Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Psychiatry has utilized lithium to treat affective disorders since the late 1940s; however, roughly 30 years passed before its effect on the thyroid gland was observed. Lithium-induced hypothyroidism is a common consequence of lithium usage, with an estimated prevalence rate between 6% and 52%. However, lithium-induced hyperthyroidism is rare and infrequently reported in the literature, with an incidence of < 0.1%.
To the Editor: Psychiatry has utilized lithium to treat affective disorders since the late 1940s; however, roughly 30 years passed before its effect on the thyroid gland was observed.1 Lithium-induced hypothyroidism is a common consequence of lithium usage,2 with an estimated prevalence rate between 6% and 52%.3 However, lithium-induced hyperthyroidism is rare and infrequently reported in the literature,1,2,4,5 with an incidence of < 0.1%.5,6 Lithium-induced hyperthyroidism usually occurs with long-term treatment and typically presents as a painless and transient thyroiditis, with proposed causality directed toward lithium’s toxic effect on the thyroid or a diffuse, toxic multinodular goiter.1,5,7 Autoimmunity and autoantibody production has also been implicated in the development of lithium-induced hyperthyroidism, which has been demonstrated in 20% of lithium-treated patients compared to 7.5% untreated.5,8
Lithium and antipsychotics are often prescribed concomitantly in clinical practice. While lithium-induced hyperthyroidism is a rare occurrence, antipsychotic-induced akathisia is more prevalent, with a reported incidence rate of up to 30%.9 Akathisia is characterized by an inability to sit still or inner restlessness.10,11 The distress and subjective feelings of akathisia may be mistaken as symptoms of a psychiatric disorder. Frequently, psychosis appears more pronounced during akathisia due to increased agitation.12 Psychiatric manifestations have also been reported in hyperthyroidism including psychosis, emotional lability, and depression.13 Hyperthyroidism and akathisia share symptoms of anxiety, irritability, difficulty concentrating, and psychomotor agitation.13
β-Adrenergic blockers are effective treatments for akathisia and hyperthyroidism.13,14 Treatment of hyperthyroidism with propranolol 60 mg/d or metoprolol tartrate 100 mg/d has been shown to decrease total triiodothyronine (T3) levels by approximately 17.1% and 12.1%, respectively, without altering total thyroxine (T4) levels.15
Case report. Ms A, a 38-year-old woman, was diagnosed with DSM-IV schizoaffective disorder, bipolar type. Medical diagnoses consisted of hypertension and lithium-induced hypothyroidism. Medications included clozapine 400 mg/d, quetiapine 325 mg/d, levothyroxine 50 µg/d, metoprolol succinate 25 mg/d, propranolol 80 mg/d, and lithium 900 mg/d. Her vital signs were stable and monitored daily. No family history of affective disorders or thyroid complications was present.
While residing at our long-term psychiatric facility, Ms A presented with akathisia-like symptoms, worsening psychosis, and a 33-lb weight loss over 8 months despite treatment with clozapine and quetiapine. She reported feeling as if she were “crawling out of her skin” and could not sit still. The treatment team initially thought she was suffering from antipsychotic-induced akathisia. However, there were no medication changes, and, at times, Ms A’s restlessness subsided. Free T4 and thyroid-stimulating hormone (TSH) levels were ordered to rule out hyperthyroidism.
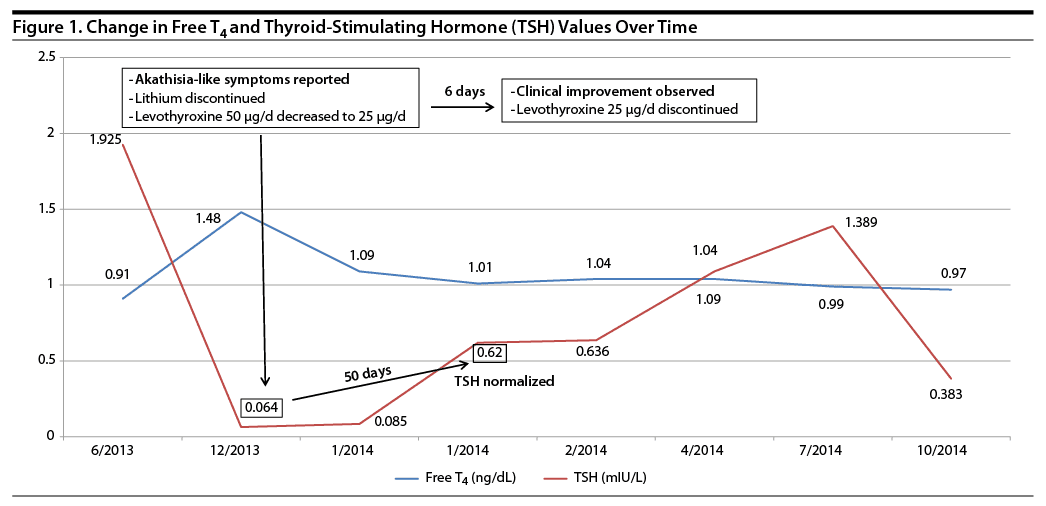
Ms A’s thyroid function tests revealed a free T4 level of 1.48 ng/dL and TSH level of 0.064 mIU/L. Comprehensive metabolic panel and complete blood count results were within normal limits. She was referred to our specialty clinic, and lithium 900 mg/d was discontinued and levothyroxine was decreased to 25 µg/d for 6 days before discontinuation. Her lithium level at the time of discontinuation was 0.8 mEq/L. One month later, free T3, free T4, and thyroid antibodies (TSH receptor antibody, thyroid peroxidase, thyroglobulin) were ordered and found to be within normal range. TSH levels normalized approximately 50 days after her medication changes, while clinical improvement was observed 6 days later (Figure 1). A self-report further confirmed akathisia-like symptoms had abated, and she was “feeling better.”
