Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: The cerebellum is the center for control of voluntary movements and coordination, thereby playing a pivotal role in maintenance of posture, balance, gait, and speech. However, research reveals a wider role additionally involving control of cognitive functions, emotion, and behavior due to widespread cerebellar connections to the cortex and association areas.
Recent reports reveal that patients with cerebellar disease develop mood changes and cognitive decline, and a strong association has been reported between the structural and functional abnormalities of the cerebellum and psychiatric disorders like schizophrenia, bipolar disorder, depression, anxiety, attention-deficit/hyperactivity disorder, and autism.
Cerebellar Cognitive Affective Syndrome: A Case Report
To the Editor. The cerebellum is the center for control of voluntary movements and coordination, thereby playing a pivotal role in maintenance of posture, balance, gait, and speech. However, research reveals a wider role additionally involving control of cognitive functions, emotion, and behavior due to widespread cerebellar connections to the cortex and association areas.1-3
Recent reports4 reveal that patients with cerebellar disease develop mood changes and cognitive decline, and a strong association has been reported between the structural and functional abnormalities of the cerebellum and psychiatric disorders like schizophrenia, bipolar disorder, depression, anxiety, attention-deficit/hyperactivity disorder, and autism. Cerebellar cognitive affective syndrome is a rare entity observed in patients with focal cerebellar lesions characterized by disturbances of executive function, impaired spatial cognition, impaired visual-spatial memory, personality change, and linguistic difficulties.5
Case report. A 60-year-old man presented to the psychiatry outpatient services with a history of persistent and pervasive low mood and disturbed sleep and appetite for the past 2 months following an episode of high-grade fever with loose stools and vomiting for which he was admitted for 2 days and diagnosed with acute gastroenteritis. Nearly a week later, the patient’s family members noticed that he was unusually quiet, would not interact with anyone, and stopped going to work. He also had difficulty walking and speaking. He would often sway and needed support while walking. There was no history of alcohol or drug use except for smoking for the past 20 years. There was no significant past or family history of any medical illness.
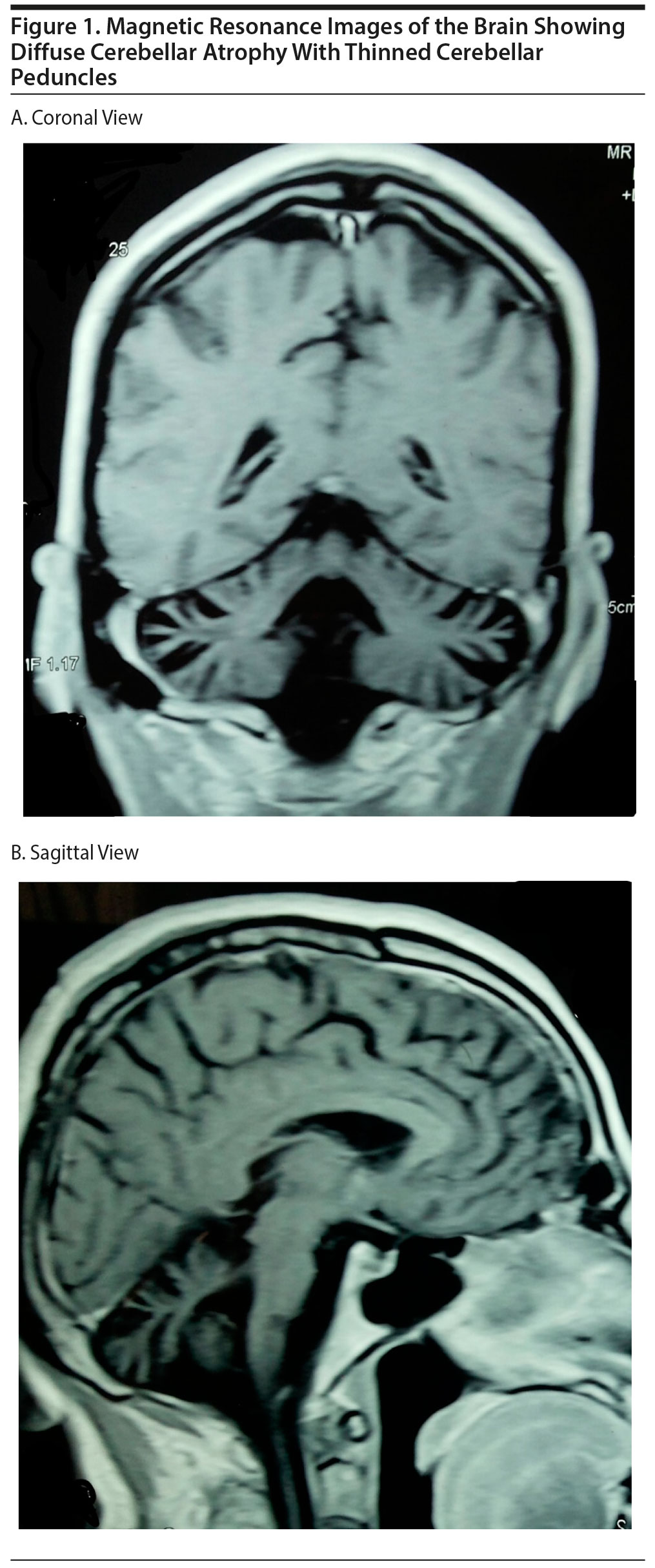
