Sometimes the most lingering injuries are the ones we can’t see. Military veterans know that all too well. According to the Traumatic Brain Injury Center of Excellence, doctors have diagnosed more than 460,000 service members with a first-time TBI since 2000.
Finally, relief might be on the horizon. Stanford researchers have discovered that ibogaine, a plant-based psychoactive compound, showed improvements in “depression, anxiety and functioning among veterans with traumatic brain injuries.
The new study, which Nature Medicine published online Jan. 5, includes detailed data on nearly three dozen U.S. special forces veterans.
“No other drug has ever been able to alleviate the functional and neuropsychiatric symptoms of traumatic brain injury,” Nolan Williams, MD, an associate professor of psychiatry and behavioral sciences said in a press release announcing the findings. “The results are dramatic, and we intend to study this compound further.”
Veterans Desperate for Treatment
The U.S. Department of Veterans Affairs defines traumatic brain injury as an injury to the head that disrupts the normal functioning of the brain.
“For Veterans of Operations Enduring Freedom, Iraqi Freedom and New Dawn (OEF/OIF/OND), the sources of blast injury most often are improvised explosive devices (IED), also called roadside bombs; artillery, rocket and mortar shells, traps, aerial bombs, and rocket-propelled grenades,” according to the agency’s website. “TBIs also can be caused by motor vehicle accidents, falls, or any incident involving a sudden blow or jolt to the head.”
Ibogaine, according to the researchers, “is a naturally occurring compound found in the roots of the African shrub iboga, and it has been used for centuries in spiritual and healing ceremonies. More recently, it has gained interest from the medical and scientific communities for its potential to treat opioid and cocaine addiction, and research has suggested that it increases signaling of several important molecules within the brain, some of which have been linked to drug addiction and depression.”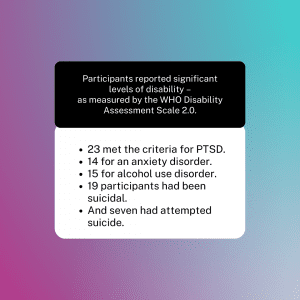
“Veterans are on the front line of our national defense, but here they are on the front line of cutting-edge research that has the potential to help millions of people – both in and out of uniform,” VETS Co-Founder and CEO Amber Capone explained. “We remain laser-focused and dedicated to our mission of supporting access to psychedelic-assisted therapies for veterans and advancing research into their safety and efficacy. Our collaboration with Stanford University and Dr. Williams is a major step forward in proving the potential of ibogaine for treating PTSD and TBI.”
But ibogaine has languished as a Schedule I drug for more than 50 years. As a result, U.S. medical professionals couldn’t take advantage of it. Canadian and Mexican clinics treat patients regularly with the drug.
“There were a handful of veterans who had gone to this clinic in Mexico and were reporting anecdotally that they had great improvements in all kinds of areas of their lives after taking ibogaine,” Williams added. “Our goal was to characterize those improvements with structured clinical and neurobiological assessments.”
Leveraging Treatment for Research
Williams and his Stanford colleagues worked with Veterans Exploring Treatment Solutions (VETS), a leading nonprofit committed to preventing veteran suicide, to study 30 veterans with a history of TBI who exhibited clinically severe psychiatric symptoms and functional disabilities. These veterans had already separately arranged for a dual treatment of magnesium and ibogaine at a clinic in Mexico.
Ahead of the treatment, the researchers measured the participants’ levels of PTSD, anxiety, depression, and functioning based on both self-reported questionnaires and clinician-administered assessments. Participants then traveled to the Ambio Life Sciences Clinic in Mexico, where they took oral ibogaine and magnesium. Stanford then hosted the returning veterans for post-treatment assessments.
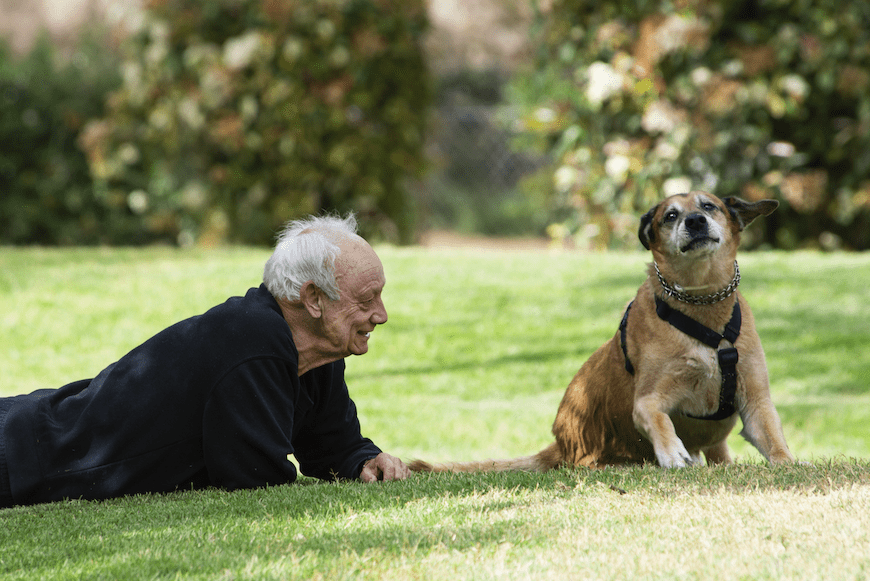
“These men were incredibly intelligent, high-performing individuals who experienced life-altering functional disability from TBI during their time in combat,” Williams reported. “They were all willing to try most anything that they thought might help them get their lives back.”
Game-changing Outcomes for Veterans
On average, the researchers revealed that ibogaine treatment immediately led to significant improvements in functioning, PTSD, depression, and anxiety. Better still, those effects persisted for at least 30 days after treatment.
Before treatment, the study participants had an average disability rating of 30.2 on the disability assessment scale, translating to “mild to moderate disability.” One month after treatment, that rating jumped to 5.1, indicating no disability whatsoever.
Participants also revealed dramatic average reductions of 88 percent in PTSD symptoms, 87 percent in depression symptoms, and 81 percent in anxiety symptoms. Finally, cognitive testing also showed improvements in concentration, information processing, memory, and impulsivity.
But the stories these veterans tell convey more than statistical analysis could:
“I wasn’t willing to admit I was dealing with any TBI challenges. I just thought I’d had my bell rung a few times — until the day I forgot my wife’s name. Since [ibogaine treatment], my cognitive function has been fully restored. This has resulted in advancement at work and vastly improved my ability to talk to my children and wife.”
– Craig, a 52-year-old study participant from Colorado who served 27 years in the U.S. Navy.
“Before the treatment, I was living life in a blizzard with zero visibility and a cold, hopeless, listless feeling. After ibogaine, the storm lifted.”
– Sean, a 51-year-old veteran from Arizona with six combat deployments.
Critically, the researchers found no serious side effects or cardiac issues, but they did stress the need for more analysis.
Further Reading
Pimavanserin 34 mg at Bedtime for the Treatment of Insomnia in PTSD
Functional Disability in US Military Veterans
Patient Functioning, Life Engagement, and Treatment Goals in MDD