Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
Have you ever assumed that a patient who is crying has depression? Have you ever considered that nonpsychiatric causes of crying may be present? Have you ever wondered if more specific interventions might be applied on the basis of the etiology of crying?
Differential Diagnosis and Management Strategies

LESSONS LEARNED AT THE INTERFACE OF MEDICINE AND PSYCHIATRY
The Psychiatric Consultation Service at Massachusetts General Hospital (MGH) sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Dr Lokko is a postgraduate year 4 resident, an administrative chief resident at the Massachusetts General Hospital/McLean Hospital Adult Psychiatry Residency Training Program, and a clinical fellow at Harvard Medical School, Boston, Massachusetts. Dr Stern is chief of the Avery D. Weisman Psychiatry Consultation Service at Massachusetts General Hospital and the Ned H. Cassem professor of psychiatry in the field of psychosomatic medicine/consultation at Harvard Medical School, Boston, Massachusetts.
Prim Care Companion CNS Disord 2016;18(4):doi:10.4088/PCC.16f01956
© Copyright 2016 Physicians Postgraduate Press, Inc.
Submitted: April 4, 2016; accepted May 20, 2016.
Published online: July 21, 2016.
Potential conflicts of interest: Dr Stern is an employee of the Academy of Psychosomatic Medicine, has served on the speaker’s board of Reed Elsevier, is a stock shareholder in WiFiMD (Tablet PC), and has received royalties from Mosby/Elsevier and the Massachusetts General Hospital Psychiatry Academy and McGraw Hill. Dr Lokko reports no financial or other affiliation relevant to the subject of this article.
Funding/support: None.
Corresponding author: Hermioni N. Lokko, MD, MPP, Department of Psychiatry, Massachusetts General Hospital/McLean Hospital, 15 Parkman St, Wang ACC-812, Boston, MA 02114 ([email protected]).
Have you ever assumed that a patient who is crying has depression? Have you ever considered that nonpsychiatric causes of crying may be present? Have you ever wondered if more specific interventions might be applied on the basis of the etiology of crying? If you have, then the case vignettes and discussion presented here should prove useful.
Crying is recognized around the world as a uniquely human expression and as a sign of vulnerability and distress.1,2 Crying is labeled as weeping, bawling, sobbing, wailing, blubbering, howling, keening, yowling, shedding tears, or sniveling; the term used is often determined by one’s culture.3 Crying occurs in response to both negative and positive emotions.2,4 Crying can also be regarded as an attachment behavior that elicits caregiving responses from others.2
Crying serves both intraindividual and interindividual functions.4 Intraindividual functions of crying facilitate self-soothing in the person who cries as well as relief from stress.4 Interindividual functions of crying evoke empathy and protective responses from others, which facilitate social bonding and reduce aggression among individuals.4 Crying also communicates one’s emotional level to others (eg, distress, pain, need for support).2
Despite limited data on crying’s impact on clinicians, few would dispute that intense affect experienced by clinicians who observe a patient crying can impact decision-making.5,6 In general hospitals, health care providers often respond with immediate expressions of empathy when they witness a patient crying.7 However, crying may indicate more than distress; it may herald a more complex clinical presentation.8
We present 3 case vignettes in which consultation was requested to evaluate a patient who was crying. We will use these case vignettes to highlight and discuss the prevalence of crying and the evolutionary benefits and physiologic components of crying and to review how clinicians react to tearful patients. We also will discuss the differential diagnosis of crying and formulate management strategies for those who cry.
CASE 1
Mr A, a previously healthy 23-year-old man, presented to the emergency department after sustaining an unintentional gunshot wound to his head (with no trauma to the brain). Postoperatively, psychiatric consultation was requested to complete a safety assessment and to evaluate for depression, since his course was characterized by persistent tearfulness. During the psychiatric evaluation, Mr A reported that collecting and shooting guns was a hobby of his and that his gunshot wound was accidental. Although he endorsed feeling depressed in the setting of postoperative pain, he denied having other neurovegetative symptoms of depression (eg, there were no thoughts of suicide or homicide). His mental status examination revealed a pleasant young man lying in bed with gauze wrapped around his head; he displayed a full range of affect. He felt demoralized but did not meet DSM-5 criteria for a depressive disorder.9 Further evaluation by the medical and surgical teams led to suspicion of epiphora (watery eyes caused by inadequate draining of tears by tear ducts) secondary to his head trauma and surgical repair. Surgical drainage of Mr A’s tear ducts corrected his persistent tearfulness.

