Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(3):23f03667
Author affiliations are listed at the end of this article.
Have you ever been uncertain about the nature and severity of the sequelae of a traumatic brain injury (TBI)? Have you been unsure about how best to evaluate your patients following a TBI? Have you been challenged to find an effective approach to your patients’ impulsivity, aggression, and disturbed sleep? Have you wondered about whether your patients will recover quickly and completely after a TBI? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr B, an active-duty Army Sergeant First Class with 15 years of military service, sustained a blast injury from an improvised explosive device (IED) while deployed in Afghanistan that resulted in a left lower extremity amputation and a mild TBI (mTBI).
Initially, he received treatment overseas before being returned to the United States for treatment at a military hospital, primarily for his lower extremity amputation. Before his discharge from the inpatient service, he was screened for his mTBI and considered to be “stable.” However, during a follow-up visit with his new primary care physician (PCP), Mr B reported a bevy of symptoms, including sleeping only 3 hours per night because of “nightmares” as well as pain, poor memory, impaired concentration, and severe irritability. Although he denied the use of illegal substances, on occasion he would drink up to 2 bottles of wine per night for his pain and to help him sleep. He also had issues with his residual limb due to a poorly fitting prosthetic device from limb shrinkage, as well as superficial, but painful, skin lesions on the bony prominences of his amputation site.
Prior to the IED blast, Mr B was independent in all aspects of his life, working full time in a physically demanding job with no restrictions placed on his physical function. He had no history of hospitalizations, surgeries, or medical conditions other than chronic back pain that had been ameliorated by weight loss and a brief course of physical therapy. He did not take any medications, but he drank “socially” (2 drinks once or twice per week) and used smokeless tobacco (which he quit while he was an inpatient).
Mr B was right-handed, reported no developmental delays, had completed some college courses, and had advanced military training. He was married with 4 children but did not do much childrearing following his injuries. He was raised in a small town with 2 married parents and 3 siblings; he reported that his childhood was “okay.” He did not have much familial support, as his military station was far from his home and his mother was deceased. There was no family history of neurological or psychiatric conditions.
Following the IED blast, Mr B was started on numerous medications: both short-acting and long-acting oxycodone (substituted for hydromorphone while an inpatient), indomethacin (to prevent the development of heterotopic ossification of his left residual limb), proton pump inhibitors (for prophylaxis of upper gastrointestinal bleeding and stress ulcer prophylaxis), propranolol and topiramate (for irritability), and a small dose of quetiapine (for sleep).
Prior to the IED blast, Mr B had sustained several head injuries from vehicle rollovers and other blast exposures; each went without treatment (“I needed to just keep going”). Other military incidents included exposures to dead bodies. Although he refused to answer questions about thoughts of suicide, he admitted to having morbid thoughts and thoughts of not waking up.
Mr B doubted that these problems could be helped by a medical provider, and he only presented for care to pacify his wife (they were close to divorcing) and because he was ordered to be evaluated by his command. His PCP, although an experienced provider, was unsure about how to address Mr B’s multiple concerns, as he did not know which ones were related to the TBI.
DISCUSSION
What Are TBIs, and What Causes Them?
The Centers for Disease Control and Prevention (CDC) defines TBI as “a disruption in the normal function of the brain that can be caused by a bump, blow, or jolt to the head or a penetrating head injury.”1 Observing any of the following clinical signs constitutes a disruption: a period of loss or a decreased level of consciousness; a loss of memory for events immediately before (retrograde amnesia) or after the injury (posttraumatic 2 amnesia); neurological deficits (eg, muscle weakness, loss of balance or coordination, disruption of vision, a change in speech and language, or sensory loss); or any alteration in mental state at the time of the injury (such as confusion, disorientation, slowed thinking, or difficulty with concentration).2
TBIs tend to occur in 6 ways: the head being struck by an object, the head striking an object, acceleration/ deceleration of the brain without direct external impact, a foreign body that penetrates the brain, force from a blast or explosion, and “other forces yet to be defined,” which covers diagnoses such as anomalous health incidents.3
Another definition that can help to characterize TBI comes from The Demographics and Clinical Assessment Working Group of the International and Interagency Initiative Toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health; it states that “a traumatic brain injury is an alteration in brain function, or other evidence of brain pathology, which is caused by an outside force.”2 It is noteworthy that this definition focuses specifically on the brain and not the head, as people can have a head injury that does not cause a brain injury; conversely, they can have a brain injury and not show external evidence of a head injury. In addition, evidence of brain pathology (eg, as seen on a magnetic resonance imaging [MRI] scan) could be evidence of a TBI despite a lack of symptoms, just as an individual may have symptoms of a TBI without confirmation by neuroimaging or other laboratory findings.
The annual incidence of TBI is estimated to be between 27 million and 69 million.4,5 In order of frequency, the most common causes of hospital admissions due to TBI are falls, motor vehicle collisions, and assaults. The most common causes of deaths due to TBI are motor vehicle collisions, followed by suicides and falls.6
Particularly in children and young adults, TBIs are often related to injuries sustained while playing sports and engaging in other recreational activities. However, there is a paucity of data regarding these TBIs since many of these injuries go unreported or untreated. One systematic review found that up to 30% of all TBIs were sports related.7
The pathophysiology of TBIs is divided between primary and secondary brain injuries.8 Primary injury is the injury that occurs at the time of the trauma, when the extracranial forces are applied to intracranial contents; these include focal contusions, hematomas, and shearing injuries (including diffuse axonal injuries [DAIs]). Secondary brain injuries occur after the trauma, in which a cascade of molecular injuries develops over hours or days as a sequela of the trauma (including inflammatory responses, neurotransmitter-mediated excitotoxicity that causes glutamate free-radical injury to cell membranes, mitochondrial dysfunction, and secondary ischemia from vasospasm and focal microvascular occlusions).
How Common Are TBIs?
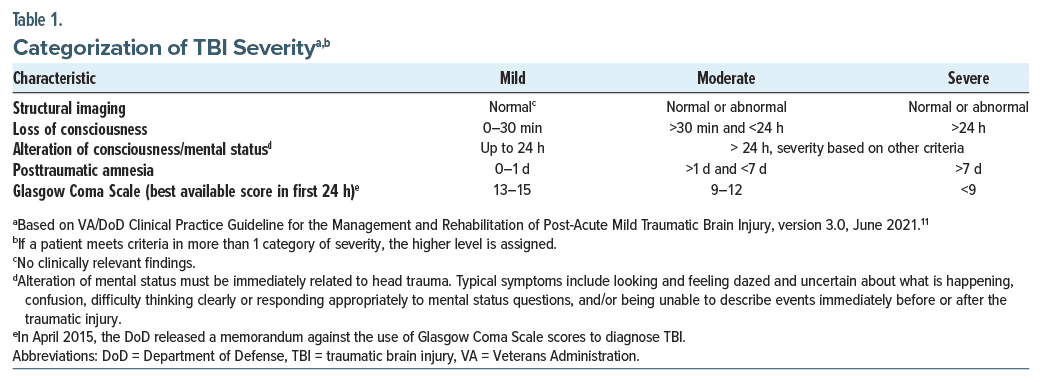
Determining the incidence and prevalence rates of TBIs is challenging, as universal criteria and definitions are lacking. They can induce confusion, disorientation, or impairments of consciousness and memory around the time of or following the injury, lasting less than 30 minutes.9 Current classification schemas typically categorize TBI severity as mild, moderate, or severe based on the Glasgow Coma Scale (GCS) score.10 Most TBIs are mild (ie, mTBI) (with a GCS score of 13–15), while those with a moderately severe TBI have a GCS score of 9–12, and those with a severe TBI have a score of 3–8 on the GCS (Table 1).11 Unfortunately, the GCS has several limitations: its interpretation can be complicated by the patient’s intoxication with alcohol or other substances; it requires a clinical examination; and when loss of consciousness has not been witnessed, the diagnosis becomes more subjective.
