ICD-9, 295.7). She also was being successfully treated for rectal prolapse, atypical tuberculosis with pulmonary obstructive chronic disease, and human immunodeficiency virus and hepatitis C virus coinfection. The patient had been on treatment with different tranquilizers, antidepressants, mood stabilizers, and antipsychotics, but had never achieved full remission of symptoms. Blood work and urinalysis showed no significant changes. Brain CT scan disclosed CSP (Figure 1B). EEG showed bilateral temporal slowing. Diagnosis was changed to secondary psychotic syndrome (ICD-11, 6E61) related to temporal lobe epilepsy due to structural condition (ICD-11, 8A60), and after psychoeducation, psychopharmacologic treatment was adjusted to gabapentin 800 mg 3 times daily, clonazepam 2 mg 3 times daily, mirtazapine 60 mg each day, olanzapine 20 mg each day, and haloperidol decanoate intramuscular injectable 300 mg monthly. After 6 months of follow-up, the patient’s illness was in full remission, and she was free of neuropsychiatric symptoms. She was able to move to a housing-first project apartment while keeping psychotherapy and occupational therapy. Although we might never understand clearly if this case was of postictal or interictal psychosis, gabapentin and clonazepam were believed to be the best option to prevent both epileptic seizures and alcohol/drug abuse relapse. Depressive symptoms were treated with mirtazapine, while haloperidol and olanzapine have been crucial for the prophylaxis of new psychotic episodes.
Case Report 3
A 57-year-old woman was seen in an outpatient appointment for mood swings, obsessive thinking, compulsive rituals, thought broadcasting, auditory hallucinations, and grandiose delusions. She had 8 psychiatric admissions and follow-up since age 18 years, with diagnosis of schizophrenia (ICD-9, 295.9) and obsessive-compulsive disorder (ICD-9, 300.3) at different times by various physicians. We found information compatible with episodes of both nonaffective and affective psychotic episodes, suggesting a diagnosis of schizoaffective disorder (ICD-9, 295.7). She also was being successfully treated for obesity-related diabetes mellitus, epilepsy, and iatrogenic parkinsonism. The patient had been on treatment with different tranquilizers, antidepressants, mood stabilizers, and antipsychotics, but had never achieved full remission of symptoms. Blood work and urinalysis showed no significant changes. Brain CT scan disclosed CSP (Figure 1C). EEG showed inconstant bilateral temporal slowing. Diagnosis was changed to secondary psychotic syndrome (ICD-11, 6E61) related to temporal lobe epilepsy due to structural condition (ICD-11, 8A60), and after psychoeducation, psychopharmacologic treatment was adjusted to sodium valproate 500 mg 4 times daily, clomipramine 75 mg 3 times daily, clozapine 100 mg each day, and aripiprazole intramuscular injectable 400 mg monthly. After 6 months of follow-up, the patient’s illness was in full remission, and she was free of neuropsychiatric symptoms. Although not yet elderly, she was successfully admitted to a nursing home to ease the burden on her family, already in burnout. As there was a description of various seizures in this case, it was believed to be a case of interictal psychosis, so sodium valproate seemed to be a good option for the management of epilepsy and mood swings. Last but not least, while clomipramine contributed to the treatment of obsessive thinking, aripiprazole and clozapine surely helped in the treatment of previously resistant psychotic symptoms.
Discussion
For decades, neuroscientists and clinicians have been searching for correlations between CSP and schizophrenia spectrum disorders.2 This line of research was based on some studies’ findings that may reflect neurodevelopmental abnormalities in midline and associated limbic structures of the brain in schizophrenia spectrum disorders.3 A more recent systematic review with meta-analysis4 suggested that only a large CSP is associated with schizophrenia spectrum disorders, whereas a small CSP may be considered a normal neuroanatomical variation.
On the other hand, studies looking for correlations between CSP and epilepsy are not as common, unfortunately. Although a study5 showed no differences in CSP prevalence between mesial TLE patients and healthy controls, some authors believe there might be an important role for septal and diencephalic midline structures in cerebral electrogenesis, as more than two-thirds of patients with CSP may show epilepsy.6 Indeed, there is convincing evidence of frequent, sometimes continuous epileptic activity in limbic structures at the time of psychosis, suggesting that, in some cases at least, the epileptic activity is the cause of the psychotic symptoms.7
As part of the limbic system, septum pellucidum neurodevelopment malformations (eg, CSP) should not be underestimated as possibly involved in the complex physiopathology of TLE psychosis. Although the use of CT and EEG is limited for the study of CSP and TLE, there is some interest in developing more refined neuroimaging and neurophysiological research regarding the relation between these 2 entities, whose psychopathology may resemble, among other disorders, schizoaffective spectrum disorders.
Published online: November 12, 2020.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Permission was obtained from the patients to publish these case reports, and information was de-identified to protect anonymity.
REFERENCES
1.Wang LX, Li P, He H, et al. The prevalence of cavum septum pellucidum in mental disorders revealed by MRI: a meta-analysis. J Neuropsychiatry Clin Neurosci. 2020;32(2):175-184. PubMed CrossRef
2.Mathew RJ, Partain CL, Prakash R, et al. A study of the septum pellucidum and corpus callosum in schizophrenia with MR imaging. Acta Psychiatr Scand. 1985;72(5):414-421. PubMed CrossRef
3.Takahashi T, Suzuki M, Hagino H, et al. Prevalence of large cavum septi pellucidi and its relation to the medial temporal lobe structures in schizophrenia spectrum. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(6):1235-1241. PubMed CrossRef
4.Trzesniak C, Oliveira IR, Kempton MJ, et al. Are cavum septum pellucidum abnormalities more common in schizophrenia spectrum disorders? a systematic review and meta-analysis. Schizophr Res. 2011;125(1):1-12. PubMed CrossRef
5.Trzesniak C, Linares IM, Coimbra ÉR, et al. Adhesio interthalamica and cavum septum pellucidum in mesial temporal lobe epilepsy. Brain Imaging Behav. 2016;10(3):849-856. PubMed CrossRef
6.Varsik P, Buranová D, Kollár B, et al. The quest of cavum septi pellucidi: obscure chance event discovery or the result of some encoded disturbance? developmental cerebral dysplasias, cavum septi pellucidi and epilepsy: clinical, MRI and electrophysiological study. Neuroendocrinol Lett. 2005;26(3):219-224. PubMed
7.Elliott B, Joyce E, Shorvon S. Delusions, illusions and hallucinations in epilepsy, 2: complex phenomena and psychosis. Epilepsy Res. 2009;85(2-3):172-186. PubMed CrossRef
aClínica Universitária de Psiquiatria e Psicologia Médica, Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal
bHospital Júlio de Matos, Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal
*Corresponding author: João Gama Marques, MD, PhD, Centro Hospitalar Psiquiátrico de Lisboa, Hospital Júlio de Matos, Avenida do Brasil, 53, Lisboa, 1749-002 Portugal ([email protected]).
Prim Care Companion CNS Disord 2020;22(6):20l02613
To cite: Gama Marques J. Temporal lobe epilepsy mimicking schizoaffective disorder in patients with cavum septi pellucidi. Prim Care Companion CNS Disord. 2020;22(6):20l02613.
To share: https://doi.org/10.4088/PCC.20l02613
© Copyright 2020 Physicians Postgraduate Press, Inc.
Please sign in or purchase this PDF for $40.00.
Save
Cite