Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Limbic encephalitis may have various causes and be associated with a number of neuropsychiatric disorders. Our knowledge of viral etiology, including herpes simplex virus, is quite advanced, but in autoimmune cases, our knowledge is still limited.
Case report. A 72-year-old man was admitted to our outpatient clinic for sudden-onset amnesia and confusion that had lasted for more than 2 weeks.
Thymoma and Limbic Encephalitis: A Dangerous Liaison
To the Editor: Limbic encephalitis may have various causes and be associated with a number of neuropsychiatric disorders.1 Our knowledge of viral etiology, including herpes simplex virus, is quite advanced, but in autoimmune cases, our knowledge is still limited.2
Case report. A 72-year-old man was admitted to our outpatient clinic for sudden-onset amnesia and confusion that had lasted for more than 2 weeks. The symptoms manifested 15 days previously as a result of a psychologically stressful situation, and he was unable to find his way home. According to relatives, he had been staring at a fixed point for 2 minutes at a time and had a conversation with his deceased mother. These episodes were repeated several times during the same day. His medical history included mild heart failure and benign prostatic hyperplasia. He had been treated with indapamide, acetylsalicylic acid, and alfuzosin for hypertension and benign prostate hypertrophy.
During the neurologic examination, his personal and place orientation were found to be normal despite temporal disorientation. His speech included word perseverations. His standardized Mini-Mental State Examination (MMSE)3 score was 21/30 (2 points lost for orientation, 3 for attention and calculation, 2 for recall, and 2 for language).
Perseverations in Luria alternating motor sequences and clock drawing tests and planning errors were also present, suggesting executive dysfunction and mild cognitive impairment. Results of the examination of pyramidal, extrapyramidal, cerebellar, and sensory systems were found to be within normal limits.
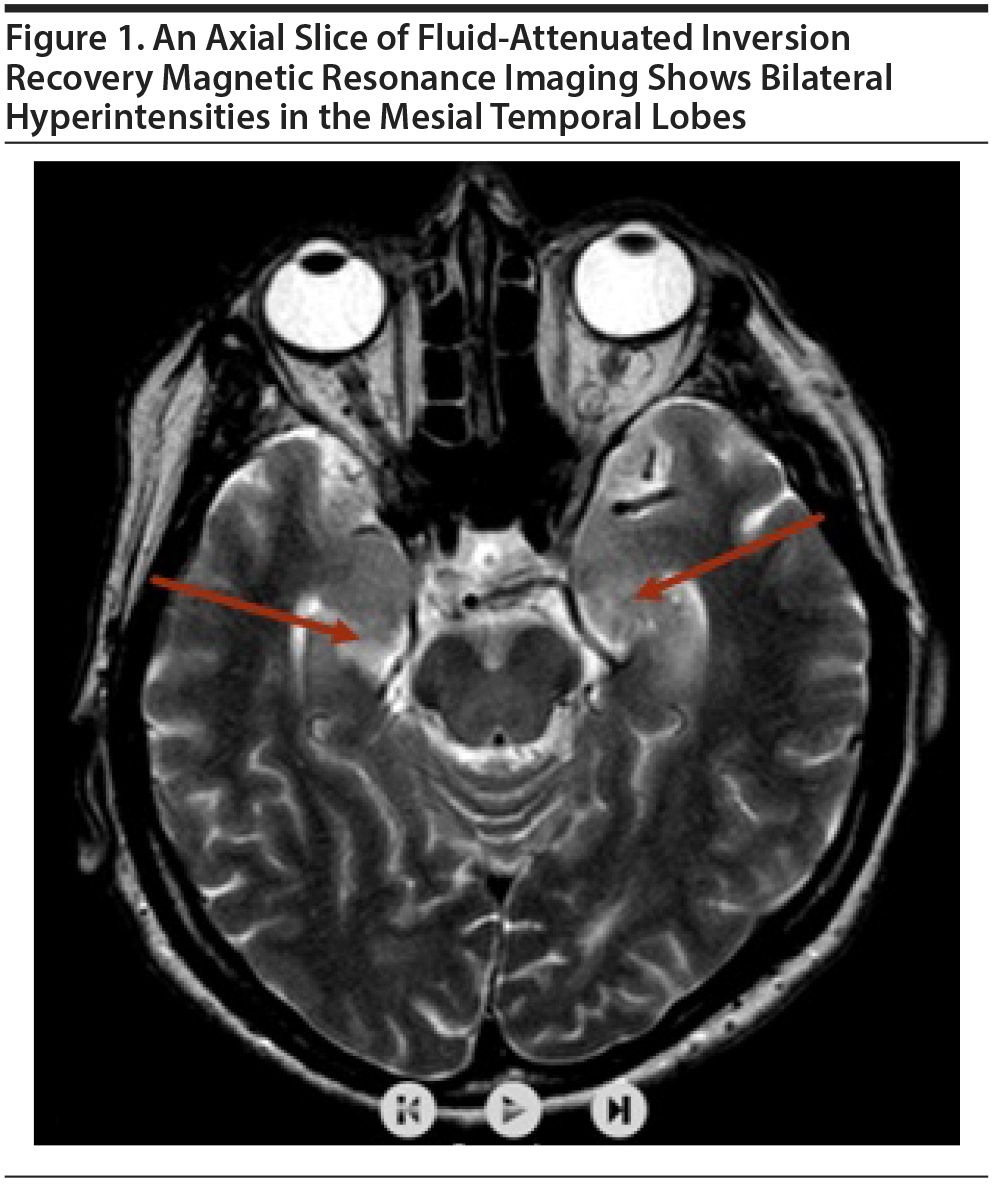
Brain magnetic resonance imaging (MRI) revealed hyperintensities in bilateral mesial temporal lobes (Figure 1). His electroencephalogram showed bitemporal neuronal hyperexcitability. No fever was present, and blood chemistry analysis including blood count was unremarkable. Cerebrospinal fluid (CSF) analysis showed protein and glucose levels within normal limits with no inflammatory cells. Herpes simplex virus 1 and 2 IgG and IgM antibodies examined by the polymerase chain reaction test were negative. The diagnosis was limbic encephalitis associated with cognitive impairment and epilepsy.