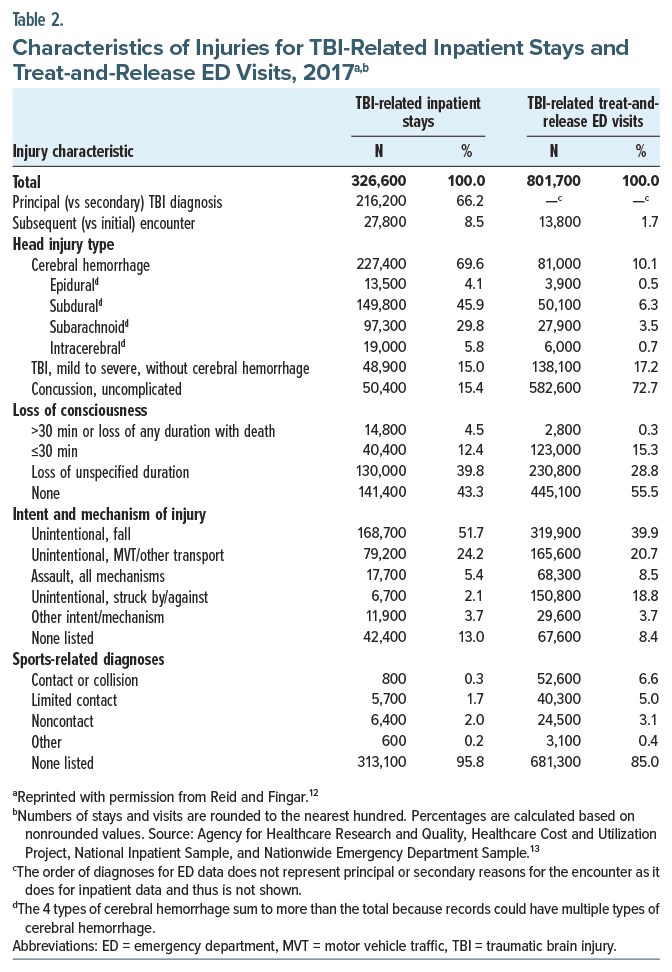
In 2017, the Agency for Healthcare Research and Quality (AHRQ)12 found that there were more than 1 million TBI-related inpatient stays and treat-and release emergency department (ED) visits (Table 2). Most of these encounters for diagnosis and treatment (71%) involved ED visits, accounting for a rate of 247 per 100,000 population, while the remaining 29% were for inpatient stays, having a rate of 100 per 100,000 population.
Although there were ∼227,000 TBI-related hospitalizations in 2016, the number of admissions decreased to almost 224,000 in 2017 and to 223,050 in 2018.12,14,15 Rates have varied by age, gender, and the principal mechanism of injury. Unintentional falls and motor vehicle crashes were the most common mechanisms of injury that contributed to a TBI-related hospitalization. The oldest age group (≥75 years) accounted for the greatest number of TBI-related hospitalizations and deaths in the CDC surveillance report, with similar data found in the AHRQ report.12,14,15
Within the Department of Defense (DoD) and the Veterans Administration (VA)16 since the year 2000, more than 473,000 service members have sustained what is now considered as the signature wound of current wars, with most of those sustaining an mTBI (82.3%). Unlike civilian TBIs, military TBIs are more commonly associated with blast injuries.17
What Are the Most Common Manifestations of TBIs?
While most people who have sustained an mTBI recover fully, a minority endorse ongoing psychiatric and neurological complaints after their injury. Persistent (ie, lasting beyond 90 days), nonspecific, postconcussive symptoms following a TBI include headaches, nausea, dizziness, vertigo, fatigue, irritability, and impaired concentration.3,11,17 Unfortunately, no pharmaceutical agents have been approved by the US Food and Drug Administration (FDA) for the treatment of postconcussive neurological or psychiatric symptoms. Nevertheless, the DoD recommends using published practice guidelines for the management of major depressive disorder (MDD), posttraumatic stress disorder (PTSD), and alcohol and substance use disorders (SUDs), as well as agitation or aggression.18 The relationship between mTBI and these comorbid psychiatric conditions remains both controversial and complex. Neuropsychiatric sequelae of TBI may be directly attributable to the concussive event or to co occurring (or preexisting) conditions (eg, PTSD, depression, anxiety, insomnia, pain, or alcohol and SUDs).17,18 Patients with comorbid psychiatric diagnoses may present with more severe symptomatology even when their brain injury is less severe. The DoD Clinical Practice Guideline for the management of mTBI recommends against conducting comprehensive neuropsychological/cognitive testing within the first 30 days following mTBI.11,18 Symptoms after the TBI vary based on brain injury location, severity, and other sequelae that are associated with moderate or severe TBI (eg, hypoxia/anoxia, intensive care unit treatment, cerebral hemorrhage, and skull fracture). Symptoms that serve as a harbinger of more serious conditions include an altered or decreased level of consciousness, disorientation, seizures, or a worsening neurological examination.
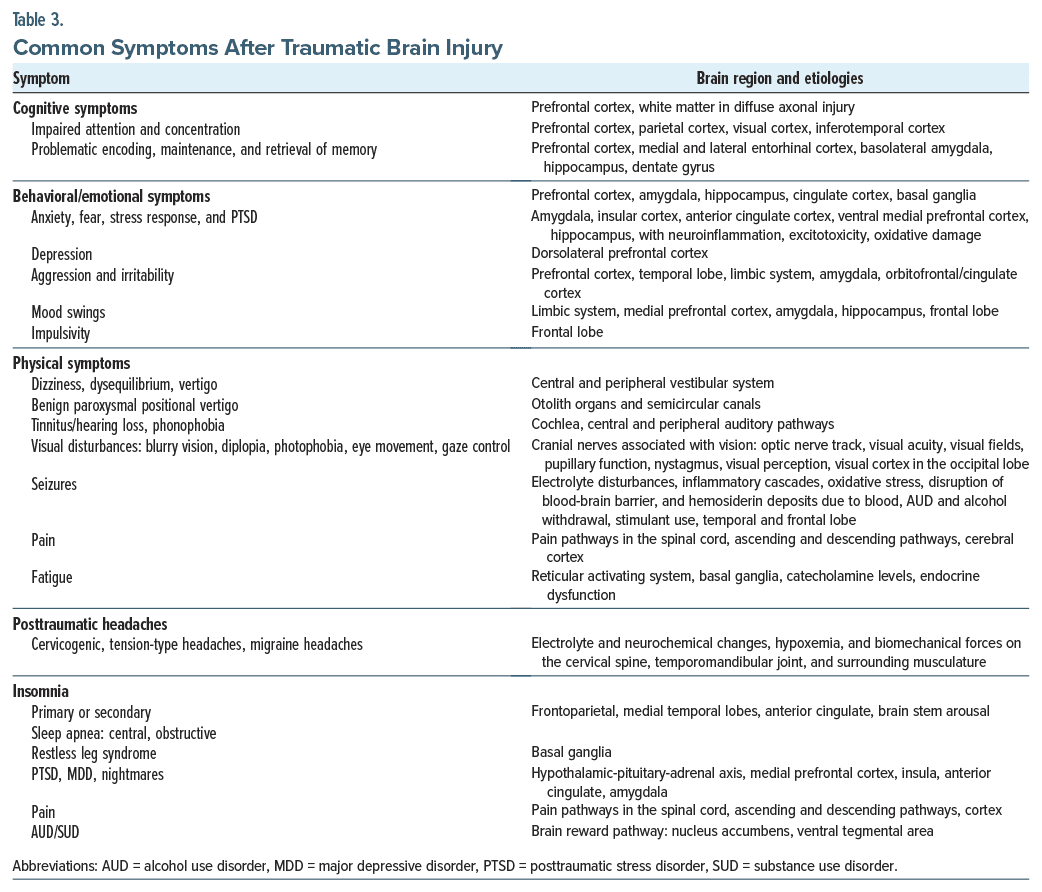
Symptoms encountered commonly after a TBI are often categorized by their affective, behavioral, cognitive, and physical manifestations (Table 3).3,11,18,19 Kenzie and colleagues20 presented a Causal Loop Diagram that integrated research from several fields showing the interrelatedness of the dynamics of concussion from impact, through affected networks and neurotransmission; these mechanisms may account for impairments in sleep, fatigue, sensorimotor function, cognition, stress, and mood.17,20 Complaints related to impaired cognition and attention are common shortly after the mTBI.13,17,18,20,21 Cognitive symptoms include problems with attention and concentration, memory, and processing speed, as well as speech, language, and executive function.19,21 The brain regions involved in impaired cognition, attention, and concentration include the prefrontal cortex, the inferotemporal cortex, the white matter (in DAI), and the parietal cortex, as well as the visual cortex.21,22 Problems with encoding, maintaining, and retrieving memories involve the prefrontal cortex, the medial and lateral entorhinal cortex, the basolateral amygdala, the hippocampi, and the dentate gyrus.21,22
Neurobehavioral symptoms after a TBI are common and include anxiety, fear, stress response, PTSD, depression, aggression, irritability, mood swings, and impulsivity.3,13,17,18,22,23 Brain regions involved in anxiety and fear include the amygdala, hippocampus, and prefrontal cortex. Pathophysiological etiologies that contribute to the development of anxiety, fear, and stress response to a TBI include neuroinflammation, excitotoxicity, and oxidative damage.13,22,23 These disturbances can be seen in both PTSD and TBI, and they share common overlapping pathophysiological processes.13,22,23 In addition, changes in the neuroendocrine system involve hypothalamic-pituitary adrenal axis dysregulation in PTSD.13,22,23
PTSD requires exposure to a trauma or stressor with death or threatened death, actual or threatened serious injury, or an actual or threatened sexual violence through direct exposure, witnessing the trauma, or learning that a relative or close friend was exposed to trauma or through indirect exposure as in first responders or medics. The traumatic event leads to reexperiencing symptoms with intrusive memories, nightmares, flashbacks, and emotional or physical responses to reminders of the trauma, with avoidance, impaired cognition and mood, and hyperarousal. PTSD is associated with comorbid psychiatric disorders in more than 80% of patients, most commonly with alcohol use or a SUD, depression, and anxiety, and these conditions are present in 13%–27% of people following a TBI.23 PTSD and TBI have considerable overlap in their symptomatology (eg, disturbed sleep, irritability, difficulty concentrating, slowed thinking, and impaired memory) that can complicate making an accurate diagnosis.17,22,23 There is growing evidence that PTSD can occur after a TBI, even with a severe TBI, when there is little to no recall of the brain injury event.23
First-line treatment of PTSD includes use of evidence-based manualized psychotherapies, such as prolonged exposure, cognitive processing therapy, and eye movement desensitization and reprocessing therapy.24 FDA-approved medications for PTSD include paroxetine and sertraline, while the VA/DoD Clinical Practice Guideline for PTSD updated in 2023 documents a strong recommendation for paroxetine, sertraline, or venlafaxine.24 Fluoxetine has been downgraded (to neither for nor against) in the VA/DoD PTSD guideline.24
Depression. Depression is commonly seen in patients with persistent postconcussive symptoms, with an estimated prevalence of 17%–61%.3,17,18,25 Comorbid depression correlates with higher rates of postconcussive sequelae and poorer outcomes. While some patients present with signs and symptoms consistent with MDD, depression in people after a TBI may be phenomenologically and neurobiologically distinct.26 Although some individuals present with amotivation, anhedonia, poor appetite, and insomnia, others have apathy, lethargy, hypersomnia, an increased appetite, and leaden paralysis.26 Depression in those with TBI may also present with significant anxiety, aggressive behavior, fatigue, distractibility, anger, or irritability.25,26
Predictors of depression after TBI include female gender, risk-taking behavior, alcohol use disorder (AUD), preinjury depression, postinjury unemployment, and a lower brain volume.25,27 The brain region most associated with depression is the dorsolateral prefrontal cortex. Neuroinflammation, neuroendocrine dysregulation, metabolic abnormalities, and neurotransmitter and circuitry dysfunction are each implicated as mechanisms for the development of post-TBI depression.17,26 The VA/DoD clinical practice guideline for the treatment of symptoms after TBI suggests avoiding medications that may lower the seizure threshold, such as bupropion, as well as medications that can contribute to confusion (eg, lithium, benzodiazepines, or anticholinergic agents).18 Patients with a history of TBI may also be more sensitive to medication side effects. Selective serotonin reuptake inhibitors (SSRIs) (eg, citalopram, fluoxetine, and sertraline) are considered first-line treatments for depression after TBI.26
