Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Fahr’s disease is a rare neurologic disorder characterized by abnormal calcified deposits in the basal ganglia and cerebral cortex presenting with progressive dementia, psychosis, and dyskinesias. We present an atypical case of Fahr’s disease presenting with primarily neuropsychiatric disease with profound, rapidly progressive psychosis and memory deficits with no focal neurologic deficits that was responsive to haloperidol.
Case report. A 44-year-old Vietnamese man with a history of well-controlled hypertension presented with 2 weeks of acute, progressively worsening memory loss and psychosis.
New-Onset Psychosis and Dementia: An Atypical Case of Fahr’s Disease
To the Editor: Fahr’s disease is a rare neurologic disorder characterized by abnormal calcified deposits in the basal ganglia and cerebral cortex presenting with progressive dementia, psychosis, and dyskinesias. We present an atypical case of Fahr’s disease presenting with primarily neuropsychiatric disease with profound, rapidly progressive psychosis and memory deficits with no focal neurologic deficits that was responsive to haloperidol.
Case report. A 44-year-old Vietnamese man with a history of well-controlled hypertension presented with 2 weeks of acute, progressively worsening memory loss and psychosis. During this time, he experienced loss of semantic and episodic memory with preservation of procedural memory. He exhibited social isolation, disinhibition, irritability, and aggression. He displayed worsening paranoia and developed auditory and visual hallucinations. He was noted to increasingly engage in compulsive repetitive behaviors.
At admission, the patient was alert, yet disoriented. His speech was pressured with prominent latency and echolalia. He was tangential with evident derailment. He exhibited significant psychomotor agitation with echopraxia, bradykinesia, and micrographia. He was actively responding to internal stimuli and describing "demons" in the room. The physical examination was nonfocal. The St Louis University Mental Status examination1 for detecting mild cognitive impairment and dementia was performed, with scores of 10/30 on day 1 and 14/30 on day 2.
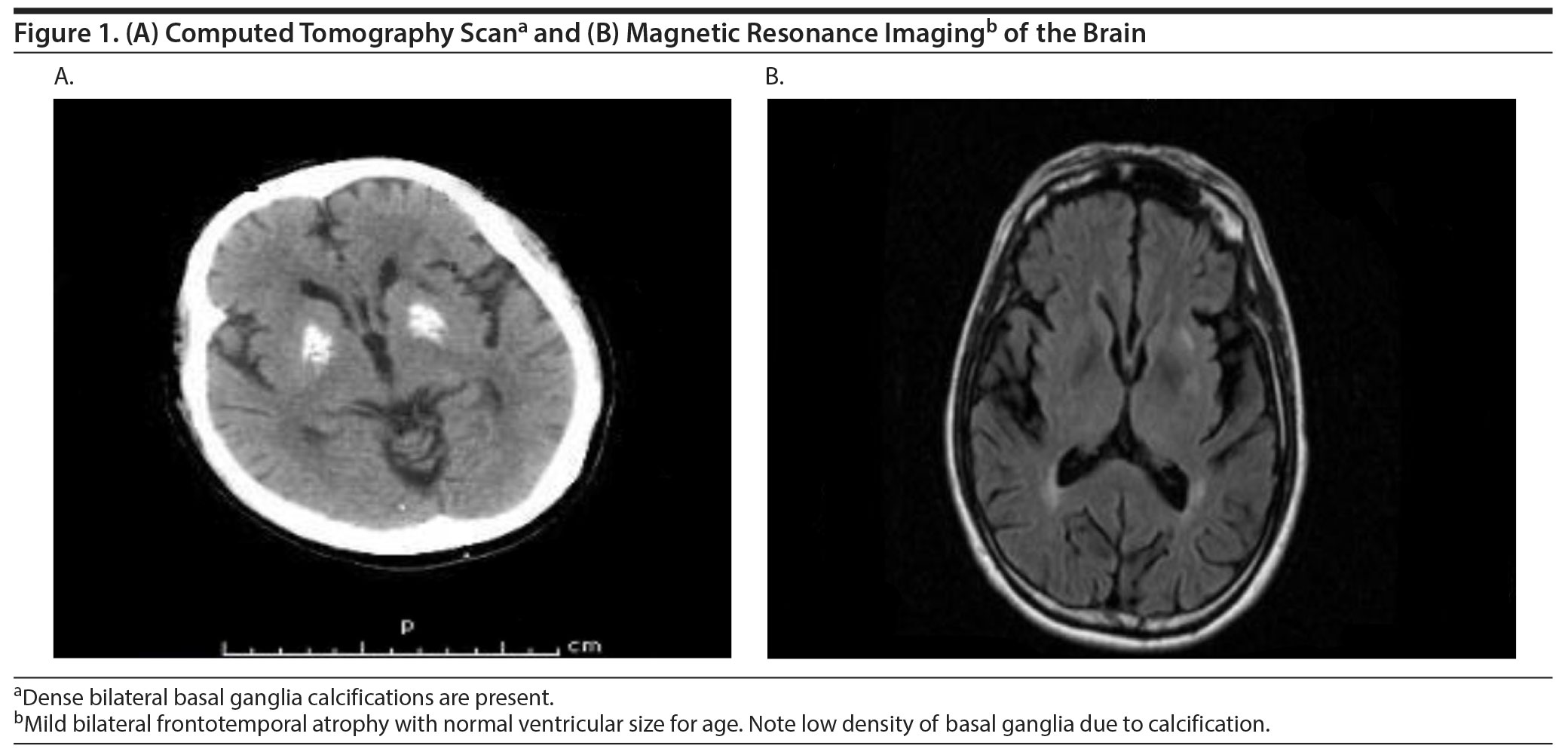
Initial laboratory evaluation included a complete blood count, comprehensive metabolic profile, urine drug screen, urinalysis, and lumbar puncture. The only pertinent positive finding was an elevated creatine kinase-MB level of 976. Screening for Creutzfeldt-Jacob disease, metabolic encephalopathy, and parathyrotoxicosis was negative. Head computed tomography and magnetic resonance imaging were obtained, and the diagnosis of Fahr’s disease (ICD-10 criteria) was confirmed on day 7 of admission (Figure 1). A positron emission tomography scan showed minimal, asymmetric uptake of radiotracer in the medial aspect of the bilateral temporal lobes, with significant reduction of metabolism in the basal ganglia and frontal lobes. Electroencephalography showed diffuse background slowing.
