ABSTRACT
Objective: To evaluate the temporal trend in young adult depression, prescription patterns of first- and second-line antidepressants, and factors influencing therapy intensification for depression stratified by sex.
Methods: A retrospective cohort of people aged ≥ 18 years with incident depression between 2006 and 2017 was extracted from the Centricity Electronic Medical Records.
Results: Among 2,201,086 people with depression (82% on antidepressants), the mean age was 47 years, 29% were male, 40% had cardiometabolic multimorbidity, and 32% were diagnosed at age < 40 years (young adult depression). Prevalence of young adult depression increased significantly from 26% to 36% with a higher proportion in females compared to males (34% vs 26%) between 2006 and 2017. Selective serotonin reuptake inhibitors (SSRIs) were the most prescribed first-line antidepressant (56%), with a prescribing rate increase from 47 per 1,000 person-years to 81 per 1,000 person-years. Among first-line antidepressant recipients, 23% had treatment intensification after a median of 17 months. Compared to those aged 60–70 years, younger males and females had a similar significantly higher treatment intensification risk (range of hazard ratio [HR], 1.09–1.46). Cardiometabolic multimorbidity was associated with a 2% (HR CI, 1.01–1.05) and 7% (HR CI, 1.05–1.09) higher treatment intensification risk in males and females, respectively, while anxiety increased the treatment intensification risk by 63% (HR CI, 1.57–1.68) in males and 57% (HR CI, 1.52–1.62) in females. Non-Whites and SSRI initiators had lower risks of treatment intensification (all HR CI < 1).
Conclusions: More than one-third of US adults with depression are aged < 40 years with an increasing trend among females. The temporal antidepressant prescribing rates were similar between sex, while significant ethnic disparity in therapy intensification was observed between sex
Prim Care Companion CNS Disord 2022;24(5):21m03162
To cite: Dibato J, Montvida O, Polonsky WH, et al. Young adult depression, antidepressant prescriptions, and therapy intensification in people with incident depression in the United States. Prim Care Companion CNS Disord. 2022;24(5):21m03162.
To share: https://doi.org/10.4088/PCC.21m03162
© 2022 Physicians Postgraduate Press, Inc.
aMelbourne EpiCentre, University of Melbourne and Melbourne Health, Melbourne, Australia
bUniversity of California, San Diego, California
cMelbourne Medical School, The University of Melbourne, Parkville, Australia
dSchool of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
*Corresponding author: Sanjoy K. Paul, PhD, The Royal Melbourne Hospital–City Campus, 7 East, Main Bldg, Grattan St, Parkville, Victoria 3050, Canada ([email protected]).
The prevalence of depression has been increasing globally, with depressive disorders being one of the leading causes of nonfatal health loss over the last 3 decades.1 The prevalence of depression among young adults has also been increasing in many countries, including the United States.2–4 However, the empirical evidence on depression is inconsistent with a high level of heterogeneity due to varying study designs and definitions of the condition in different countries.5 Globally, the prevalence of mental health disorders remains poorly understood and typically underestimated.5,6
National surveys from the United States have reported significantly higher and increasing prevalence of depression among young adults,2,3,7 while the multimorbidity among this population is also increasing.8,9 To understand the burden of depression and anxiety, the US National Institute of Mental Health’s strategic plan calls for the use of electronic medical records (EMRs) to upscale mental health research.10
While increasing prevalence of mental illness coupled with multimorbidity and the associated challenges in therapeutic management has been discussed as one of the most challenging public health issues,11,12 we are unaware of any study that evaluated the temporal trend in depression onset by age group and sex and the prevalence of cardiometabolic multimorbidity at the time of diagnosis of depression using nationally representative data from the United States.13 There is also a paucity of large nationally representative data-based studies evaluating the population-based prescriptions of specific antidepressants targeting major depressive disorder (MDD), their changes over time, and the underlying factors driving these changes from the time of depression diagnosis. As practice guidelines in recent years have started to provide more specific recommendations regarding old- and new-generation antidepressant drug classes,14,15 details of actual prescriptions of antidepressants in the real world could be very informative for clinicians and health policymakers in benchmarking their performance in depression treatment. While claims data were used to evaluate the therapy utilizations in previous studies,16–18 large EMRs offer unparalleled opportunities to explore risk factors and comorbidities in people with depression to better understand the changing dynamics for successful disease management at the population level.19 This study addresses the unmet need for real-world evidence to inform the current global debate on the emerging challenges in the efficient management of mental health–related issues.