- Crying is prevalent in the general hospital and should not be dismissed since the potential etiologies include serious medical, neurologic, and psychiatric conditions.
- Despite the limited data on the best practices to manage crying in hospitalized patients, empathic expressions, as well as pharmacologic and nonpharmacologic management, can provide relief to patients.
Case 1 Discussion
Mr A’s tearfulness and crying could have been explained by several factors, including depression, demoralization, or negative emotions (eg, anxiety, fear, anger, helplessness, pain). However, psychiatric evaluation revealed a medical and surgical etiology for his excessive tearing. Creation of a broad differential diagnosis and an appreciation of the physiologic components of crying were essential for making an accurate diagnosis and for management of his symptoms.
HOW OFTEN DO PATIENTS CRY IN THE GENERAL HOSPITAL?
In an 18-month prospective study of all patients referred to a psychiatric consultation service, Green et al8 found that crying is a common reason (about 17% of their referrals) for psychiatric consultation in medical and surgical inpatients. However, neurologic disorders (especially those with structural or metabolic dysfunction of the central nervous system) are at least as likely to cause crying as are psychiatric disorders.8 A 1-day study10 of all adult inpatients on medical-surgical floors (not just those for whom a psychiatric consultation was requested, N = 650) revealed that 25% had cried in the 24 hours before the assessment was conducted. Remarkably, few patients informed staff of their emotional state or their crying.10
WHAT ARE THE EVOLUTIONARY BENEFITS AND PHYSIOLOGIC COMPONENTS OF CRYING?
Crying has persisted in our species because of its survival benefits, which include lubricating the surface of the eye and helping to wash particulate matter (eg, dust) out of the eyes.11,12 Although many animals cry, crying as a form of emotional expression is unique to humans who cry for myriad reasons ranging from the mundane (eg, celebration of a sports victory) to the significant (eg, the birth of a child or the death of a loved one).13
Tears have been categorized into 3 types: basal tears, reflex tears, and emotional tears. Basal or continuous tears routinely cover the surface of the cornea and facilitate lubrication, nourishment, and protection. With no direct blood supply to the cornea, basal tears are an essential source of oxygen for the eye. Reflex tears are similar to basal tears except that they are produced in response to local irritation (eg, from foreign particles such as dust, wind, or smoke) surrounding the eye (including the cornea, conjunctiva, or nasal mucosa). A hot or bright light shone on the tongue or mouth, as well as vomiting, yawning, or coughing, can also produce reflex tears. The immediate increase in the amount of basal tears causes the eye to water, which washes out irritants that come in contact with the eye.
Emotional tears (ie, induced by grief, pain, anger, or happiness) are typically accompanied by an altered breathing pattern and characteristic facial expressions. Emotional tears tend to contain more protein than do basal or reflex tears, and they can contain hormones (eg, prolactin, adrenocorticotropic hormone, leucine) since the autonomic nervous system has been triggered. Although the literature on the neuronal circuits that mediate crying is meager, it has been established that the limbic cortex and the midline thalamic structures are involved with crying.14 The release of neuroendocrine hormones and serotonin is sometimes associated with the stress-relieving nature of tear production. The lacrimal glands produce tears when they are stimulated by the nicotinic and muscarinic receptors of the autonomic nervous system.
Crying is a complex secretomotor phenomenon that involves the shedding of tears from the lacrimal apparatus, with no irritation of the ocular structures; it is often accompanied by contractions of the muscles of facial expression and by vocalization.4 The lacrimal apparatus consists of the lacrimal gland, the superior and inferior lacrimal punctums, the lacrimal sac, the nasolacrimal duct, the inferior meatus, and turbinate. The lacrimal gland, which produces tears, is located in the upper, outer corner of the eye, and its excretory ducts branch downward toward the eyeball. The front of the eye is washed by a constant stream of tears, which drains through 2 small openings (lacrimal puncta) in the inner corner of the eye to the lacrimal canaliculi. Tears flow from the lacrimal canaliculi into the lacrimal sac and then into the nasolacrimal duct and the nasal cavity. Any eye injury or inflammation caused by trauma, irritants, or allergies, as well as blockages in the lacrimal apparatus can cause excessive tearing or epiphora.
