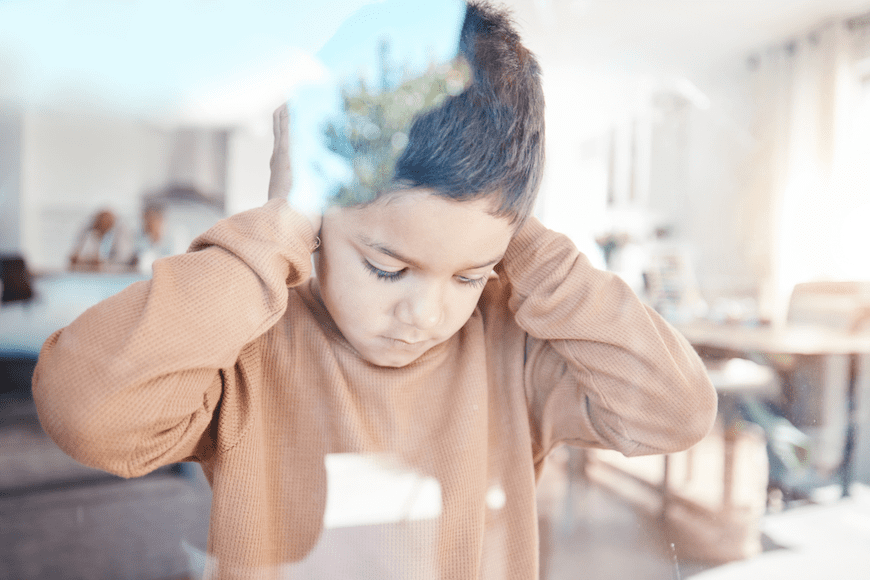
As parents across the country struggle with the challenges of raising a child diagnosed with autism – and as psychiatric professionals fight to help them – it might help to know that the latest CDC data shows that 1 in 36 American children are autistic. That’s up from 1 in 44 just two years ago.
So the timing of a new study from the University of North Carolina School of Medicine’s Department of Psychiatry couldn’t be better.

This latest research, appearing in the Journal of the American Medical Association, discovered that “enlarged perivascular spaces in the brains of babies, caused by an accumulation of excess cerebrospinal fluid, have a 2.2 times greater chance of developing autism later in life.”
Cerebrospinal fluid (CSF) constantly runs through tiny channels around the brain’s blood vessels, known as perivascular spaces. These spaces should be able to purge neurological waste, but disruptions of this process can cause neurological dysfunction, cognitive decline, or developmental delays.
What this research reveals is that infants with particularly enlarged perivascular spaces have a 2.2 times greater chance of developing autism compared to infants with similar genetic risks. This study also suggested that there’s a link between enlarged perivascular spaces in infancy and sleep problems seven to 10 years after diagnosis.
“These results suggest that perivascular spaces could serve as an early marker for autism,” the study’s lead author, Dea Garic, PhD, assistant professor of psychiatry and a member of the Carolina Institute for Developmental Disabilities, wrote.
Starting Young, With an Eye Toward CSF Levels
Garic and her team of researchers looked at infants with a greater chance of developing autism, based on a family member with a similar diagnosis. The researcher tracked these infants before any official autism diagnosis – from 6 months of age to 2 years.
Their study found that 30 percent of infants who later developed autism had enlarged perivascular spaces by 1 year of age. By the time they turned 2, almost half of them diagnosed with autism had enlarged perivascular spaces.
While scientists have studied the role CSF plays in early childhood development for more than a decade, these UNC researchers were the first to uncover the link between too much CSF in infants and a later autism diagnosis. This study reinforced the earlier link between an excessive amount of CSF volume in 6-month-olds and enlarged perivascular spaces at 24 months.
Uncovering an Autism Link To Sleep Problems
Periodically, every six hours or so, the brain purges a wave of CSF from the perivascular spaces to eliminate any potentially harmful neuroinflammatory proteins from building up. This CSF cleansing is more effective while we sleep, based on evidence that most CSF circulation and clearance happens then.
But when something disrupts that sleep, it also disrupts that CSF clearance, as previous animal research has shown.
“Since autism is so highly linked with sleep problems, we were in this unique position to examine CSF dynamics and sleep,” said Garic, who is first author of the paper. “It was really striking to observe such a strong association separated by such a long period of time over childhood. But it really shows how perivascular spaces not only have an effect early in life, but they can have long-term effects, too.”
Methodology
The UNC researchers looked at 870 MRIs from the Infant Brain Imaging Study (IBIS), a national network of researchers investigating brain development, autism, and related developmental disabilities, to measure excessive CSF volume and enlarged perivascular spaces. The researchers pulled MRIs from sleeping infants at 6, 12, and 24 months of age to observe changes over time.
“Our findings were striking, given that neuroradiologists typically view enlarged perivascular spaces as a sign of neurodegeneration in adults, but this study reported it in toddlers,” Garic explained. “This is an important aspect of brain development in the first years of life that should be monitored.”
FURTHER READING
Risk Factors in Autism Spectrum Disorder