Using patient-level longitudinal data in people with incident depression from US nationally representative large EMRs, we sought to (1) evaluate the temporal trend in young adult depression, (2) explore the overall trend in antidepressant prescription rates, (3) explore the patterns of first- and second-line antidepressant prescriptions by drug class and generic drug, and (4) identify factors associated with changes to antidepressant prescription stratified by sex. We also compared estimated prevalence rates of depression from the EMRs with those reported in the US national surveys.
METHODS
Data
The Centricity Electronic Medical Records (CEMR) provides patient-level data from over 40,000 ambulatory and primary care medical practices based across all US states. The CEMR is generally representative of the US population with respect to demographics, major disease prevalence, and cardiometabolic risk factors reported in the US national health surveys20 and has been extensively used for epidemiologic and public health studies.21–23 The CEMR provides comprehensive longitudinal patient-level information on demographics, anthropometrics, clinical and laboratory measures, medication usage, and diseases. Prescription data include generic ingredients of both inpatient and outpatient medications with their respective prescription start and stop dates.
Cohort Identification
Using a clinically guided machine learning algorithm24,25 with information from ICD-CM disease codes and antidepressant prescriptions for any mental illness, a cohort of people diagnosed with depression was identified (Supplementary Tables 1 and 2). The algorithm is described in the methods section of the Supplementary Material and in Supplementary Figure 1. The study cohort of newly identified depression was formed with the following conditions: (1) known age and sex, (2) aged 18–70 years at the time of depression diagnosis by clinical code or prescription use, (3) starting from January 1, 2006, and (4) date of diagnosis at least 12 months after registering in the EMR. The date of depression diagnosis or first prescription date of an antidepressant was defined as the index date (Supplementary Figure 2).
Study Variables
Data on prescriptions, disease diagnoses, demographics, and clinical and laboratory measurements were extracted. A full description and the methodology for demographic, clinical, and medication variable extraction and assessment from the CEMR have been described.26 Cardiometabolic multimorbidity was defined as having at least 2 cases of atherosclerosis cardiovascular diseases, heart failure, microvascular disease including chronic kidney disease, cancer, type 1 diabetes mellitus, type 2 diabetes mellitus, ≥ class 2 obesity (body mass index ≥ 35 kg/m2), hypertension, and dyslipidemia. A disease was considered as prevalent at baseline if its first available diagnostic date was on or prior to the index date.
Time to Treatment Intensification
Among people receiving antidepressants and intensified by either adding or switching to a second-line antidepressant, time to treatment intensification was calculated as the number of years between the first prescription date and the first observed date with intensification. Those without intensification during follow-up were “censored,” and the time to treatment intensification was calculated as the number of years between the index date and the study observation end date (end date included date of death or date the patient left practice or the last date of data collection). Patients who had dose titration within the same drug could not be identified because of nonavailability of complete data on doses for individual therapies.
Ethics Statement
According to the US Department of Health and Human Services Exemption 4 (CFR 46.101[b][4]), this study is exempt from ethics approval from an institutional review board and informed consent.
