This week, The Journal of Clinical Psychiatry presented the case study of a 65-year-old man diagnosed with amyotrophic lateral sclerosis (ALS). The psychological distress described in this paper is both expected and heartbreaking.
16,000 Americans Live With ALS
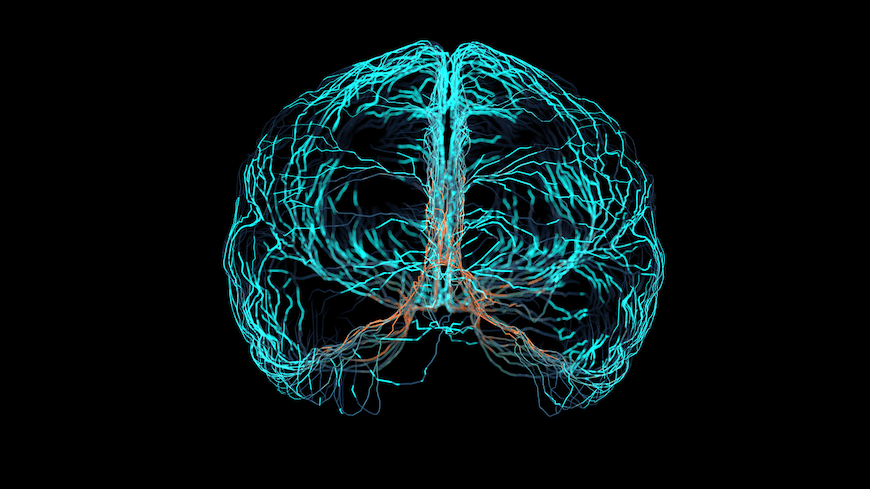
ALS is a neurodegenerative disease. Also known as Lou Gehrig’s disease, it’s a progressive neurodegenerative disorder that primarily affects nerve cells in the brain and spinal cord, leading to muscle weakness, atrophy, and paralysis. Symptoms include difficulty in speaking, swallowing, and breathing, along with general muscle weakness and twitching.
Most ALS patients are diagnosed through a combination of clinical examination, electromyography (EMG), and other tests to rule out similar conditions. The disease can be genetic in some cases, with about 5-10 percent of cases being familial. It usually appears between the ages of 40 and 70, with an average age of onset at 55. The median survival rate after diagnosis is 3 to 5 years, though some patients may live longer.
Patients feel its profound impact both physically and mentally. The subject featured in this case is no exception.
Michael’s Story
Michael had been living with ALS for 12 years. His gradual deterioration left him with no voluntary muscle control and he relied on technology and caregivers for communication and daily activities. He experienced intense psychiatric anguish, including depression and anxiety. This is common in ALS patients due to the unpredictable and terminal nature of the disease. Although ALS is always complicated to treat, Michael’s case was particularly challenging, given his personal history of depression and the additional stress of a divorce.
Michael’s care included psychotherapy and psychopharmacology, tailored to his specific needs. Psychotherapy involved a combination of cognitive behavioral therapy, dialectical behavior therapy, and acceptance and commitment therapy. His team hoped this approach would help Michael manage his mood and stress, and improve his relationships, especially with his children.
The psychopharmacological treatment approach to his mental health was not as straightforward. His response to medications was not ideal and he could not tolerate drugs that worsened his respiratory function.
A Need for Compassion and Clarity
The authors noted a lack of standardized guidelines for treating the emotional and cognitive symptoms of ALS, making his individualized treatment essential. Michael’s case underscores the necessity of a multidisciplinary approach in treating ALS patients. Clinicians can’t simply address the physical aspects of the disease. They also have to pay attention to the psychological, emotional, and existential challenges these patients face.
Michael was fortunate in that his care team included the perspectives of various healthcare professionals, each contributing to a comprehensive understanding of his condition. They understood the importance of creating a holistic and personalized treatment plan that went beyond managing physical symptoms to include psychological support and existential considerations. Michael’s story is a poignant reminder of the nuanced and multifaceted nature of care required for all ALS patients.
IN OTHER PSYCHIATRY AND NEUROLOGY NEWS
- An additional case report reviews the medical journey of two sisters with a rare case of induced olfactory reference syndrome.
- A review of the South Florida Cognitive Screener, an 8-item self-report instrument developed to capture the most common cognitive, functional, and behavioral complaints typically reported early in the process of cognitive decline.
- Part 4 in an ongoing series by Chittaranjan Andrade, MD on exercise and health covers what to do, how to do it, and why you should.
- A new CDC report estimates that 1.3 percent of U.S. adults – more than three million people – live with chronic fatigue syndrome (ME/CFS).
- In this new case report, scientists report on methods that increased the durability of rTMS in major depressive disorder.
- An uncommon case of urinary retention on a low dose of the antidepressant venlafaxine.
NEW AT CME INSTITUTE
Click to earn free accredited CME credit.
Optimizing Mental Health for Women: Recognizing and Treating Mood Disorders Throughout the Lifespan
Reviewing Non-Dopaminergic Mechanisms for Positive and Negative Schizophrenia Symptom Management