Aggression and irritability. Additional neuropsychiatric symptoms following TBI include mood instability, emotional dysregulation, impulsivity, aggression, anger, irritability, and violence.3,14,17,20,26–30 Mood symptoms may involve the limbic system, medial prefrontal cortex, amygdala, hippocampus, and frontal lobe.28–30 Pharmacologic interventions for mood disorders after TBI often involve use of SSRIs or serotonin-norepinephrine reuptake inhibitors, as well as mood stabilizers that may help to regulate these systems.27 The neurocircuitry of aggression and violence (reviewed by Siever28) showed failure to control systems in the prefrontal cortex, an imbalance between regulatory influences of the amygdala and other limbic regions that involve catecholaminergic excess, and subcortical imbalances of the glutamate/γ-aminobutyric acid (GABA)ergic systems. A systematic review of the treatment of patients with agitation and/or aggression after TBI also recommended against using benzodiazepines and haloperidol, while it favored the administration of atypical antipsychotics, such as olanzapine, as well as amantadine, beta-blockers (eg, propranolol and pindolol), antiepileptic drugs (AEDs), or methylphenidate.31 Aggression after TBI has a prevalence estimated variably at 11%–96%, which may be associated with depression, a history of alcohol use or a SUD, orbitofrontal lesions, being an older male, and having poor premorbid functioning.31 Pathological laughter or crying (formerly known as pseudobulbar affect)32 (as reviewed by Roy and colleagues33) found a prevalence rate of 15.5%–21.4% within the first year after brain injury. Risk factors include male gender, mTBI, and motor vehicle accidents.33
Physical symptoms following a TBI. Dizziness and disequilibrium are common after TBI.18,34 Etiologies of these symptoms include white matter abnormalities and DAI, as well as central and peripheral vestibular system dysfunction.18,34 Otolith organs may be involved leading to benign paroxysmal positional vertigo. These symptoms may lead to gait instability and impaired balance that may be effectively treated with canalith repositioning and vestibular rehabilitation and occupational therapy.18,34 Additional common symptoms include hearing loss, tinnitus, and phonophobia. Visual disturbances include blurry vision, diplopia, photophobia, eye movement disorders, and problems with gaze control.18 The etiology of visual changes is often multifactorial and includes damage to the optic nerve, orbital and periorbital injury or hemorrhage, oculomotor nerve injury with axonal injury, and loss of retinal ganglion cells.35 Evaluation and treatment may involve several disciplines (eg, ophthalmology, neuro-ophthalmology, and vision rehabilitation).18 Changes in the sense of smell and taste (anosmia/hyposmia and dysgeusia/hypogeusia) following TBI may be associated with olfactory bulb dysfunction, orbitofrontal cortex, and temporal lobe pole, as well as gray matter density reduction in secondary olfactory regions including gyrus rectus, medial orbitofrontal cortex, anterior cingulate cortex, insula, and cerebellum.36
Seizures. Seizures may result from electrolyte disturbance, inflammatory cascades, oxidative stress, free radicals, and reactive oxygen species, as well as blood-brain barrier dysfunction, blood, skull fracture, and genetic biomarkers, and are more common in moderate-to-severe TBI than mTBI.37,38 Posttraumatic seizures are often classified as immediate (within 24 hours), early (1–7 days after TBI), or late (>7 days postinjury).37 Immediate and early seizures are conceptualized as being provoked from the injury itself.37 AUD, alcohol withdrawal, and substance intoxication (with cocaine or other stimulants) may increase the risk of seizures after TBI. In addition, certain psychotropics, including bupropion and antipsychotics, may lower the seizure threshold and increase the risk of seizures after a brain injury. Posttraumatic epilepsy (PTE) is characterized by recurrent seizures following TBI and may be seen in up to 50% of patients following a TBI, depending on the location and severity of the brain injury.37,38 The risk of PTE is generally associated with the temporal or frontal lobe; it is highest in the first 2 years after brain injury and is strongly correlated with TBI severity.39 Additionally, TBI is more frequently associated with psychogenic nonepileptic seizures or “dissociative seizures.”37 Current management of PTE consists of prophylactic treatment with levetiracetam or phenytoin for the first 7 days after the initial injury.37,38 Treatment of PTE and AED selection is often guided by the seizure type, whether it is focal or generalized, and considering medication side effects and tolerability. First line medications for PTE include levetiracetam and oxcarbazepine.39 Levetiracetam is more frequently used due to its ease of use and safety profile.39 Many cases of PTE are refractory to treatment with AEDs.38 AEDs are often prescribed for 3–6 months after an early posttraumatic seizure.39
Pain. Approximately 40%–50% of patients following an mTBI complain of persistent pain.17,18 The complexity of chronic pain pathways, nonopioid pharmacologic options, and interventional procedures as well as complementary and alternative therapies was recently reviewed.40 Pain management is often a priority in people following a TBI. Although many patients expect to receive an analgesic, use of nonpharmacologic therapies should be considered (eg, yoga, mindfulness, biofeedback, and acupuncture).40 Moreover, use of opioids should be avoided in those with chronic pain until other attempts at pain control have been attempted and failed. Posttraumatic headaches (PTHs) are also common; they are noted in 30%–90% of people with TBI, regardless of the TBI severity.17,18 PTHs are considered secondary headache disorders that start within 7 days after head trauma. History should be obtained for the presence of headache disorders prior to the TBI. PTHs present like migraine headaches, tension-type headaches, and cervicogenic headaches.18,41 The potential for neck trauma and cervical spine contribution to headache pathology is important to consider in the differential diagnosis.18 Migraine-like PTHs may be associated with somatic symptoms, such as nausea and vomiting, photophobia, and phonophobia, as well as cognitive and psychological symptoms.18,41 These headaches are often severe, throbbing or pulsatile, or unilateral and can last longer than 4 hours.18 Tension-like PTHs are usually mild to moderate; dull, aching, or with a band-like pressure; bilateral; and without significant nausea or malaise, as well as with significant palpable muscle tenderness and contraction in the neck muscles that is associated with decreased cervical range of motion in those with cervicogenic headaches.18
Posttraumatic fatigue. Fatigue is one of the most common symptoms following a TBI.18 Estimates of the prevalence of fatigue following an mTBI range from 20% to 75%.17,18 As a difficult-to-define syndrome, fatigue is a nonspecific symptom with a broad differential that includes PTSD, depression, pain, and other illnesses.17,18 It is important to differentiate between fatigue, apathy, excessive daytime sleepiness, sleep apnea, insomnia, and medication side effects.17 In addition, fatigue may be multifactorial with 1 or more of these impacting energy levels. The brain regions implicated in the pathophysiology of fatigue include the reticular activating system and the basal ganglia.17 Changes in catecholamine levels and pituitary function lead to abnormal levels of thyroid and growth hormone and decreased cortisol levels that may contribute to post-TBI fatigue.17
Insomnia. Sleep disturbances are common following TBI, and they develop in approximately one-third of patients following an mTBI.18 Patients may present with a persistent difficulty falling or staying asleep, a delayed sleep phase syndrome, and an irregular sleep-wake pattern.18 It is important to evaluate common causes of secondary sleep disorders, including central or obstructive sleep apnea, restless leg syndrome, and psychiatric disorders (such as MDD or PTSD, pain, and alcohol or substance use). Sleep is regulated by numerous molecular mechanisms for circadian rhythm and sleep regulation that involve wake promoting and sleep-suppressing endogenous molecules (such as catecholamines, orexin, histamine, GABA, adenosine, serotonin, melatonin, and prostaglandin D2).42 The brain regions involved are the frontoparietal, medial temporal lobes, anterior cingulate precuneus, and brain stem arousal networks.42 Pharmacologic treatment of sleep disturbance following an mTBI is complex. For all pharmacologic interventions, providers should assess the risk-benefit profiles, including side effects and misuse potential. Patients with a history of a TBI may be more sensitive to the cognitive side effects of sedatives/ hypnotics.