Statistical Methods
Baseline characteristics were summarized by number (%), mean (SD), or median (first quartile, third quartile) as appropriate. To establish clarity on the use of antidepressants with or without a clinical diagnosis code for depression, the study cohorts were divided into 3 groups: (1) individuals with a diagnosis code for depression and prescribed an antidepressant, (2) individuals with a diagnosis code for depression but not prescribed an antidepressant, and (3) individuals taking an antidepressant without a clinical diagnosis for depression. The age groups at the time of diagnosis of depression were categorized as 18–29, 30–39, 40–49, 50–59, and 60–70 years. Representativeness of the data was assessed by computing prevalence of depression and any mental illness using methods described elsewhere27 and comparing these estimates with those from national surveys.28–32
The rates per 1,000 person-years of initiating individual antidepressant drug classes were estimated using the standard life table technique. Person-years was measured from the date of clinical diagnosis of depression to the earliest of the following: prescription date of the respective antidepressants, date of death, date the patient left the practice, or the last date of data collection from that practice. To evaluate the changing patterns in individual trends for the prescription rates, joinpoint regression based on annual percent change estimates was obtained.33
Among those who initiated at least 1 antidepressant monotherapy, the proportion of individuals who initiated second-line therapy and the median time to second-line therapy initiation were calculated overall and by first-line antidepressant drug class. Accounting for potential nonproportionality, the weighted Cox regression model34 was used to determine factors associated with the risk of antidepressant therapy intensification separately for males and females, and the results were expressed as hazard ratios (95% CI). Missing covariate data were included as a categorical field to retain sample size.
RESULTS
Representativeness of the EMRs
From all available adult patient–level data from 2006 to 2017 (aged ≥ 18 years and at least 1 year of being active in the EMRs, n = 19,425,810), the proportions of people with any mental illness/depression were 28.9% (95% CI, 28.8–29.0)/21.4% (95% CI, 21.3–21.5). The overall prevalence of depression during the 2012–2013 study period was 18% (95% CI, 18.1–18.2), which is very close to the 21% reported in the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III) survey during the same period.28 The prevalence of any mental illness estimated during the periods 2010/2013 was 20.1% (95% CI, 20.1–20.2)/24.3% (95% CI, 24.2–24.3), which is similar to 20%/19% reported in the National Survey on Drug Use and Health survey reports.29,30 The trends in the prevalence of depression and any mental illness from the CEMR across different demographics were comparable to those from the US national surveys (Supplementary Table 3).
Cohort Characteristics