A general physical and central nervous system examination revealed a conscious, cooperative elderly man with ataxic gait, dysarthric speech, and impaired tandem walking. However, other tests for coordination (finger-to-nose test, heel-shin test, dysdiadochokinesia) were normal. Sensory and motor systems and cranial nerves were intact. A mental state examination revealed poor eye contact, reduced psychomotor activity and speech, depressed affect, hopelessness, and wishes to die. Higher mental functions revealed impaired attention and concentration (digit span test, serial subtraction test) and poor immediate and recent memory with intact judgment and insight. Results of routine blood investigations, thyroid function tests, vitamin B12 levels, and electroencephalograph were within normal limits. The patient was nonreactive for HIV and hepatitis B and C. Magnetic resonance brain imaging showed diffuse cerebellar atrophy with thinned-out cerebellar peduncles (Figure 1A and B). Cerebellar cognitive affective syndrome was suspected (diagnosed based on symptom cluster as per references 1-5). He was started on fluoxetine 20 mg/d, which was increased to 40 mg/d after a week, and he reported improvement at 4-week follow-up.
Cerebellar cognitive affective syndrome was conceptualized by Schmahmann and Sherman1,5 while observing patients with cerebellar damage. They found that behavioral changes were clinically prominent in patients with disease of the posterior lobe of the cerebellum and the vermis.1,5 There can be a number of causes for cerebellar damage such as viral infections and drugs, but no specific etiology could be detected in our patient, who most likely was a sporadic case of cerebellar degeneration.1
References
1. Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16(3):367-378. PubMed doi:10.1176/jnp.16.3.367
2. Hokkanen LS, Kauranen V, Roine RO, et al. Subtle cognitive deficits after cerebellar infarcts. Eur J Neurol. 2006;13(2):161-170. PubMed doi:10.1111/j.1468-1331.2006.01157.x
3. Timmann D, Dimitrova A, Hein-Kropp C, et al. Cerebellar agenesis: clinical, neuropsychological and MR findings. Neurocase. 2003;9(5):402-413. PubMed doi:10.1076/neur.9.5.402.16555
4. Phillips JR, Hewedi DH, Eissa AM, et al. The cerebellum and psychiatric disorders. Front Public Health. 2015;3:66. PubMed doi:10.3389/fpubh.2015.00066
5. Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121(pt 4):561-579. PubMed doi:10.1093/brain/121.4.561
aDepartment of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India
Potential conflicts of interest: None reported.
Funding/support: None reported.
Published online: March 31, 2016.
Prim Care Companion CNS Disord 2016;18(2):doi:10.4088/PCC.15l01851
© Copyright 2016 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top