How Can Neuroimaging and Neuropsychiatric Testing Refine the Diagnosis and Guide Treatment of TBIs?
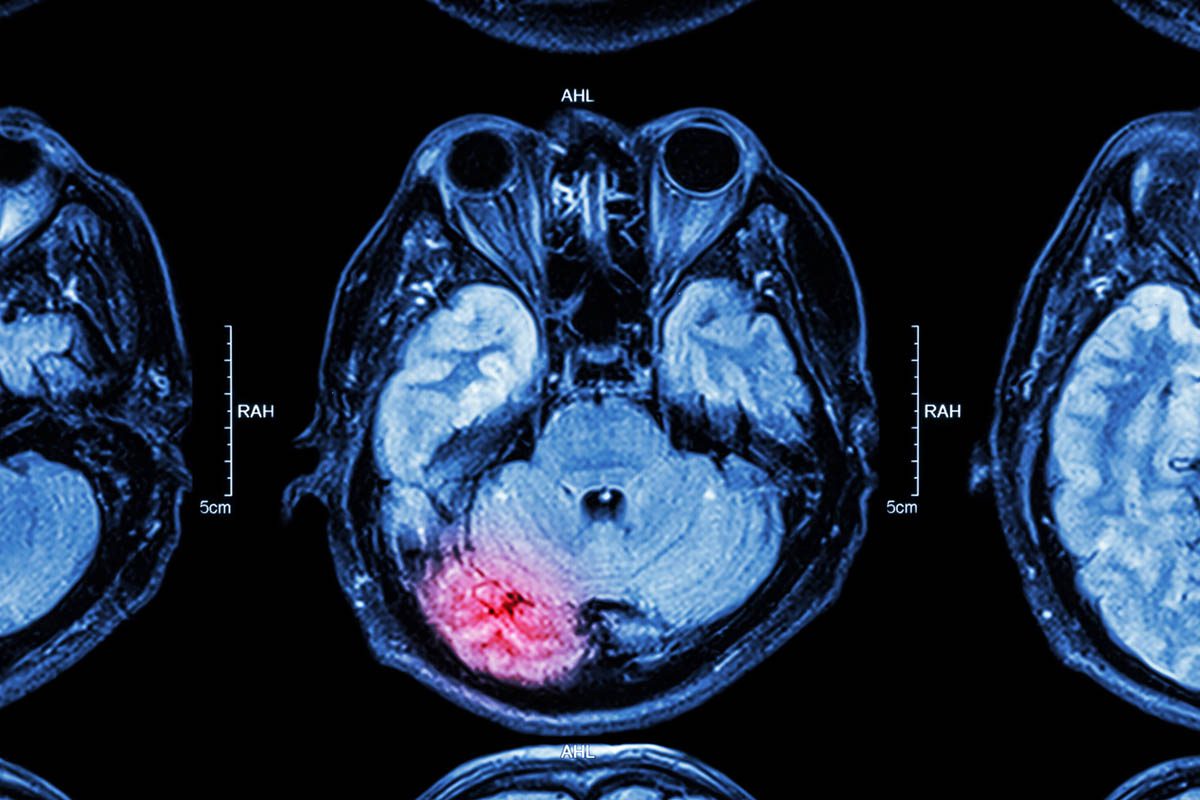
Neuroimaging plays a crucial role in the assessment and management of TBIs. Various imaging techniques, such as computed tomography (CT), MRI, functional MRI (fMRI), diffusion tensor imaging (DTI), and positron emission tomography (PET), provide valuable information about the structural and functional changes that occur in the brain following TBI.43
CT is often the initial imaging modality used in the acute setting of a TBI due to its wide availability and ability to detect acute intracranial hemorrhages and skull fractures quickly.43 It is particularly useful in identifying life-threatening injuries that require an immediate intervention. CT findings, such as brain contusions and hemorrhagic axonal injury, have been shown to be independent predictors of poor outcomes following a TBI.44 However, CT has limited sensitivity to detect subtle brain injuries, and it does not provide detailed information about the underlying pathophysiology of TBI.
MRI is a more sensitive imaging modality that can detect a wider range of brain abnormalities associated with TBI, including contusions, microhemorrhages, DAI, and edema.43 MRI can also provide detailed anatomical information, and it is particularly useful in detecting DAI, which is a common and often underdiagnosed injury in patients who have sustained a TBI.44 Diffusion-weighted imaging and DTI (which measure the diffusion of water molecules in brain tissue) can reveal microstructural changes in white matter tracts, and these methods have been shown to correlate with clinical outcomes following TBIs.44,45 In addition, fMRI can assess brain activation patterns and connectivity, providing insights into the functional consequences of TBI.43
PET imaging, including fluorodeoxyglucose (FDG)- PET and ligand-based PET (tau and translocator protein [TSPO]), can provide information about brain metabolism, neuroinflammation, and the distribution of abnormal proteins associated with TBI.46–50 FDG-PET has been shown to improve outcome prediction in patients following an mTBI and can help identify brain regions with altered glucose metabolism.44 Ligand-based PET imaging that targets tau and TSPO can provide insights into the pathophysiological processes that underlie TBI, such as neurodegeneration and neuroinflammation.46,48–50
Neuroimaging plays a crucial role in the evaluation and management of concussion and postconcussion syndrome (PCS).51 Various imaging techniques provide valuable insights into the structural and functional changes that occur in the brain following a concussion.51–53 MRI is commonly used in the assessment of concussion and PCS. It can detect structural abnormalities (such as contusions, hemorrhages, and DAI), which are often associated with concussion.52,54,55 MRI findings can also help guide clinical decision-making and provide prognostic information.54 Advanced MRI techniques, such as DTI, can assess microstructural changes in white matter tracts and provide insights into the integrity of neural pathways affected by concussion.52 Functional neuroimaging techniques, such as fMRI, can assess brain activation patterns and connectivity, providing information about the functional consequences of concussion, including changes in default-mode networks and activation during specific cognitive tasks.55 These techniques have been used to study the effects of concussion on cognitive processes, such as working memory, and to evaluate the recovery of brain function over time.56,57 FDG-PET can provide information about brain metabolism and help identify regions of altered glucose metabolism associated with concussion and PCS.53 Neuroimaging findings in concussion and PCS can vary depending on the severity of the injury and the individual characteristics of the patient; some studies have shown that neuroimaging findings may be normal in individuals following a concussion, especially in cases of mild injury.54 However, advanced neuroimaging techniques have revealed subtle abnormalities in brain structure and function that may not be apparent on conventional imaging.52 In addition to aiding in the diagnosis and evaluation of concussion and PCS, neuroimaging can also help guide treatment decisions. For example, neuroimaging findings can help identify individuals at higher risk for prolonged recovery and guide the implementation of targeted interventions.58 Neuroimaging can also be used to monitor the effects of treatment and track the recovery process.56
Neuroimaging has been valuable in the clinical assessment of TBI and in guiding psychiatric assessment and treatment. Since TBI is associated with an increased risk of psychiatric disorders (including depression, anxiety, PTSD, and cognitive impairment), neuroimaging techniques can help elucidate the neural correlates of these psychiatric symptoms and provide objective measures of brain abnormalities associated with TBI related psychiatric disorders.59–61 For example, neuroimaging studies have shown structural and functional abnormalities in the prefrontal cortex, amygdala, hippocampus, and other brain regions in individuals with TBI-related psychiatric disorders.45,59,62 These findings can inform the development of targeted interventions and personalized treatment approaches for patients with psychiatric comorbidities following a TBI.
