When Raynaud’s phenomenon comes up as a patient complaint it is often in relation to frigid winter temperatures or perhaps in reaction to extreme stress. A case study described in The Primary Care Companion for CNS Disorders points to another cause that is relevant to psychiatrists: as a side effect to stimulants.
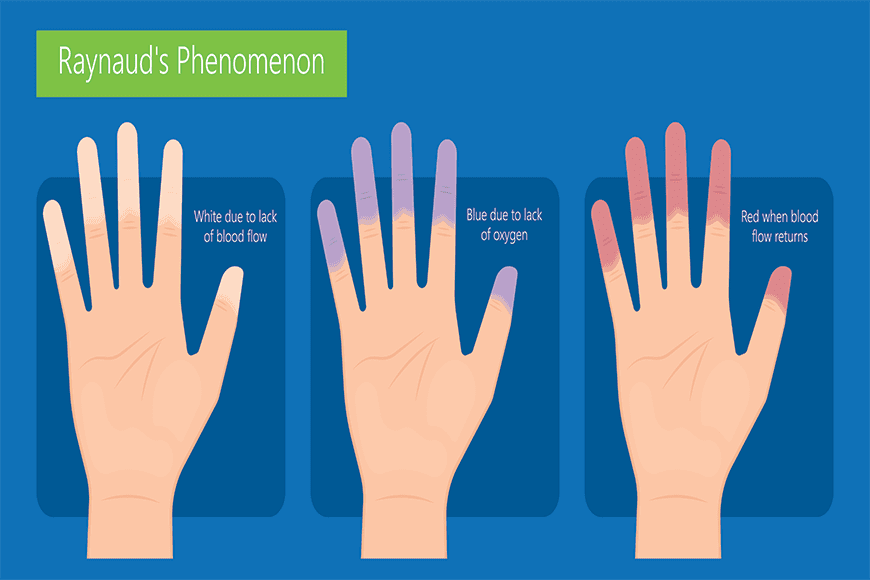
Raynaud’s typically affects the fingers and toes with a stinging numbness brought on by vasospasm, the constriction of the smaller arteries that supply blood to those extremities. The stricken area often turns a pale shade of white and then blue-to-purple. Typically, it takes about 15 minutes for the afflicted area to return to normal, a process that can include throbbing, pain, and swelling.
In the clinical vignette described by experts from the Clarion Psychiatric Center in Pennsylvania, a 15-year-old female patient was diagnosed with oppositional defiant disorder and ADHD combined type. She was initially treated with 10 mg of Adderall with a plan to increase to 20 mg after 2 weeks.
One week after the start of treatment, the patient began to experience daily episodes of Raynaud’s. She did have a history of the condition prior to taking the psychostimulant that was triggered in the winter after her evening showers. These bouts occurred once three 3 a week or so and typically presented as a purple fourth finger bilaterally and purple feet and legs bilaterally with mottling.
However, when the condition was triggered by Adderall, she was plagued by symptoms daily. Each episode lasted for approximately 2 hours with no sensory changes or weakness. As soon as she discontinued Adderall, her episodes subsided. She was switched to guanfacine extended release, and was doing well on this medication with a moderate reduction in symptoms.
This case underscores Raynaud’s phenomenon as a rare but noteworthy side effect that has been reported with the use of psychostimulants, particularly mixed salt amphetamines. These drugs have higher potency and cause more peripheral vasoconstriction than methylphenidate. Methylphenidate is primarily a reuptake inhibitor of catecholamines, but mixed salt amphetamines, in addition to reuptake inhibition, also release catecholamines, the clinicians noted in their write up.
The authors of this paper urge clinicians to do a careful history when prescribing these medications, particularly if a patient has a history of rheumatological disorders. Peripheral manifestations of the stimulants are worse in such patients as they run the risk of developing gangrene or even the need for amputations.