Lithium-induced hyperthyroidism may require supportive care with β-adrenergic blockers and treatment with antithyroid medications with or without steroids.5 However, Ms A demonstrated improvement shortly after discontinuing lithium and reducing the dose of levothyroxine. β-Adrenergic blockers are known to mask signs of hyperthyroidism, which may have accounted for Ms A’s stable vital signs.
Lithium and antipsychotics are pivotal drugs in the management of mental illness; therefore, health care providers should be aware of the differences and similarities between hyperthyroidism and akathisia when using these medications concomitantly. Conservative management is warranted in patients taking lithium, including regular follow-up assessments and longitudinal laboratories measuring thyroid function.
References
1. Yassa R, Saunders A, Nastase C, et al. Lithium-induced thyroid disorders: a prevalence study. J Clin Psychiatry. 1988;49(1):14-16. PubMed
2. Bandyopadhyay D, Nielsen C. Lithium-induced hyperthyroidism, thyrotoxicosis and mania: a case report. QJM. 2012;105(1):83-85. PubMed doi:10.1093/qjmed/hcq234
3. Kirov G, Tredget J, John R, et al. A cross-sectional and a prospective study of thyroid disorders in lithium-treated patients. J Affect Disord. 2005;87(2-3):313-317. PubMed doi:10.1016/j.jad.2005.03.010
4. Siyam FF, Deshmukh S, Garcia-Touza M. Lithium-associated hyperthyroidism. Hosp Pract (1995). 2013;41(3):101-104. PubMed doi:10.3810/hp.2013.08.1073
5. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 2013;6(1):3. PubMed doi:10.1186/1756-6614-6-3
6. Bocchetta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clin Pract Epidemol Ment Health. 2006;2(2):23. PubMed doi:10.1186/1745-0179-2-23
7. Brownlie BE, Turner JG. Lithium associated thyrotoxicosis. Clin Endocrinol (Oxf). 2011;75(3):402-403. PubMed doi:10.1111/j.1365-2265.2011.04048.x
8. Wilson R, McKillop JH, Crocket GT, et al. The effect of lithium therapy on parameters thought to be involved in the development of autoimmune thyroid disease. Clin Endocrinol (Oxf). 1991;34(5):357-361. PubMed doi:10.1111/j.1365-2265.1991.tb00305.x
9. Janno S, Holi M, Tuisku K, et al. Prevalence of neuroleptic-induced movement disorders in chronic schizophrenia inpatients. Am J Psychiatry. 2004;161(1):160-163. PubMed doi:10.1176/appi.ajp.161.1.160
10. Barnes TR, Braude WM. Akathisia variants and tardive dyskinesia. Arch Gen Psychiatry. 1985;42(9):874-878. PubMed doi:10.1001/archpsyc.1985.01790320042006
11. Bratti IM, Kane JM, Marder SR. Chronic restlessness with antipsychotics. Am J Psychiatry. 2007;164(11):1648-1654. PubMed doi:10.1176/appi.ajp.2007.07071150
12. Iqbal N, Lambert T, Masand P. Akathisia: problem of history or concern of today. CNS Spectr. 2007;12(suppl 14):1-13. PubMed
13. Geracioti TD. Identifying hyperthyroidism’s psychiatric presentations. Current Psychiatry. 2006;5(12):84-92.
14. Zubenko GS, Lipinski JF, Cohen BM, et al. Comparison of metoprolol and propranolol in the treatment of akathisia. Psychiatry Res. 1984;11(2):143-149. PubMed doi:10.1016/0165-1781(84)90098-2
15. Shikara MM, Maniar R, Steier W, et al. The effect of propranolol, atenolol and metoprolol on the serum levels of thyroxin (T4) and triiodothyronine (T3). Proc West Pharmacol Soc. 2003;46:1275.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top