CT and MRI are commonly used imaging modalities that provide valuable information about the structural abnormalities associated with TBI. However, advanced techniques, such as fMRI, DTI, and PET imaging, provide insights into the functional and metabolic changes in the brain following TBI, as well as in concussion and PCS. Furthermore, neuroimaging has contributed to our understanding of the neural correlates of TBI-related psychiatric disorders, guiding psychiatric assessment and treatment in this population.
What Types of Cognitive Testing Can Be Conducted Following a TBI?
Cognitive assessment (including cognitive screening, neuropsychological testing, and computer-based testing) plays a crucial role in the evaluation (eg, of the extent and nature of cognitive deficits), prediction of outcomes, and management (eg, guiding rehabilitation interventions) of TBI.
Cognitive screening tests (such as the Montreal Cognitive Assessment63 and Mini-Mental State Examination64) provide a quick assessment of cognitive functioning in individuals who have sustained a TBI. However, these tests offer limited information about certain cognitive domains, and they may not detect subtle deficits.65 On the other hand, detailed neuropsychological evaluations can provide comprehensive data on a variety of cognitive domains (such as visuospatial function, memory, attention, executive function, language, and praxis) as well as neuropsychiatric and behavioral features.65 Neuropsychological testing is considered the “gold standard” test for the assessment of cognitive deficits associated with TBI.66 Such testing helps to identify specific cognitive impairments, the severity of deficits, and how these deficits change over time.67 Neuropsychological testing has also been used extensively in research studies to investigate the cognitive sequelae of TBI.68
Several studies have demonstrated the predictive value of neuropsychological testing in TBI. For instance, Carroll and colleagues69 found that children who sustained an mTBI had a good prognosis, with quick resolution of symptoms, and little evidence of residual cognitive deficits. However, Nordström and associates70 showed that individuals with an mTBI had lower overall cognitive function compared to those without a TBI during a follow-up period. Nordström and associates70 also found lower scores on separate tests of cognitive function, suggesting that neuropsychological testing can help to identify cognitive impairments even in those with an mTBI.
Longitudinal considerations are essential in the assessment of cognitive function following a TBI. TBI can result in both acute and chronic cognitive deficits. DTI has been used to assess microstructural white matter injuries associated with TBI,71 and Sidaros and coworkers44 demonstrated a correlation between DTI findings and clinical outcomes after a severe TBI. Sidaros and coworkers’ study44 found that the extent of white matter injury on DTI correlated with long-term cognitive impairment. Moreover, Wright and colleagues72 showed that acute metabolic crisis-related brain atrophy was associated with worse cognitive abilities at 12 months postinjury, highlighting the importance of longitudinal assessments in understanding the trajectory of cognitive recovery and identifying individuals at risk for long-term cognitive deficits.
Computer-based testing has emerged as a promising tool for cognitive assessment following TBI. Such testing offers standardized and objective measures of cognitive function and allows for efficient administration and scoring.73 Fetta and associates’ critical review73 evaluated the impact of computer-based cognitive rehabilitation interventions on cognitive outcomes in populations with acquired brain injuries and provided insights into the potential benefits of computer-based testing in TBI. Their review highlighted the limited number of studies specifically focused on mTBI and emphasized the need for more research in this area.73
Long-term outcomes following TBI are influenced by the robust interplay between cognitive and psychiatric factors. Studies have shown that individuals with TBI and comorbid psychiatric symptoms have worse cognitive outcomes compared to those without psychiatric symptoms.68 For example, the presence of psychiatric symptoms can impact functional outcomes and the quality of life in individuals who have sustained a TBI.74 Neuropsychological assessments can also assist in differentiating between cognitive deficits that are directly related to TBI and those that may be associated with preexisting psychiatric conditions. This differentiation is crucial for accurate diagnosis and appropriate treatment planning. For example, individuals with a TBI may experience cognitive impairments that are distinct from those associated with psychiatric disorders, such as PTSD or depression.75 Neuropsychological assessment can also help to identify the specific cognitive profile associated with TBI, which can guide treatment decisions and interventions.
Neuropsychological evaluation can also provide insights into emotional and behavioral functioning that may be related to TBI (eg, irritability, impulsivity, and emotional dysregulation)76 and which can have a significant impact on psychiatric assessment and treatment planning. Furthermore, neuropsychological assessment can assist in identifying individuals who may benefit from specific psychiatric interventions. For instance, individuals with TBI who have cognitive deficits that impact their ability to engage in therapy may require modifications to treatment approaches (such as providing additional support or utilizing compensatory strategies).77 By identifying cognitive strengths and weaknesses, neuropsychological assessment can guide the selection of appropriate therapeutic interventions and help optimize treatment outcomes.
What Resources Are Available for Patients Following a TBI?
Unfortunately, there is a paucity of data about TBI related disability; however, some generalities have been noted. Most patients who experience an mTBI recover without sequelae,78 although a significant minority have problems that last for months or even years. Most individuals who suffer following a moderate or severe TBI improve significantly over time, even after several years.
Multiple resources are available to patients with complications (including disability) of a TBI. Most are treated by their PCPs. Specialists in physical medicine and rehabilitation and psychiatrists can also be helpful, particularly when there is impaired function and/or symptoms of affective, behavioral, or cognitive dysfunction.
Physical therapists are the most utilized rehabilitation therapists, as many patients with even an mTBI have complaints of dizziness and loss of balance. Back to work or school recommendations can be fine-tuned following assessments (such as the Buffalo Concussion Treadmill Test, which establishes the heart rate at which exercise induced exertion exacerbates post-TBI symptoms).79 Occupational therapists can assist with activities of daily living, including concerns of sensory overload, disorganization, and dysregulated sleep hygiene/insomnia.80 Speech and language therapists can assist those patients who have issues with articulation or word production, and they can help with strategies to optimize memory and recall.81
Although neuropsychological testing is rarely needed in cases of mTBI, it is recommended for those who have had a prolonged recovery or when there is a question about the etiology of the symptoms. Neuropsychologists can also recommend cognitive rehabilitation when testing reveals specific deficits.82
Creative art therapies include art therapy,83 music therapy,84 and dance/movement therapy.85 These are often initiated in conjunction with other therapies (eg, music therapy with physical therapy for gait and ambulation, or with a behavioral health provider to address mental health concerns).
Mental health providers often work closely with patients following a TBI, as issues with depression86 and anxiety are often reported, among other mental health concerns, either due to the brain injury or the mechanism by which it was acquired (eg, assault). Most individuals do well with a general course of treatment. However, mental health counseling may require modifications when there are cognitive issues, and medication management must be carefully tailored if the patient has post-TBI sensitivities to medications. Other treatments include nutritionist counseling (to optimize diet and nutrient intake that facilitates optimal recovery), acupuncture (often used for chronic pain to minimize the use of medications), yoga, meditation, and mindfulness.87
An invaluable piece of multimodal TBI treatment is the use of psychoeducation for the patient and their family members, friends, and even, when appropriate and with the patient’s consent, the patient’s employer. Psychoeducation often begins with the PCP and then continues during consultations from other physicians, rehabilitation specialists, and resources in the community. Psychoeducation is invaluable because, although patients with TBI often look “normal,” they may develop changes in their personality and/or cognitive function that could be difficult for families and other supportive individuals to understand. One systematic review of TBI treatment found that psychoeducation was the most effective treatment to avoid posttraumatic symptoms.88
Support groups can provide psychoeducation as well as peer support for patients, spouses, and other family members, who often feel (despite the high prevalence of TBI) they are the only ones dealing with post-TBI concerns and questions. Examples include The Brain Injury Association for America and the Traumatic Brain Injury Center of Excellence for military members and veterans. Many state, county, and local resources can also help with reintegration into communities.
What Is the Usual Course and Prognosis Following a TBI?