A total of 2,201,086 patients identified with incidence depression met the study inclusion criteria (Supplementary Figure 2), with a median (Q1, Q3) follow-up of 3.9 (1.5, 6.7) years (Table 1). The mean (SD) age was 47 (15) years, with 29% male, 37% smokers, 40% obese, 15% diabetic, 7% with atherosclerosis cardiovascular disease, 40% with cardiometabolic multimorbidity, and 16% diagnosed with other mental illnesses including anxiety. Approximately 32% of the cohort was diagnosed before age 40 years, and the proportion of young adult depression increased from 26% in 2006% to 36% in 2017, with a significantly higher proportion of females versus males (34% vs 26%, Figure 1A). The baseline cardiometabolic multimorbidity for males/females was 50%/35%.
Trend in Antidepressant Prescriptions
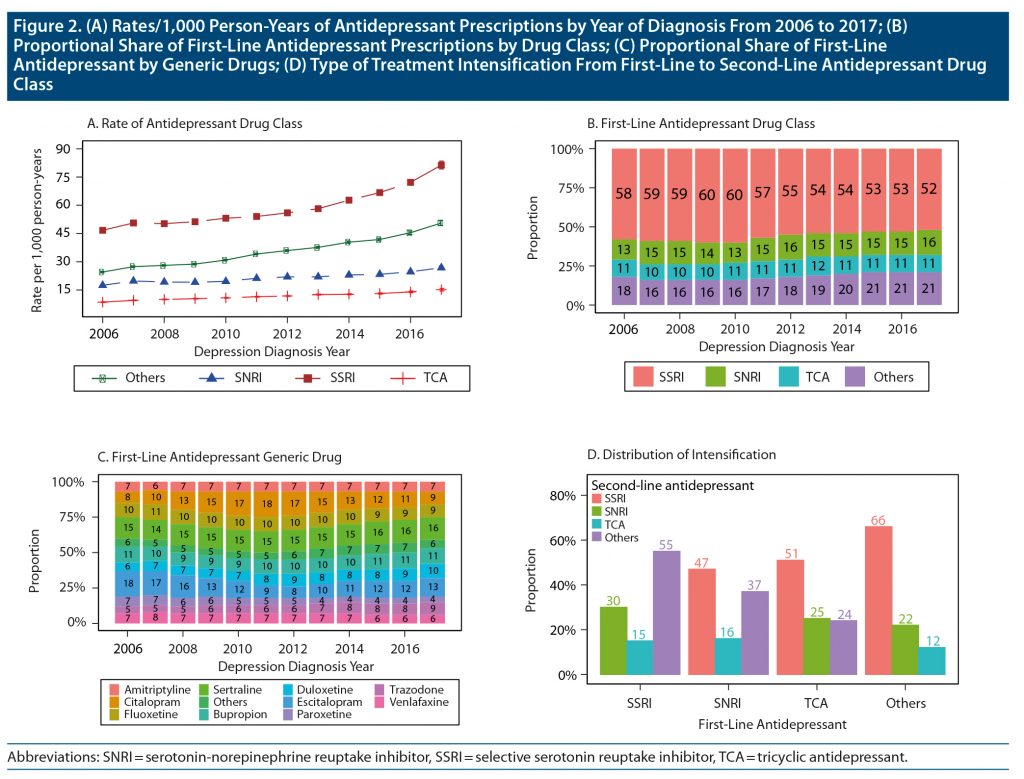
Among those diagnosed with depression, the proportion not receiving any therapeutic intervention for depression in males/females increased from about 7%/6% in 2006 to 18%/17% in 2017 (Figure 1B). The rates of initiation of different identified classes of antidepressants by the year of diagnosis are provided in Figure 2A. Selective serotonin reuptake inhibitor (SSRI) prescription rates increased significantly (rate [95% CI]/1,000 person-years from 47 [46–48] in 2006 to 81 [79–83] in 2017). The prescribing rates of other antidepressants increased from 24 (95% CI, 23–25) to 51 (95% CI, 49–52)/1,000 person-years, while the prescribing rates of serotonin-norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs) remained relatively unchanged. Similar patterns were observed among males and females (Supplementary Figures 3A and 3B).
A further evaluation of the overall antidepressant prescription rates by age and sex shows significant higher and recent increases in the rates of antidepressant prescription (mostly SSRIs) among male and female adults aged 18–39 years, while a constant yearly increase in prescription rates for the other age groups was observed since 2006 (Supplementary Figure 4, Supplementary Table 4).
Patterns of First-Line Antidepressant Prescription
In the eligible cohort, 1,797,863 (82%) individuals received at least 2 prescriptions for antidepressants. The most prescribed first-line drug classes were SSRIs (56%: mostly citalopram, escitalopram, and sertraline) followed by “others” (19%: mostly bupropion and trazodone), which were consistent from 2006 to 2017, similar for males and females (Figures 2B and 2C, Supplementary Figures 3C and 3D).
Patterns of Antidepressant Treatment Intensification
Of those who initiated antidepressants, 405,086 (23%) had a prescription intensification with an overall median (Q1, Q3) of 17 (6, 37) months of duration of first-line antidepressant use before therapy intensification. After a change from SSRI, the most common second-line treatments were 55% other antidepressants followed by 30% SNRIs overall; 60% other antidepressants and 27% SNRIs in males; and 53% other antidepressants and 32% SNRIs in females (Figure 2D, Supplementary Figures 3E and 3F). Among those who initiated SNRIs, TCAs, and other antidepressants, SSRI was the most common second-line choice, with higher percentages of SSRI choice consistently recorded among females. Compared to males, females were 22% more likely to intensify therapy, with the observed trends consistent across all age groups (P < .01). Details for all the possible intensification between the drug classes and their respective generic ingredients are presented in Supplementary Table 5.