The patient was given intravenous prednisolone 1,000 mg/d for 5 days followed by oral prednisolone at a dose of 16 mg per/d. In addition, valproic acid 1,000 mg/d was started orally. The limbic encephalitis antibody panel of plasma and CSF showed leucine-rich glioma inactivated 1 (LGI1) positivity. Abdomen and thorax computed tomography (CT) scans were performed. A round mass lesion was found in the retrosternal area on the thorax CT scan. Examination results of acetylcholine receptor antibodies and muscle-specific tyrosine kinase in peripheral blood were negative. An anterior thoracotomy was performed, and the mediastinal mass was removed. The pathological examination showed type B2 thymoma (cortical thymoma).
Our final diagnosis established anti-LGI1 limbic encephalitis related to thymoma according to the 2018 ICD-10-CM diagnosis code G04.81 (other encephalitis-limbic). Oral prednisolone was discontinued because a second brain MRI showed regression in lesions 6 weeks after surgery. At the 6-month follow-up visit, the patient showed none of the previous symptoms and was given no immune treatment. His MMSE score had improved to 25/30 (2 points lost for attention and calculation, 1 for recall, and 2 for language). His score improved due to better orientation and recall. Valproic acid was prescribed to be used for at least 1 year.
LGI1 is a secreted synaptic protein that organizes α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors of glutamate.4 LGI1 antibodies are associated with thymoma in a ratio < 5% and even less with other cancers. Anti-LGI1 limbic encephalitis can cause memory dysfunction and seizures. In this disorder, the most affected brain area is the medial temporal lobe. In addition, hyponatremia is common in these cases.5
Thymomas are commonly associated with myasthenia gravis.6 However, this case highlights that thymomas may also be related to limbic encephalitis.
References
1. Foster AR, Caplan JP, Jason PC. Paraneoplastic limbic encephalitis. Psychosomatics. 2009;50(2):108-113. PubMed CrossRef
2. Lancaster E. The diagnosis and treatment of autoimmune encephalitis. J Clin Neurol. 2016;12(1):1-13. PubMed CrossRef
3. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state." A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. PubMed
4. Dalmau J, Geis C, Graus F. Autoantibodies to synaptic receptors and neuronal cell surface proteins in autoimmune diseases of the central nervous system. Physiol Rev. 2017;97(2):839-887. PubMed CrossRef
5. Vincent A, Bien CG, Irani SR, et al. Autoantibodies associated with diseases of the CNS: new developments and future challenges. Lancet Neurol. 2011;10(8):759-772. PubMed CrossRef
6. Romi F, Hong Y, Gilhus NE. Pathophysiology and immunological profile of myasthenia gravis and its subgroups. Curr Opin Immunol. 2017;49:9-13. PubMed CrossRef
aDepartment of Neurology, Maltepe University, Faculty of Medicine, Istanbul, Turkey
bClinical Psychology and Neuroscience, Department of Psychology, Maltepe University, Istanbul, Turkey
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Consent was obtained from the patient and his legal guardian to publish the case report, and information was de-identified to protect anonymity.
Published online: September 27, 2018.
Prim Care Companion CNS Disord 2018;20(5):17l02257
To cite: Ates MF, Sahin S, Cinar N, et al. Thymoma and limbic encephalitis: a dangerous liaison. Prim Care Companion CNS Disord. 2018;20(5):17l02257.
To share: https://doi.org/10.4088/PCC.17l02257
© Copyright 2018 Physicians Postgraduate Press, Inc.
Please sign in or purchase this PDF for $40.00.
Save
Cite