The consequences of TBI vary depending on the severity of the injury, as well as on preinjury and postinjury factors.89–90 One study of moderately severe TBI (n = 79 contacted; n = 51 participated)89 involved interviews of patients 17–42 months post-TBI and found that although three-fourths of them worked full-time, most struggled with cognitive and functional limitations. Another study of moderate-to-severe TBI involved interviewing patients up to 10 years postinjury (n = 141)90 and found that 70% had returned to driving; however, 60% reported difficulties in cognition, communication, behavior, and emotional functions; 40% required more support than before their injury; and 30% reported difficulties in personal relationships. Overall, the study found that problems experienced by patients 2 years postinjury persisted until 10 years postinjury.90 Those at greater risk for experiencing long-term health problems or death included racial and ethnic minorities, service members and veterans, people who experienced homelessness, people who resided in correctional and detention facilities, survivors of intimate partner violence, and people who lived in rural areas.91
PCS, a term most often for those with concussion or mTBI, is believed to peak in the first weeks or months postinjury and to subside 1–6 months postinjury. However, persistent PCS is inadequately studied. For example, 18%–31% of patients with an mTBI have persistent PCS 3–6 months postinjury, with up to 44% reporting 3 or more symptoms 1 year postinjury and 29%–54% reporting disability at 3–6 months.89,92 Furthermore, PCS has a low specificity,93 as it develops in patients with chronic pain, spinal cord injuries, orthopedic injuries, and non-TBI trauma and in those with psychological distress, as well as in healthy adults. Predicting who will manifest PCS more than 3 months postinjury is difficult because TBI severity does not predict PCS.91 PCS predictors include pain, premorbid psychiatric history, depression, preinjury neuroticism, anxiety, and anxiety sensitivity—the belief that sensations are signs of impending harmful consequences. PCS has been positively associated with emotion-focused coping but negatively associated with problem-focused coping. PCS treatment includes education, reassurance, and returning to exercise and activities.93–95 Rest may not be “the best medicine” after a concussion. Regular exercise may be protective against anxiety and depression. Graded exercise protocols under the supervision of an athletic trainer or another health care provider may also provide an in vivo method for anxiety desensitization. Physical activity is beneficial in decreasing PCS in both acute and chronic phases after concussion (as established by a meta-analysis of 23 studies).95 However, vigorous exercise within 2 weeks following an injury may result in additional symptoms. In those patients with gait imbalance or incoordination, vestibular physical therapy can be helpful. In those with cognitive symptoms (such as memory and concentration problems), cognitive rehabilitation is indicated. Other symptoms, such as headaches or nausea, may require symptomatic treatment.
How Did Mr B Fare?
Mr B was skeptical that medical treatment could help him; however, he was at least willing to talk with his PCP about his alcohol use and poor sleep. Mr B agreed that his alcohol use had “gotten out of control.” Consequently, he assented to substance use treatment and, because he needed the alcohol to sleep, a sleep evaluation.
He was prescribed naltrexone for his alcohol use. His sleep study revealed sleep apnea, for which he was prescribed a continuous positive airway pressure machine. These treatments ameliorated both his mood and his pain, and improvements in function led Mr B to believe that his PCP could help him.
With this positive therapeutic relationship, Mr B agreed to changing his (mostly ineffective) medication regimen. He was referred for acupuncture for his pain complaints (which also benefitted his sleep and mood), started on a regimen of venlafaxine (for his pain and his mood), started on gabapentin (for his neuropathic pain, phantom pain, and ameliorating insomnia), and taken off his other medications.
With continued improvement, Mr B was willing to engage in other therapies. He went to physical therapy for his gait difficulties, the prosthetic device clinic for a new fitting socket, and the wound clinic to address the skin breakdown. He started to eat more home-cooked meals (he had been eating mostly fast-food and vending machine snacks) and supplemented these with a multivitamin to assist in his wound healing. Consequentially, he also reported having more energy during the day. Prior to this, due to irritability, he had avoided returning home at night to eat with his wife and children. Now, Mr B was pleasantly surprised to find that dinner with his family each evening was noncontentious.
Although Mr B’s sleep had improved, he still had issues with sleep hygiene, including staying up late to watch television or using his smartphone excessively. He went to occupational therapy for these issues, and, while there, the occupational therapist addressed desensitization exercises for the remaining phantom limb pain. After benefitting from these treatments, Mr B was comfortable with the occupational therapist and discussed with the therapist some of his traumatic events (the therapist had been appropriately trained for these types of discussions). This made him comfortable further discussing his emotions, in general.
At this point, Mr B reported sleeping 7 hours most nights, felt well rested, and was thus taken off narcotics. He was able to initiate many of the strategies that had been prescribed, which resulted in improved functionality. However, he still had issues with his attention and memory and was referred to speech and language therapy to address these concerns. Next, Mr B was referred to a neuropsychologist. Testing showed slowed information-processing and impaired long-term memory, attention, working memory, executive function, and social cognition. These findings were consistent with both a TBI and anxiety. He followed the neuropsychologist’s recommendation to see a mental health provider for therapy, as all the previous recommendations had been very helpful to him.
He started cognitive processing therapy for his prior traumas. Simultaneously, he began art and music therapy, which both assisted with his cognitive rehabilitation and enabled him to be more open with his therapist. His wife accompanied him to marital counseling, and she became involved with a support group for spouses of patients with TBI. Empowered with psychoeducation, she became better able to handle her husband’s symptoms and stated she better understood his stressors.
After his therapeutic course, Mr B remained on active duty, no longer abused alcohol, was off the narcotic medication, became more functional at work, remained married to his wife, reported (along with his wife) high levels of marital satisfaction, and enjoyed a better relationship with his 4 children. He and his family resumed activities they had previously enjoyed together (such as camping). Mr B frequently stated to his support group and fellow soldiers that his “life had been saved” by his treatment team. He went from believing that nothing could help to being regarded as a mentor to fellow soldiers dealing with the sequelae of TBI and war trauma.
CONCLUSION
TBIs (that often occur because of falls, motor vehicle collisions, or assaults) are experienced by 27 million to 69 million each year. Fortunately, while TBIs are often categorized as mild, moderate, or severe based on the GCS score, most TBIs are mild (ie, mTBI) (with a GCS score of 13–15) and are associated with a full recovery. Nevertheless, a minority of those who have sustained a TBI endorse ongoing psychiatric and neurological complaints after their injury. Persistent (ie, lasting beyond 90 days) nonspecific postconcussive symptoms include headaches, seizures, nausea, dizziness, vertigo, fatigue, chronic pain, and irritability, as well as impaired attention and concentration. Unfortunately, no pharmaceutical agents have been approved by the FDA for the treatment of postconcussive neurological or psychiatric symptoms. Nevertheless, the DoD recommends using published practice guidelines for the management of specific symptoms and comorbid conditions (eg, MDD, PTSD, and alcohol or SUDs, as well as agitation or aggression). Various imaging techniques, such as CT, MRI, fMRI, DTI, and PET, provide valuable information about the structural and functional changes that occur in the brain following TBI, and the results of these tests can be used to guide treatment interventions. In addition to pharmacologic approaches for persistent symptoms, an invaluable piece of multimodal TBI treatment is the use of psychoeducation for the patient and their family members, friends, and even, when appropriate and with the patient’s consent, the patient’s employer.
Article Information
Published Online: May 9, 2024. https://doi.org/10.4088/PCC.23f03667
© 2024 Physicians Postgraduate Press, Inc.
Submitted: November 1, 2023; accepted December 22, 2023.
To Cite: Matta SE, LaCroix C, Walterfang M, et al. Traumatic brain injuries: manifestations, evaluation, management, and outcomes. Prim Care Companion CNS Disord. 2024;26(3):23f03667.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (Matta, Tanev, Stern); Harvard Medical School, Boston, Massachusetts (Matta, Tanev, Stern); Department of Psychiatry, Department of Physical Medicine and Rehabilitation, Uniform Services University of the Health Sciences, Bethesda, Maryland (LaCroix); The Royal Melbourne Hospital, Department of Psychiatry, University of Melbourne, Richmond, Australia (Walterfang).
Corresponding Author: Theodore A. Stern, MD, Harvard Medical School, Massachusetts General Hospital, 55 Fruit St, WRN 606, Boston, MA 02114 ([email protected]).
Author Information: Drs Matta, LaCroix, Walterfang, and Tanev are co-first authors. Dr Stern is the senior author.
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Traumatic brain injuries (TBIs) can develop when the head is struck by an object, when acceleration/deceleration of the brain occurs without direct external impact, when a foreign body penetrates the brain, when one is in proximity to a blast or explosion, and in response to other anomalous health incidents.
- Current classification schemas categorize TBI severity as mild, moderate, or severe based on the Glasgow Coma Scale (GCS) score; most TBIs are mild (with a GCS score of 13–15), while those with a moderately severe TBI have a GCS score of 9–12, and those with a severe TBI have a score of 3–8 on the GCS.
- While most people who have sustained a mild TBI recover fully, a minority endorse ongoing psychiatric and neurological complaints after their injury.
- No pharmaceutical agents have been approved by the US Food and Drug Administration for the treatment of postconcussive neurological or psychiatric symptoms; the Department of Defense recommends using published practice guidelines for the management of depression, posttraumatic stress disorder, alcohol and substance use disorders, and agitation or aggression.