Factors Associated With Antidepressant Treatment Intensification
Compared to people aged 60–70 years at baseline, the risk of therapy intensification was progressively significantly higher in younger age groups for both sexes (Figure 3, Supplementary Table 6). Overall, compared to those aged 60–70 years, the adjusted hazard ratios (HR) (95% CI) for males/females in the age groups 18–29, 30–39, 40–49, and 50–59 years were 1.19 (1.14–1.24)/1.36 (1.32–1.40), 1.25 (1.20–1.31)/1.42 (1.38–1.46), 1.25 (1.20–1.30)/1.35 (1.32–1.39), and 1.14 (1.09–1.19)/1.16 (1.14–1.19), respectively. Non-White ethnic groups had lower risks of treatment intensification compared to Whites: the adjusted HR (95% CI) for Black/others in males was 0.86 (0.82–0.89)/0.96 (0.92–0.99) and in females was 0.87 (0.79–0.96)/0.86 (0.82–0.90). People with cardiometabolic multimorbidity had higher risk: HR (CI) of therapy intensification for males/females: 1.02 (1.01–1.05)/1.07 (1.05–1.09). Anxiety was associated with higher therapy intensification risk: males/females: 1.63 (1.57–1.68)/1.57 (1.52–1.62). Males and females on SSRIs were significantly less likely to intensify to second-line therapies (range of HR CI, 0.73–0.92), while those on SNRIs had higher risk of therapy intensification (range of HR CI, 1.03–1.36).
DISCUSSION
With global concerns about increasing prevalence of depression among young adults, there is an urgent need to understand the risk dynamics and treatment patterns in people of different ages from the time of diagnosis of depression. The novelty of this study includes the comprehensive evaluation of temporal trends in young adult depression and multimorbidity in males and females, the rates of utilization of different classes of antidepressants, a holistic evaluation of choices of different generic ingredients by the order of initiation, and the factors associated with therapy intensification in more than 2 million people from the United States with incident depression over a decade using large representative EMRs. Our study also highlights sex-based differences in the patterns of treating patients with incident depression in real-life settings.
For a holistic evolution of risk dynamics in people with depression, use of large representative EMRs containing detailed information on risk factors and comorbidities is essential, leading to our ability to conduct robust population-level outcome studies. Fundamental to this is the evaluation of the representativeness of EMRs with survey data in terms of major distribution characteristics. The observed prevalence rates of depression from CEMR during 2006, 2008, and 2012–2013 were similar to those reported in the Behavioral Risk Factor Surveillance System and NESARC-III surveys during the same periods.28,31,32 Similarities in the trend of any mental illness prevalence by sex, age, and ethnicity were also observed from other US national surveys (Supplementary Table 1).29,30 With the extensive data mining of the mental illnesses using related clinical diagnoses and prescriptions for antidepressants, the comparability of the proportions of people with depression and the distribution of their clinical characteristics suggest the usability of the EMRs in conjunction with claims and registry–based data for the much-needed population-level evidence generation in mental health, especially to support the US Food and Drug Administration initiative on “Exploring the Use of Real-World Data to Generate Real-World Evidence in Regulatory Decision-Making.”35,36
We observed that more than 30% of the cohort were diagnosed with depression at an early age, and the proportion of young adult depression significantly increased by 10% between 2006 and 2017. In addition, 40% of cardiometabolic multimorbidity was recorded in the study cohort with significantly higher proportions in males compared to females (50% vs 35%). In the absence of any population-level study, a detailed exploration of the dynamics of young adult depression and how multimorbidity is playing a role in this context is warranted.
We observed lower earlier and significantly higher recent antidepressant prescriptions rates among young adults compared to older age groups. A possible explanation for the observed trends could be a result of the observed link between SSRIs and increase in suicide rates prior to 2006, which led to a decrease in the use of antidepressants, and the economic downturn in 2008, which led to an increase in MDD and a consequent rise in antidepressant use among young adults.37–39
At present, first-line pharmacologic treatment of MDD in adults includes SSRIs, SNRIs, and other new-generation antidepressants.14,15 In the presence of nonresponse or side effects from the first-line agent, different therapy intensification strategies including modification of the initial drug dosage, switching to a different antidepressant, or augmentation by another drug are recommended. Few US-based surveys40,41 and US claims data–based studies17,18 have evaluated the utilization patterns of antidepressants in people with established depression. Kern and colleagues17 explored 2014–2019 US claims data and reported that SSRIs were the most common first-line treatment, and 20%–40% of patients had treatment combination after first-line therapies.
