Prim Care Companion CNS Disord 2023;25(1):22cr03256
To cite: Uvais NA, Sreeraj VS, Moideen S, et al. Central nervous system lymphoma presenting as psychogenic vomiting. Prim Care Companion CNS Disord. 2023;25(1):22cr03256.
To share: https://doi.org/10.4088/PCC.22cr03256
© 2023 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry, Iqraa International Hospital and Research Centre, Calicut, India
bDepartment of Psychiatry, National Institute of Mental Health and Neurosciences, Bangalore, Karnataka, India
cDepartment of Internal Medicine, Iqraa International Hospital and Research Centre, Calicut, Kerala, India
dDepartment of Radiology, Iqraa International Hospital and Research Centre, Calicut, India
*Corresponding author: N. A. Uvais, MBBS, DPM, Department of Psychiatry, Iqraa International Hospital and Research Centre, Calicut, India ([email protected]).
Psychogenic vomiting refers to persistent or recurrent vomiting in the absence of any obvious organic cause and resulting from a psychological mechanism. A diagnosis of psychogenic vomiting is made within the overall biopsychosocial context, with emotional changes and psychological stressors often triggering the symptom production.1,2 Self-induced vomiting presents in many psychiatric conditions such as eating disorders, but spontaneous psychogenic vomiting is an uncommon presentation that is disabling.3 Hypokalemia and dehydration due to psychogenic vomiting most often necessitates detailed evaluation with hospitalization. A retrospective study4 from Portugal revealed that 3–12 per million of the general population required hospitalization annually for psychogenic vomiting, and it is predominant among females (74%).
Generally, psychogenic vomiting does not respond to standard antiemetic agents and requires antianxiety/antidepressant treatments in the form of pharmacologic or psychosocial interventions.5 In a case series by Muraoka et al,6 most of the patients did not have vomiting solely due to emotional conflict but had it in combination with past organic or gastrointestinal function abnormalities. Thus, vomiting presenting in the context of psychosocial stressors is most often due to modulation of an abnormal brain-gut axis and in the absence of a history could be an early manifestation of a medical illness. Here, we describe a case of central nervous system lymphoma presenting as psychogenic vomiting in a young woman.
Case Report
A 22-year-old married mother of a 3-year-old child with a husband working in the Gulf presented to the emergency department with a 2-week history of recurrent vomiting. The vomiting was episodic and severe, not associated with nausea, recurring every half to 1 hour. The vomitus consisted of ingested food particles when it happened immediately after eating. There was no history of fever, abdominal pain, or loose stools. There was no response to standard central and peripherally acting antiemetic agents. A detailed medical and neurologic evaluation revealed no organic causes. The routine blood investigations were within normal limits. She also reported worries regarding her symptoms and impaired appetite and sleep for 1 week duration. She was referred to the psychiatric department to rule out psychological causes for the vomiting.
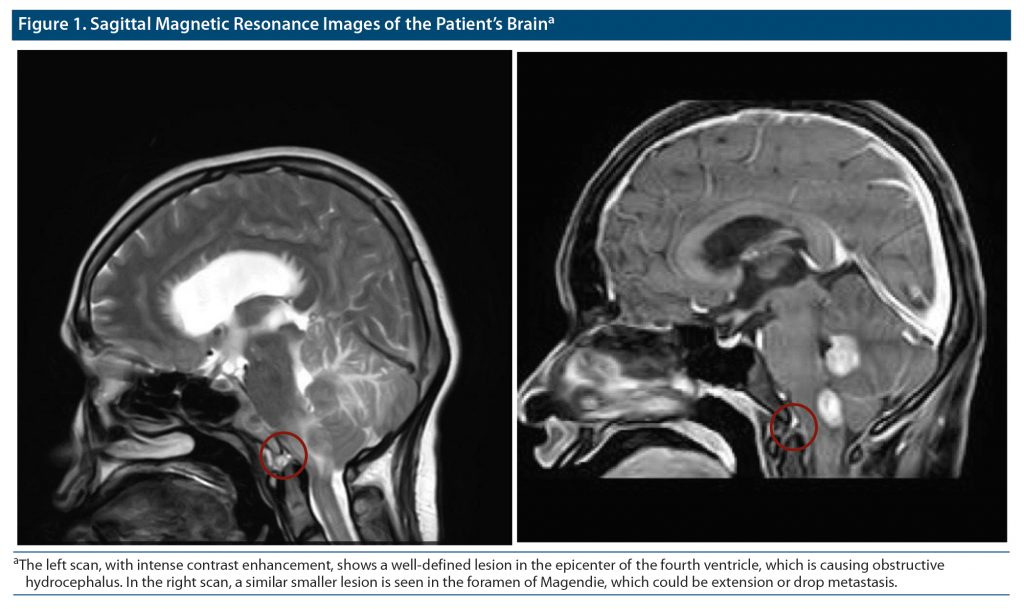
During the psychiatric interview, she reported significant stress related to her relationship with her in laws. There was also a history of conversion disorder during childhood. Her mental status examination showed anxious affect. Considering absence of medical causes, significant ongoing stress, and history of conversion disorder during childhood, a provisional diagnosis of conversion disorder (psychogenic vomiting) was made, and she was started on oral clonazepam 0.375 mg/d. Her condition significantly improved, and she started eating normally within 2 days and was discharged. She was readmitted to the hospital with recurrent vomiting within 2 weeks while on clonazepam, and a magnetic resonance imaging brain scan was conducted to rule out any organic causes, which revealed lymphoma near the fourth ventricle of the brain (Figure 1). She was referred to another center for further treatment.