- Various imaging techniques provide valuable information about the structural and functional changes that occur in the brain following TBI, and the results of these tests can be used to guide treatment interventions.
- An invaluable piece of multimodal TBI treatment is the use of psychoeducation for the patient and their family members, friends, and even, when appropriate and with the patient’s consent, the patient’s employer.
References (95)

- CDC (Centers for Disease Control and Prevention). Traumatic brain injury & concussion. 2017. [August 12, 2018]. https://www.cdc.gov/traumaticbraininjury/index.html
- Menon DK, Schwab K, Wright DW, et al. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–1640. PubMed CrossRef
- Eapen BC, Bowles AO, Sall J, et al. The management and rehabilitation of post acute mild traumatic brain injury. Brain Inj. 2022;36(5):693–702. PubMed CrossRef
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):56–87. PubMed CrossRef
- Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018;130(4):1080–1097. PubMed CrossRef
- Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res. 2012;43(4):299–307. PubMed CrossRef
- Theadom A, Mahon S, Hume P, et al. Incidence of sports-related traumatic brain injury of all severities: a systematic review. Neuroepidemiology. 2020;54(2):192–199. PubMed CrossRef
- Greve MW, Zink BJ. Pathophysiology of traumatic brain injury. Mt Sinai J Med. 2009;76(2):97–104. PubMed CrossRef
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Centers for Disease Control and Prevention; 2003.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. PubMed CrossRef
- Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Management and Rehabilitation of Post-Acute Mild Traumatic Brain Injury. Version 3.0. Department of Veterans Affairs, Department of Defense; 2021.
- Reid LD, Fingar KR. Inpatient stays and emergency department visits involving traumatic brain injury, 2017. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Statistical Brief #255. Agency for Healthcare Research and Quality (US); 2020. PMID: 32379407.
- Shin LM, Liberzon I. The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology. 2010;35(1):169–191. PubMed CrossRef
- CDC. Surveillance Report: Traumatic Brain Injury-Related Hospitalizations and Deaths by Age Group, Sex, and Mechanism of Injury–United States, 2016 and 2017. US Department of Health and Human Services, CDC; 2021.
- Peterson AB, Thomas KE. Incidence of nonfatal traumatic brain injury-related hospitalizations – United States, 2018. MMWR Morb Mortal Wkly Rep. 2021;70(48):1664–1668. PubMed CrossRef
- Department of Defense. Numbers for Traumatic Brain Injury Worldwide. Accessed July 25, 2023. https://health.mil/Military-Health-Topics/Centers-of-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers
- Schieffler DA, Matta SE. Evidence to support the use of S-adenosylmethionine for treatment of post-concussive sequelae in the military. Mil Med. 2022;187(9–10):e1182–e1192. PubMed CrossRef
- Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Concussion–Mild Traumatic Brain Injury. Version 2.0. Department of Veterans Affairs, Department of Defense; 2015.
- Paterno R, Folweiler KA, Cohen AS. Pathophysiology and treatment of memory dysfunction after traumatic brain injury. Curr Neurol Neurosci Rep. 2017;17(7):52. PubMed CrossRef
- Kenzie ES, Parks EL, Bigler ED, et al. The dynamics of concussion: mapping pathophysiology, persistence, and recovery with causal-loop diagramming. Front Neurol. 2018;9:203. PubMed CrossRef
- Stemmann H, Freiwald WA. Evidence for an attentional priority map in inferotemporal cortex. Proc Natl Acad Sci U S A. 2019;116(47):23797–23805. PubMed CrossRef
- Kaplan GB, Leite–Morris KA, Wang L, et al. Pathophysiological bases of comorbidity: traumatic brain injury and post-traumatic stress disorder. J Neurotrauma. 2018;35(2):210–225. PubMed CrossRef
- Tanev KS, Pentel KZ, Kredlow MA, et al. PTSD and TBI co-morbidity: scope, clinical presentation and treatment options. Brain Inj. 2014;28(3):261–270. PubMed CrossRef
- Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress Disorder and Acute Stress Disorder. Version 4.0. Department of Veterans Affairs, Department of Defense; 2023.
- Rapoport MJ. Depression following traumatic brain injury: epidemiology, risk factors and management. CNS Drugs. 2012;26(2):111–121. PubMed CrossRef
- Jahan AB, Tanev K. Neurobiological mechanisms of depression following traumatic brain injury. Brain Inj. 2023;37(1):24–33. PubMed CrossRef
- Cnossen MC, Scholten AC, Lingsma HF, et al. Predictors of major depression and posttraumatic stress disorder following traumatic brain injury: a systematic review and meta-analysis. J Neuropsychiatry Clin Neurosci. 2017;29(3):206–224. PubMed CrossRef
- Siever LJ. Neurobiology of aggression and violence. Am J Psychiatry. 2008;165(4):429–442. PubMed CrossRef
- Arciniegas DB, Wortzel HS. Emotional and behavioral dyscontrol after traumatic brain injury. Psychiatr Clin North Am. 2014;37(1):31–53. PubMed CrossRef
- Bryant BR, Richey LN, Jahed S, et al. Behavioral and emotional dyscontrol following traumatic brain injury: a systematic review of neuroimaging and electrophysiological correlates. J Acad Consult Liaison Psychiatry. 2022;63(6):579–598. PubMed CrossRef
- Rahmani E, Lemelle TM, Samarbafzadeh E, et al. Pharmacological treatment of agitation and/or aggression in patients with traumatic brain injury: a systematic review of reviews. J Head Trauma Rehabil. 2021;36(4):E262–E283. PubMed CrossRef
- Ahmed A, Simmons Z. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483–489. PubMed CrossRef
- Roy D, McCann U, Han D, et al. Pathological laughter and crying and psychiatric comorbidity after traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2015;27(4):299–303. PubMed CrossRef
- Akin FW, Murnane OD, Hall CD, et al. Vestibular consequences of mild traumatic brain injury and blast exposure: a review. Brain Inj. 2017;31(9):1188–1194. PubMed CrossRef
- Sen N. An insight into the vision impairment following traumatic brain injury. Neurochem Int. 2017;111:103–107. PubMed CrossRef
- Han P, Winkler N, Hummel C, et al. Alterations of brain gray matter density and olfactory bulb volume in patients with olfactory loss after traumatic brain injury. J Neurotrauma. 2018;35(22):2632–2640. PubMed CrossRef
- Golub VM, Reddy DS. Post-traumatic epilepsy and comorbidities: advanced models, molecular mechanisms, biomarkers, and novel therapeutic interventions. Pharmacol Rev. 2022;74(2):387–438. PubMed CrossRef
- Fordington S, Manford M. A review of seizures and epilepsy following traumatic brain injury. J Neurol. 2020;267(10):3105–3111. PubMed CrossRef
- Zimmermann LL, Martin RM, Girgis F. Treatment options for posttraumatic epilepsy. Curr Opin Neurol. 2017;30(6):580–586. PubMed CrossRef
- Finnerup NB. Nonnarcotic methods of pain management. N Engl J Med. 2019;380(25):2440–2448. PubMed CrossRef
- Ashina H, Porreca F, Anderson T, et al. Post-traumatic headache: epidemiology and pathophysiological insights. Nat Rev Neurol. 2019;15(10):607–617. PubMed CrossRef
- Levenson JC, Kay DB, Buysse DJ. The pathophysiology of insomnia. Chest. 2015;147(4):1179–1192. PubMed CrossRef
- Shenton ME, Hamoda HM, Schneiderman JS, et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012;6(2):137–192. PubMed CrossRef
- Sidaros A, Engberg AW, Sidaros K, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain. 2008;131(pt 2):559–572. PubMed CrossRef
- Warner MA, Marquez de la Plata C, Spence J, et al. Assessing spatial relationships between axonal integrity, regional brain volumes, and neuropsychological outcomes after traumatic axonal injury. J Neurotrauma. 2010;27(12):2121–2130. PubMed CrossRef
- Allegri RF. Moving from neurodegenerative dementias, to cognitive proteinopathies, replacing “where” by “what”.... Dement Neuropsychol. 2020;14(3):237–242. PubMed CrossRef
- Yue JK, Upadhyayula PS, Avalos LN, et al. The role of blood biomarkers for magnetic resonance imaging diagnosis of traumatic brain injury. Medicina (Kaunas). 2020;56(2):87. PubMed CrossRef
- Levey AI, Qiu D, Zhao L, et al. A phase II study repurposing atomoxetine for neuroprotection in mild cognitive impairment. Brain. 2022;145(6):1924–1938. PubMed CrossRef