As observed in the CEMR, SSRIs with a favorable safety profile remained the most prescribed and increasingly popular antidepressants, while usage of other classes of therapies appeared to remain the same over the last decade. We also found 23% of those who initiated antidepressants intensified to second-line treatments. Although there is no strong evidence for the relative advantages of intensification within or between classes in the management of MDD,42 in this study we assessed risk factors that could be associated with therapy intensification between therapy classes. Milea and colleagues16 evaluated factors associated with antidepressant treatment changes using US claims data, reporting 23% treatment change after first-line therapies, and found first-line treatment and other mental illnesses to be associated with treatment change. We found that females, smokers, comorbidities, other mental illnesses, and SNRI initiators were factors significantly associated with higher risk of therapy intensification, with younger adults receiving significantly higher therapy intensification compared to those aged ≥ 60 years. On the contrary, SSRI initiators and non-Whites were significantly less likely to intensify with a second-line therapy, and this was consistent by sex.
While lack of reliable information on medication adherence is a common problem in all clinical studies, detailed validation studies of US EMRs suggest a high level of agreement between EMR prescription data and pharmacy claims data, especially in chronic diseases.43 In this study, we found a significant proportion of people who were prescribed antidepressants without a diagnosis code for depression in the EMR. This finding suggests that there is significant undercoding of clinical diagnoses in the primary and ambulatory care systems—a common issue demanding administrative intervention. Also, while we carefully chose antidepressants used for the treatment of depression only, a few people might have received this medication for other conditions as well, which is difficult to tease out from EMRs. Our extensive data-mining approach could guide the future development of dedicated pharmaco-epidemiologic studies using EMRs to generate robust real-world evidence in people with mental illness, while acknowledging the fundamental weaknesses of EMRs in relation to the absence of any therapy use indication, dosing, and general adherence.20,23 In addition, other selection biases and residual confounding issues inherent in any EMR-based outcome study may remain. Residual bias may be present in the identification of incident depression cases. However, any potential inaccuracies with these input parameters were unlikely to have changed the conclusions of our study.
This study has several strengths including use of large nationally representative population-based data with significant follow-up time, availability of data on patient characteristics, disease events, prescriptions, and laboratory measures. We also validated the representativeness of a US primary care database with the national survey report, establishing suitability of this EMR for clinical and pharmaco-epidemiologic studies. Although antidepressants prescribed in real-world settings do not always conform to practice guidelines,18 we have addressed the long-term real-world treatment patterns and empirical evidence on identifying high-risk individuals with depression following initiation of first-line therapy.
In conclusion, with increasing prevalence of young adult depression in the United States, cardiometabolic multimorbidity being one of the major factors driving depression incidence, and significant ethnic disparity in therapy management, further exploration is needed in the context of long-term safety in people with depression. This study demonstrates the usability of EMRs to generate the much-needed real-world evidence in people with mental illness in the United States.
Submitted: September 30, 2021; accepted February 16, 2022.
Published online: September 6, 2022.
Relevant financial relationships: Dr Paul is currently a full-time employee of AstraZeneca and has acted as a consultant and/or speaker for Novartis, GI Dynamics, Roche, AstraZeneca, Guangzhou Zhongyi, and Amylin. He has received grants in support of investigator and investigator-initiated clinical studies from Merck, Novo Nordisk, AstraZeneca, Hospira, Amylin, Sanofi-Aventis, and Pfizer. Drs Polonsky, Chin, and Montvida and Mr Dibato report no relevant financial relationships.
Funding/support: None.
Acknowledgments: Melbourne EpiCentre gratefully acknowledges the support from the National Health and Medical Research Council and the Australian government’s National Collaborative Research Infrastructure Strategy initiative through Therapeutic Innovation Australia.
Supplementary material: See accompanying pages.
Clinical Points
- More than one-third of US adults with depression are aged < 40 years, with significant increasing trend over the past decade.
- Approximately 1 in 2 adults treated for depression have suboptimal response after first-line antidepressants and would need some form of treatment intensification.
