Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Cerebral venous thrombosis (CVT) is a rare type of stroke, with an annual incidence of around 1/100,000. Signs and symptoms are those associated with increased intracranial pressure due to impaired venous drainage and focal neurologic deficits resulting from venous ischemia or hemorrhage. The first group of symptoms includes headache (the most common symptom and present in around 90% of patients) and papilledema.
Cerebral Venous Thrombosis Following Strangulation
To the Editor: Cerebral venous thrombosis (CVT) is a rare type of stroke, with an annual incidence of around 1/100,000.1 Signs and symptoms are those associated with increased intracranial pressure due to impaired venous drainage and focal neurologic deficits resulting from venous ischemia or hemorrhage.2,3 The first group of symptoms includes headache (the most common symptom and present in around 90% of patients4) and papilledema. Possible focal neurologic signs of CVT include hemiparesis and aphasia. Epileptic seizures are also a common symptom of CVT, occurring in around 40% of patients.5
CVT is associated with a diverse range of etiologic factors. These factors include prothrombotic conditions like Factor V Leiden mutation, pregnancy, use of oral contraception, cancer, parameningeal infections (eg, sinusitis), and dehydration among others.3,4 Although venous stasis following strangulation has been hypothetically proposed as a possible cause of CVT, there has been no report to date of a patient in whom CVT occurred after strangulation.
Case report. A 75-year-old man was transferred to the psychiatric emergency department after an attempt to strangle himself with a belt. The patient suffered from previously uncharacterized dementia and depressive symptoms. His medical history included pulmonary embolism several years ago, atrial fibrillation, and chronic renal failure. His family history was unremarkable.
The patient had been treated for atrial fibrillation with enoxaparin subcutaneously in a dose adjusted to the renal function (70 mg/d). Anticoagulant treatment with rivaroxaban had been recently replaced with enoxaparin due to renal failure.
The patient’s physical examination was remarkable for a strangulation mark on the left side of the neck. Neurologic examination revealed impaired cognitive function but no new neurologic deficit. The Mini-Mental Status Examination (MMSE)6 revealed a score of 14/30. Preexisting neurologic symptoms included dysarthria, mild facial asymmetry, and reduced coordination.
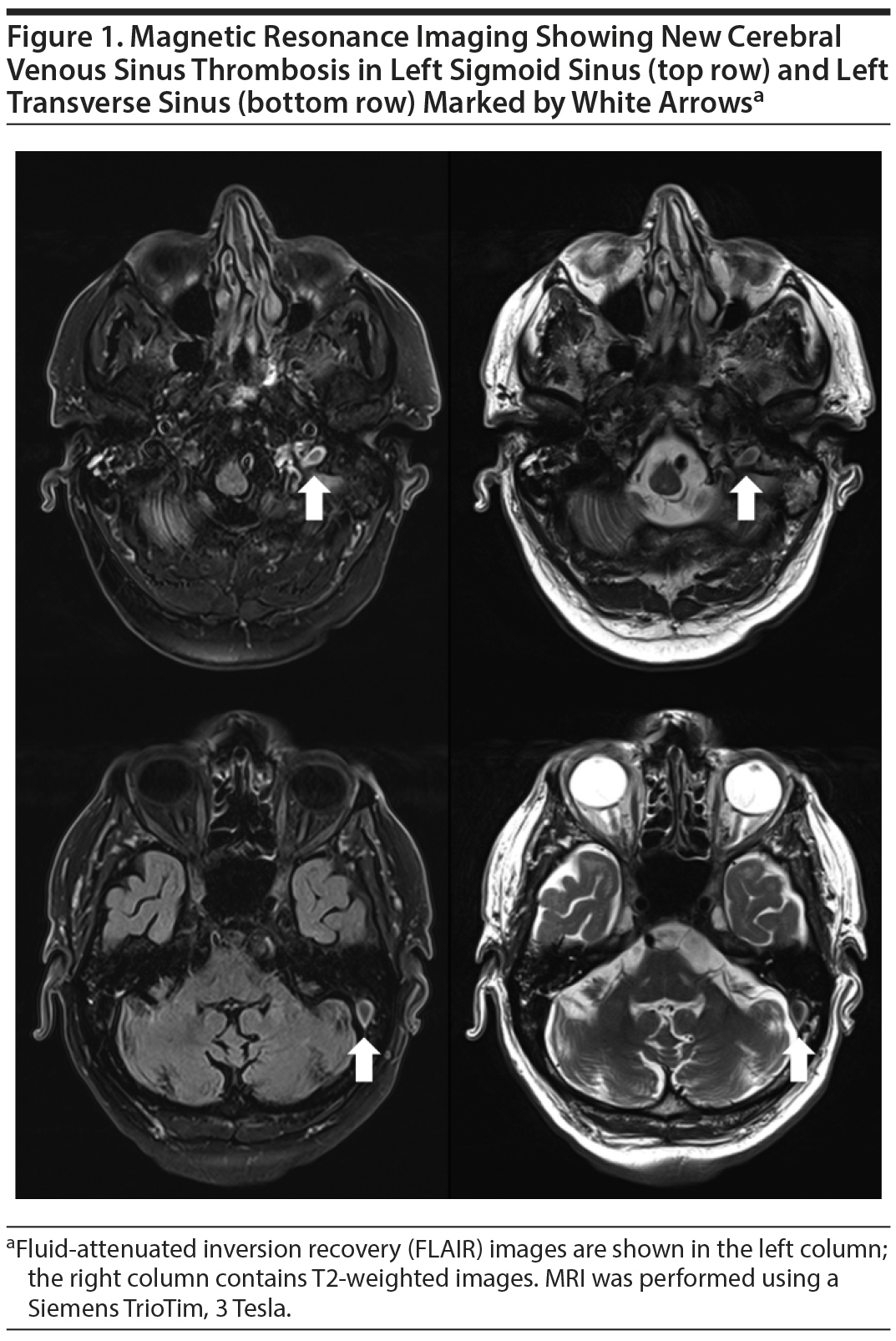
Laboratory workup confirmed renal failure (glomerular filtration rate 21 mL/min/1.73 m2). Duplex ultrasound provided no evidence of carotid dissection. Electroencephalogram results showed diffuse slowing. Two days later, cranial magnetic resonance imaging (MRI; Siemens TrioTim, 3 Tesla) for workup of dementia showed severe cerebral microangiopathy (Fazekas score of 3) indicating vascular dementia. As an incidental, unexpected finding, the MRI revealed a fresh thrombosis in the left transverse and sigmoid sinuses (Figure 1) without hemorrhage or edema in the adjacent brain tissue. A clinical and laboratory workup for causes of thrombosis was remarkable only for hyperhomocysteinemia (30.7 µmol/L; normal range, < 9 µmol/L).