- Qureshi KL, Upthegrove R, Toman E, et al. Post-traumatic stress disorder in UK civilians with traumatic brain injury: an observational study of TBI clinic attendees to estimate PTSD prevalence and its relationship with radiological markers of brain injury severity. BMJ Open. 2019;9(2):e021675. PubMed CrossRef
- Zhang J, Mitsis EM, Chu K, et al. Statistical parametric mapping and cluster counting analysis of [18F] FDG–PET imaging in traumatic brain injury. J Neurotrauma. 2010;27(1):35–49. PubMed CrossRef
- Guenette JP, Shenton ME, Koerte IK. Imaging of concussion in young athletes. Neuroimaging Clin N Am. 2018;28(1):43–53. PubMed CrossRef
- Shapiro JS, Silk T, Takagi M, et al. Examining microstructural white matter differences between children with typical and those with delayed recovery two weeks post-concussion. J Neurotrauma. 2020;37(11):1300–1305. PubMed CrossRef
- Henry LC, Tremblay S, Leclerc S, et al. Metabolic changes in concussed American football players during the acute and chronic post-injury phases. BMC Neurol. 2011;11:105. PubMed CrossRef
- Ellis MJ, Leiter J, Hall T, et al. Neuroimaging findings in pediatric sports-related concussion. J Neurosurg Pediatr. 2015;16(3):241–247. PubMed CrossRef
- Hutchison MG, Schweizer TA, Tam F, et al. FMRI and brain activation after sport concussion: a tale of two cases. Front Neurol. 2014;5:46. PubMed CrossRef
- Wylie G, Freeman K, Thomas A, et al. Cognitive improvement after mild traumatic brain injury measured with functional neuroimaging during the acute period. PLoS One. 2015;10(5):e0126110. PubMed CrossRef
- Fazio VC, Lovell MR, Pardini JE, et al. The relation between post concussion symptoms and neurocognitive performance in concussed athletes. Neurorehabilitation. 2007;22(3):207–216. PubMed CrossRef
- Leddy J, Wilber C, Willer B. Active recovery from concussion. Curr Opin Neurol. 2018;31(6):681–686. PubMed CrossRef
- Koponen S, Taiminen T, Portin R, et al. Axis I and II psychiatric disorders after traumatic brain injury: a 30-year follow-up study. Am J Psychiatry. 2002;159(8):1315–1321. PubMed CrossRef
- Fann JR, Burington B, Leonetti A, et al. Psychiatric illness following traumatic brain injury in an adult health maintenance organization population. Arch Gen Psychiatry. 2004;61(1):53–61. PubMed CrossRef
- Max JE, Lopez A, Wilde EA, et al. Anxiety disorders in children and adolescents in the second six months after traumatic brain injury. J Pediatr Rehabil Med. 2015;8(4):345–355. PubMed CrossRef
- Lam JA, Murray ER, Yu KE, et al. Neurobiology of loneliness: a systematic review. Neuropsychopharmacology. 2021;46(11):1873–1887. PubMed CrossRef
- Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. PubMed CrossRef
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. PubMed CrossRef
- Zucchella C, Federico A, Martini A, et al. Neuropsychological testing. Pract Neurol. 2018;18(3):227–237. PubMed CrossRef
- Soble JR, Critchfield EA, O’Rourke JJF. Neuropsychological evaluation in traumatic brain injury. Phys Med Rehabil Clin N Am. 2017;28(2):339–350. PubMed CrossRef
- Vanderploeg RD, Curtiss G, Belanger HG. Long-term neuropsychological outcomes following mild traumatic brain injury. J Int Neuropsychol Soc. 2005;11(3):228–236. PubMed CrossRef
- Mac Donald CL, Johnson AM, Cooper D, et al. Detection of blast-related traumatic brain injury in U.S. military personnel. N Engl J Med. 2011;364(22):2091–2100. PubMed CrossRef
- Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(43 suppl):84–105. PubMed CrossRef
- Nordström A, Edin BB, Lindström S, et al. Cognitive function and other risk factors for mild traumatic brain injury in young men: nationwide cohort study. BMJ. 2013;346:f723. PubMed
- Niogi SN, Mukherjee P, Ghajar J, et al. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am J Neuroradiol. 2008;29(5):967–973. PubMed CrossRef
- Wright MJ, McArthur DL, Alger JR, et al. Early metabolic crisis-related brain atrophy and cognition in traumatic brain injury. Brain Imaging Behav. 2013;7(3):307–315. PubMed CrossRef
- Fetta J, Starkweather A, Gill JM. Computer-based cognitive rehabilitation interventions for traumatic brain injury: a critical review of the literature. J Neurosci Nurs. 2017;49(4):235–240. PubMed CrossRef
- Kinnunen KM, Greenwood R, Powell JH, et al. White matter damage and cognitive impairment after traumatic brain injury. Brain. 2011;134(pt 2):449–463. PubMed CrossRef
- Vasterling JJ, Brailey K, Proctor SP, et al. Neuropsychological outcomes of mild traumatic brain injury, post-traumatic stress disorder and depression in Iraq deployed US Army soldiers. Br J Psychiatry. 2012;201(3):186–192. PubMed CrossRef
- Rogers JM, Read CA. Psychiatric comorbidity following traumatic brain injury. Brain Inj. 2007;21(13–14):1321–1333. PubMed CrossRef
- Drag LL, Spencer RJ, Walker SJ, et al. The contributions of self-reported injury characteristics and psychiatric symptoms to cognitive functioning in OEF/OIF veterans with mild traumatic brain injury. J Int Neuropsychol Soc. 2012;18(3):576–584. PubMed CrossRef
- Iverson GL, Lange RT. Mild traumatic brain injury. In Schoenberg MR, Scott JG, eds. The Little Black Book of Neuropsychology: A Syndrome-Based Approach. Springer US; 2010:697–719. CrossRef
- Janssen A, Pope R, Rando N. Clinical application of the Buffalo concussion treadmill test and the Buffalo concussion bike test: a systematic review. J Concussion. 2022;6:1–18. CrossRef
- Wheeler S, Acord-Vira A. Occupational therapy practice guidelines for adults with traumatic brain injury. Am J Occup Ther. 2023;77(4):7704397010. PubMed CrossRef
- Hardin KY, Kelly JP. The role of speech-language pathology in an interdisciplinary care model for persistent symptomatology of mild traumatic brain injury. Semin Speech Lang. 2019;40(1):65–78. PubMed CrossRef
- Kosaka B. Neuropsychological assessment in mild traumatic brain injury: a clinical overview. BC Med J. 2006;48(9):447–452.
- Jones JP, Walker MS, Drass JM, et al. Art therapy interventions for active duty military service members with post-traumatic stress disorder and traumatic brain injury. Int J Art Ther. 2018;23(2):70–85. CrossRef
- Bradt J, Magee WL, Dileo C, et al. Music therapy for acquired brain injury. Cochrane Database Syst Rev. 2010;(7):CD006787. PubMed CrossRef
- Chilton G, Vaudreuil R, Freeman EK, et al. Creative forces programming with military families: art therapy, dance/movement therapy, and music therapy brief vignettes. J Mil Veteran Fam Health. 2021;7(3):102–113. CrossRef
- Albrecht JS, Barbour L, Abariga SA, et al. Risk of depression after traumatic brain injury in a large national sample. J Neurotrauma. 2019;36(2):300–307. PubMed CrossRef
- Acabchuk RL, Brisson JM, Park CL, et al. Therapeutic effects of meditation, yoga, and mindfulness-based interventions for chronic symptoms of mild traumatic brain injury: a systematic review and meta-analysis. Appl Psychol Health Well Being. 2021;13(1):34–62. PubMed CrossRef
- Nygren-de Boussard C, Holm LW, Cancelliere C, et al. Nonsurgical interventions after mild traumatic brain injury: a systematic review. Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3 suppl):S257–S264. PubMed CrossRef
- Vitaz TW, Jenks J, Raque GH, et al. Outcome following moderate traumatic brain injury. Surg Neurol. 2003;60(4):285–291; discussion 291. PubMed CrossRef
- Ponsford JL, Downing MG, Olver J, et al. Longitudinal follow-up of patients with traumatic brain injury: outcome at two, five, and ten years post-injury. J Neurotrauma. 2014;31(1):64–77. PubMed CrossRef
- CDC, TBI. Get the Facts About TBI. 2023. https://www.cdc.gov/traumaticbraininjury/get_the_facts.html.
- Zgaljardic DJ, Durham WJ, Mossberg KA, et al. Neuropsychological and physiological correlates of fatigue following traumatic brain injury. Brain Inj. 2014;28(4):389–397. PubMed CrossRef
- Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Inj. 2015;29(2):228–237. PubMed CrossRef
- Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250–259. PubMed CrossRef
- Carter KM, Pauhl AN, Christie AD. The role of active rehabilitation in concussion management: a systematic review and meta-analysis. Med Sci Sports Exerc. 2021;53(9):1835–1845. PubMed CrossRef
This PDF is free for all visitors!
Save
Cite