- Age at diagnosis, ethnicity, and cardiometabolic multimorbidity are the major sociodemographic and nonpsychiatric risk factors for antidepressant prescription changes among US adults diagnosed with depression.
References (43)

- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. PubMed CrossRef
- Villarroel MA, Terlizzi EP. Symptoms of depression among adults: United States, 2019. NCHS Data Brief. 2020;(379):1–8. PubMed
- Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief. 2018;(303):1–8. PubMed
- Slee A, et al. Trends in generalised anxiety disorders and symptoms in primary care: UK population-based cohort study. Br J Psychiatry. 2021;218(3)158–164. PubMed
- Furukawa TA. An epidemic or a plague of common mental disorders? Acta Psychiatr Scand. 2019;140(5):391–392. PubMed CrossRef
- Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet. 2009;374(9690):609–619. PubMed CrossRef
- Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. PubMed CrossRef
- King DE, Xiang J, Pilkerton CS. Multimorbidity trends in United States adults, 1988–2014. J Am Board Fam Med. 2018;31(4):503–513. PubMed CrossRef
- Whitty CJM, MacEwen C, Goddard A, et al. Rising to the challenge of multimorbidity. BMJ. 2020;368:l6964. PubMed CrossRef
- National Institute of Mental Health. Strategic Plan for Research 2020. NIMH website. Accessed August 12, 2021. https://www.nimh.nih.gov/sites/default/files/documents/about/strategic-planning-reports/2020_nimh_strategic_plan_508.pdf
- Baingana F, al’Absi M, Becker AE, et al. Global research challenges and opportunities for mental health and substance-use disorders. Nature. 2015;527(7578):S172–S177. PubMed CrossRef
- Birk JL, Kronish IM, Moise N, et al. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019;38(9):802–811. PubMed CrossRef
- Hsiao CJ, Dymek C, Kim B, et al. Advancing the use of patient-reported outcomes in practice: understanding challenges, opportunities, and the potential of health information technology. Qual Life Res. 2019;28(6):1575–1583. PubMed CrossRef
- American Psychological Association. Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts. APA website. Accessed August 13, 2021.
- Cleare A, Pariante CM, Young AH, et al; Members of the Consensus Meeting. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2015;29(5):459–525. PubMed CrossRef
- Milea D, Guelfucci F, Bent-Ennakhil N, et al. Antidepressant monotherapy: a claims database analysis of treatment changes and treatment duration. Clin Ther. 2010;32(12):2057–2072. PubMed CrossRef
- Kern DM, Cepeda MS, Defalco F, et al. Treatment patterns and sequences of pharmacotherapy for patients diagnosed with depression in the United States: 2014 through 2019. BMC Psychiatry. 2020;20(1):4. PubMed CrossRef
- Gauthier G, Guérin A, Zhdanava M, et al. Treatment patterns, healthcare resource utilization, and costs following first-line antidepressant treatment in major depressive disorder: a retrospective US claims database analysis. BMC Psychiatry. 2017;17(1):222. PubMed CrossRef
- Castillo EG, Olfson M, Pincus HA, et al. Electronic health records in mental health research: a framework for developing valid research methods. Psychiatr Serv. 2015;66(2):193–196. PubMed CrossRef
- Montvida O, Dibato J, Paul S. Evaluating the representativeness of US Centricity Electronic Medical Records with reports from Centers for Disease Control and Prevention: office visits and cardiometabolic conditions. (preprint). JMIR Med Inform. 2020;8(6)e17174. CrossRef
- Dibato JE, et al. Association of cardiometabolic multimorbidity and depression with cardiovascular events in early-onset adult type 2 diabetes: a multiethnic study in the US. Diabetes Care. 2021;44(1):231–239. PubMed
- Paul SK, Bhatt DL, Montvida O. The association of amputations and peripheral artery disease in patients with type 2 diabetes mellitus receiving sodium-glucose cotransporter type-2 inhibitors: real-world study. Eur Heart J. 2021;42(18):1728–1738. PubMed CrossRef
- Montvida O, Shaw J, Atherton JJ, et al. Long-term trends in antidiabetes drug usage in the US: real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care. 2018;41(1):69–78. PubMed CrossRef
- Marie Ingram W, et al. Defining major depressive disorder cohorts using the EHR: multiple phenotypes based on ICD-9 codes and medication orders. bioRxiv. 2018:227561.