The patient’s anticoagulant treatment was switched to oral phenprocoumon. Eventually, the patient was transferred back to the nursing home after remission of depression.
Venous stasis due to compression of the jugular vein is the most plausible cause of CVT in our patient, while potentially predisposing factors were hyperhomocysteinemia2-4 and recent change of the anticoagulant regimen.
Case reports have suggested that CVT may result from stasis due to venous dilation: decreased intracranial pressure (due to spontaneous intracranial hypotension7-9 or lumbar puncture10) may lead to dilation of cerebral veins and thus reduced blood flow velocity, contributing to the risk of CVT. Mechanical obstruction of venous drainage will also contribute to stasis and is a plausible etiologic factor. However, the evidence for this relationship is limited. In a large study4 of CVT, jugular catheter occlusion was reported in 0.8% of patients, and case reports11,12 have found CVT secondary to internal jugular vein thrombosis in the presence or absence of a central venous catheter.
The incidence of CVT after strangulation may be broadly underestimated especially in older patients, since clinical presentation may be atypical, with altered mental status as the prominent symptom.13 This case report demonstrates that CVT should be included in the differential diagnosis in patients who develop otherwise unexplained neurologic or neuropsychological symptoms after strangulation.
References
1. Coutinho JM, Zuurbier SM, Aramideh M, et al. The incidence of cerebral venous thrombosis: a cross-sectional study. Stroke. 2012;43(12):3375-3377. PubMed CrossRef
2. Piazza G. Cerebral venous thrombosis. Circulation. 2012;125(13):1704-1709. PubMed CrossRef
3. Saposnik G, Barinagarrementeria F, Brown RD Jr, et al; American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158-1192. PubMed CrossRef
4. Ferro JM, Canh×£o P, Stam J, et al; ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004;35(3):664-670. PubMed CrossRef
5. Ferro JM, Canh×£o P, Bousser MG, et al; ISCVT Investigators. Early seizures in cerebral vein and dural sinus thrombosis: risk factors and role of antiepileptics. Stroke. 2008;39(4):1152-1158. PubMed CrossRef
6. Folstein MF, Folstein SE, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. PubMed CrossRef
7. Haritanti A, Karacostas D, Drevelengas A, et al. Spontaneous intracranial hypotension: clinical and neuroimaging findings in six cases with literature review. Eur J Radiol. 2009;69(2):253-259. PubMed CrossRef
8. Garcia-Carreira MC, Vergé DC, Branera J, et al. Cerebral venous thrombosis in two patients with spontaneous intracranial hypotension. Case Rep Neurol Med. 2014;2014:528268. PubMed CrossRef
9. Lan MY, Chang YY, Liu JS. Delayed cerebral venous thrombosis in a patient with spontaneous intracranial hypotension. Cephalalgia. 2007;27(10):1176-1178. PubMed CrossRef
10. Wilder-Smith E, Kothbauer-Margreiter I, Lämmle B, et al. Dural puncture and activated protein C resistance: risk factors for cerebral venous sinus thrombosis. J Neurol Neurosurg Psychiatry. 1997;63(3):351-356. PubMed CrossRef
11. Binnani P, Bahadur MM, Dalal K. Dural sinus thrombosis: a rare manifestation of internal jugular venous occlusion. Saudi J Kidney Dis Transpl. 2012;23(4):799-803. PubMed CrossRef
12. Tamizifar B, Beigi A, Rismankarzadeh M. Venous thrombosis in subclavian, axillary, brachial veins with extension to internal jugular vein, right sigmoid sinus and simultaneous pulmonary embolism. J Res Med Sci. 2013;18(1):77-79. PubMed
13. Ferro JM, Canh×£o P, Bousser MG, et al; ISCVT Investigators. Cerebral vein and dural sinus thrombosis in elderly patients. Stroke. 2005;36(9):1927-1932. PubMed CrossRef
aDepartment of Psychiatry and Psychotherapy, Central Institute of Mental Health, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany
bDepartment of Neuroradiology, University Medical Center Mannheim, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany
Potential conflicts of interest: None.
Funding/support: None.
Additional information: Information has been de-identified to protect anonymity.
Published online: June 21, 2018.
Prim Care Companion CNS Disord 2018;20(3):17l02198
To cite: Clemm von Hohenberg C, Kerl U, Sartorius A, et al. Cerebral venous thrombosis following strangulation. Prim Care Companion CNS Disord. 2018;20(3):17l02198.
To share: https://doi.org/10.4088/PCC.17l02198
© Copyright 2018 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top