The patient was started on donepezil 5 mg twice daily with no improvement. He was later started on haloperidol 1 mg twice daily to manage worsening agitation and psychosis. The patient was discharged home on day 15 of his admission with scheduled haloperidol and no hallucinations or delusions.
Fahr’s disease is characterized by abnormal deposition of calcium in the basal ganglia, dentate nuclei, putamen, thalami, and cerebellum.2 Onset of disease is insidious and presents in middle age. Neuropsychiatric features include psychosis, mood changes, memory disturbances, impaired executive functioning, inattention, and bradyphrenia.3,4 Diagnosis is based on clinical assessment, imaging, and exclusion of other causes of intracranial calcifications.5
Fahr’s disease can present as either a primary or secondary form due to metabolic or endocrine pathology. Forty percent of patients present initially with psychiatric symptoms.6 Early-onset psychotic symptoms occur at a mean age of 31 years and can present with minimal outward neurologic manifestation.7 Later-onset psychosis, with a mean age of 49 years, exhibits prominent dementia and movement disorder.7 Treatment for Fahr’s disease is supportive. Several agents have been used favorably for psychosis including use of quetiapine,7 risperidone,8 and clozapine.3
In this case, the patient exhibited rapid decompensation and prominent neuropsychiatric manifestations with no focal neurologic deficits. This case is unique given the patient’s age at presentation and highlights the importance of awareness of Fahr’s disease as a differential diagnosis for new-onset psychosis. The case illustrates the importance of early neuroimaging and consideration of organic causes in new-onset psychosis. The patient was responsive to haloperidol, with resolution of psychosis by day 15 of hospitalization. Early awareness and diagnosis of Fahr’s disease, even in cases with a prominent psychiatric manifestation, is critical, as it can aid in preserving function and reducing unneeded evaluation and treatment, while offering better prognostic guidance to the patient and family.
References
1. Tariq SH, Tumosa N. Chibnall JT, et al. Comparison of the Saint Louis University Mental Status examination and the Mini-Mental State Examination for detecting dementia and mild neurocognitive disorder-a pilot study. Am J Geriatr Psychiatry. 2006 Nov;14(11):900-10. doi:10.1097/01.JGP.0000221510.33817.86 PubMed
2. Abubakar SA, Saidu S. Idiopathic bilateral strio-pallido-dentate calcinosis (Fahr’s disease): a case report and review of the literature. Ann Afr Med. 2012;11(4):234-237. PubMed doi:10.4103/1596-3519.102855
3. El Hechmi S, Bouhlel S, Melki W, et al. Psychotic disorder induced by Fahr’s syndrome: a case report. Encephale. 2014;40(3):271-275. PubMed doi:10.1016/j.encep.2013.04.012
4. Ring HA, Serra-Mestres J. Neuropsychiatry of the basal ganglia. J Neurol Neurosurg Psychiatry. 2002;72(1):12-21. PubMed doi:10.1136/jnnp.72.1.12
5. Lam JS, Fong SY, Yiu GC, et al. Fahr’s disease: a differential diagnosis of frontal lobe syndrome. Hong Kong Med J. 2007;13(1):75-77. PubMed
6. König P. Psychopathological alterations in cases of symmetrical basal ganglia sclerosis. Biol Psychiatry. 1989;25(4):459-468. PubMed doi:10.1016/0006-3223(89)90199-6
7. Cummings JL, Gosenfeld LF, Houlihan JP, et al. Neuropsychiatric disturbances associated with idiopathic calcification of the basal ganglia. Biol Psychiatry. 1983;18(5):591-601. PubMed
8. Kumar S, Sher K, et al. Fahr’s disease: a rare neurological disease frequently misdiagnosed as acute psychosis, or mood disorder. J Neurol Disord. 2013;1:130. http://dx.doi.org/10.4172/2329-6895.1000130
9. Faye AD, Gawande S, Tadke R, et al. A case of psychosis due to Fahr’s syndrome and response to behavioral disturbances with risperidone and oxcarbazepine. Indian J Psychiatry. 2014;56(2):188-190. PubMed doi:10.4103/0019-5545.130506
aDepartment of Psychiatry, University of Michigan Hospital System, Ann Arbor
bDepartment of Pediatrics, University of Michigan Hospital System, Ann Arbor
cDepartment of Neurology, Indiana University School of Medicine, Indianapolis
Potential conflicts of interest: None.
Funding/support: None.
Published online: September 29, 2016.
Prim Care Companion CNS Disord 2016;18(5):doi:10.4088/PCC.15l01915
© Copyright 2016 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top