- Deferio JJ, Levin TT, Cukor J, et al. Using electronic health records to characterize prescription patterns: focus on antidepressants in nonpsychiatric outpatient settings. JAMIA Open. 2018;1(2):233–245. PubMed CrossRef
- Montvida O, et al. Data mining approach to estimate the duration of drug therapy from longitudinal electronic medical records. Open Bioinform J. 2017;10(1):1–15. CrossRef
- Rassen JA, Bartels DB, Schneeweiss S, et al. Measuring prevalence and incidence of chronic conditions in claims and electronic health record databases. Clin Epidemiol. 2018;11:1–15. PubMed CrossRef
- Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. PubMed CrossRef
- Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-42, HHS Publication No. (SMA) 11-4667. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2012. SAMHSA website. Accessed June 26, 2021. https://www.samhsa.gov/data/sites/default/files/2k10MH_Findings/2k10MH_Findings/2k10MHResults.htm#Ch2
- Lipari RN. H.S., Hughes A. Substance Use and Mental Health Estimates from the 2013 National Survey on Drug Use and Health: Overview of Findings. 2014 NIH website. Accessed June 27, 2021. https://www.ncbi.nlm.nih.gov/books/NBK385055/
- Home CDC. Current Depression Among Adults—United States, 2006 and 2008. CDC website. Accessed June 26, 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5938a2.htm
- Centers for Disease Control and Prevention. Mental Illness Surveillance Among Adults in the United States. CDC website. Accessed June 27, 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/su6003a1.htm
- National Cancer Institute. Joinpoint Trend Analysis Software. Surveillance website. Accessed June 27, 2021. https://surveillance.cancer.gov/joinpoint/
- Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Stat Med. 2009;28(19):2473–2489. PubMed CrossRef
- Li M, Chen S, Lai Y, et al. Integrating real-world evidence in the regulatory decision-making process: a systematic analysis of experiences in the US, EU, and China using a logic model. Front Med (Lausanne). 2021;8:669509. PubMed CrossRef
- Department of Health and Human Services. Exploring the use of Real-World Data to Generate Real-World Evidence in Regulatory Decision-Making (U01) Clinical Trials Optional. NIH website. Accessed August 14, 2021. https://grants.nih.gov/grants/guide/rfa-files/RFA-FD-20-030.html
- Jick H, Kaye JA, Jick SS. Antidepressants and the risk of suicidal behaviors. JAMA. 2004;292(3):338–343. PubMed CrossRef
- Libby AM, Brent DA, Morrato EH, et al. Decline in treatment of pediatric depression after FDA advisory on risk of suicidality with SSRIs. Am J Psychiatry. 2007;164(6):884–891. PubMed CrossRef
- Mehta K, Kramer H, Durazo-Arvizu R, et al. Depression in the US population during the time periods surrounding the great recession. J Clin Psychiatry. 2015;76(4):e499–e504. PubMed CrossRef
- Moore TJ, Mattison DR. Adult utilization of psychiatric drugs and differences by sex, age, and race. JAMA Intern Med. 2017;177(2):274–275. PubMed CrossRef
- Luo Y, et al. National prescription patterns of antidepressants in the treatment of adults with major depression in the US between 1996 and 2015: a population representative survey-based analysis. Front Psychiatry. 2020;11(35):fpsyt.2020.00035.
- Rush AJ, Trivedi MH, Wisniewski SR, et al; STAR*D Study Team. Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med. 2006;354(12):1231–1242. PubMed CrossRef
- Rowan CG, Flory J, Gerhard T, et al. Agreement and validity of electronic health record prescribing data relative to pharmacy claims data: a validation study from a US electronic health record database. Pharmacoepidemiol Drug Saf. 2017;26(8):963–972. PubMed CrossRef
Please sign in or purchase this PDF for $40.
Save
Cite