Discussion
This case describes a patient with lymphoma near the fourth ventricle of the brain presenting with psychogenic vomiting. Persistent vomiting was noted in the context of conflict within the family, which responded to a benzodiazepine due to relief of her anxiety but not to the standard central and peripherally acting antiemetic agents. The pattern of vomiting was similar to that of patients described by Muraoka et al,6 which was always related to anxiety and conversion. The other 4 types include habitual post-prandial, irregular (often seen with depressive disorders), nausea, and self-induced vomiting (seen with eating disorders).
The vomiting center lies in the medulla oblongata, comprising nucleus tractus solitaries and reticular formation. On activation of this center, motor efferent pathways passing through cranial and sympathetic nerves to the diaphragmatic and abdominal muscles trigger vomiting. The vomiting center is activated through 4 primary sources: chemoreceptor trigger zone, vestibular region, gastrointestinal tract, and cerebral cortex.7 Pain and anxiety mediated by γ-aminobutyric acid and glutamatergic neurons are known to influence the vomiting center, leading to psychogenic vomiting. Benzodiazepines, by enhancing the inhibitory systems, can reduce anxiety and thus the vomiting caused by it.
This mechanism is relevant in acute intense pain and anxiety. In chronic anxiety states, this process might not be active unless an additive factor that could activate the vomiting center is present. The lymphoma positioned around the fourth ventricle in the current patient might have reduced the threshold for vomiting. Direct pressure effect by the mass proximal to the vomiting center, involvement of certain neurons of the vomiting center in the tumor, or immunologic or inflammatory mediators released from the mass could have been additional factors that would have reduced the threshold for vomiting. Anxiety in the context of interpersonal issues within the family triggered intractable vomiting, which decreased with a single dose of a benzodiazepine.
A comparative study2 showed that most patients with psychogenic vomiting had gastric dysmotility and hypersensitivity, which had increased biological propensity to develop vomiting in the background of psychosocial factors. Few clinicians observe psychogenic vomiting as a diagnosis of exclusion and consider its diagnosis in the presence of another contributory medical condition an erroneous decision.8 Psychogenic vomiting should not be considered only after excluding organicity. Everyone has a threshold to experience vomiting due to psychological stressors. The manifestation of vomiting related to a stressor could increase the severity of the stressor or reduce the threshold due to increased gastric motility secondary to central or peripheral causes. Thus, comprehensive management of psychogenic vomiting should follow identification of the psychological stressor and the underlying factors changing the threshold for vomiting and should target both the psychological and biological factors triggering the gastric expulsion.
Published online: February 2, 2023.
Relevant financial relationships: None.
Funding/support: None.
Patient consent: Consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
References (8)

- Hederos CA. Psychogenic vomiting. Lancet. 1992;339(8803):1228. PubMed CrossRef
- Zhao Y, Ke M, Wang Z, et al. Pathophysiological and psychosocial study in patients with functional vomiting. J Neurogastroenterol Motil. 2010;16(3):274–280. PubMed CrossRef
- Olden KW, Crowell MD. Chronic nausea and vomiting: new insights and approach to treatment. Curr Treat Options Gastroenterol. 2005;8(4):305–310. PubMed CrossRef
- Cruz AM, Gonçalves-Pinho M, Santos JV, et al. Eating disorders-related hospitalizations in Portugal: a nationwide study from 2000 to 2014. Int J Eat Disord. 2018;51(10):1201–1206. PubMed CrossRef
- Pooja V, Gupta N, Khan A, et al. Psychogenic vomiting: a case series. Ind Psychiatry J. 2021;30(suppl 1):S252–S254. PubMed
- Muraoka M, Mine K, Matsumoto K, et al. Psychogenic vomiting: the relation between patterns of vomiting and psychiatric diagnoses. Gut. 1990;31(5):526–528. PubMed CrossRef
- Becker DE. Nausea, vomiting, and hiccups: a review of mechanisms and treatment. Anesth Prog. 2010;57(4):150–156, quiz 157. PubMed CrossRef
- Koyama A, Ohtake Y, Yasuda K, et al. Avoiding diagnostic errors in psychosomatic medicine: a case series study. Biopsychosoc Med. 2018;12(1):4. PubMed CrossRef
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top