WHAT IS THE DIFFERENTIAL DIAGNOSIS FOR CRYING?
Since patients cry for a variety of reasons, a differential diagnosis for crying should be created. Apart from having intense emotions, patients can react to primary general medical conditions, allergic reactions, and pain with tears. As seen in the case of Mr A, diseases specific to the eye (such as occlusion of the tear ducts or eye infections) can cause epiphora. Several psychiatric disorders, especially those with affective components (eg, sadness, anxiety), can also cause crying. Crying can also be observed as part of normal grieving.
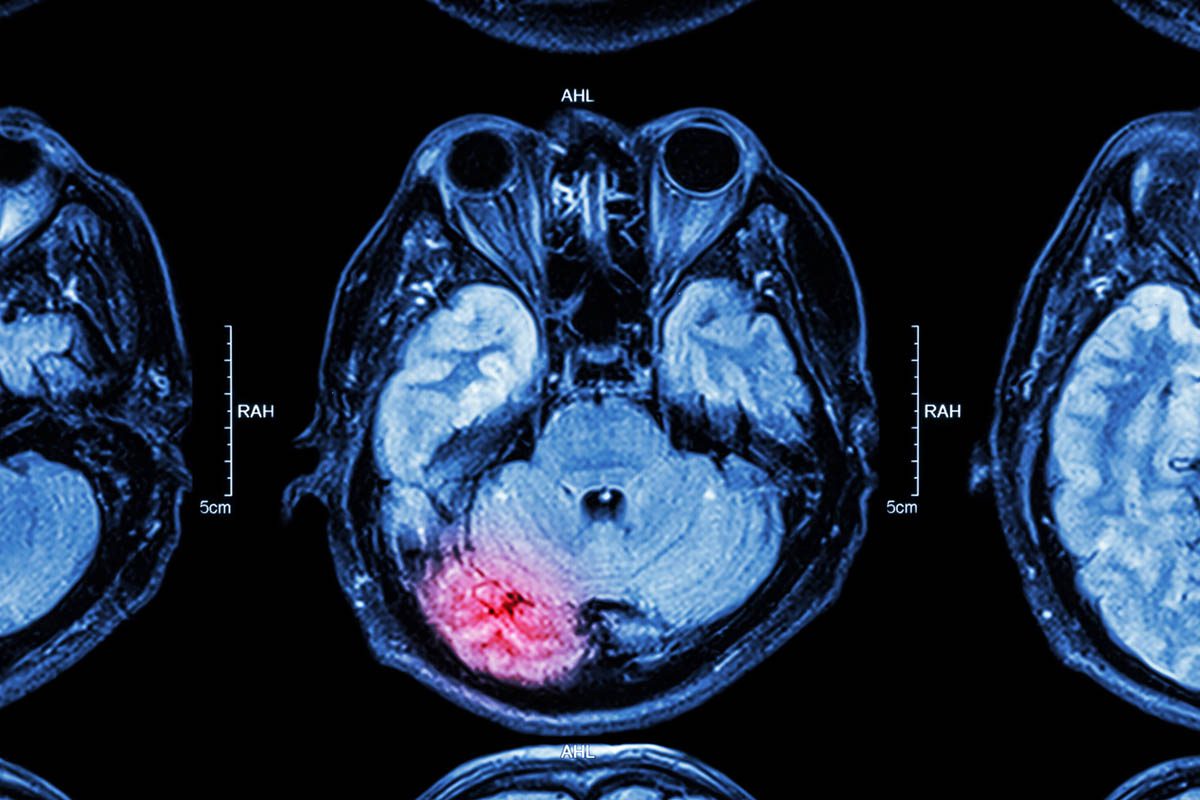
A variety of neurologic conditions and dysfunction of the central nervous system (including cerebrovascular accidents,15,16 multiple sclerosis, dementias, amyotrophic lateral sclerosis, delirium,8 complex partial seizures, dacrystic epilepsy,8 and traumatic brain injury) induce pseudobulbar affect. Sudden onset of involuntary bouts of crying (or laughing) that is incongruent to a patient’s mood or environment characterizes pseudobulbar affect, which is sometimes referred to as pathological crying, emotional lability, or emotional incontinence.17 Table 1 lists some of the common causes of crying.
CASE 2
Ms B, a 35-year-old woman, presented to the hospital with worsening abdominal pain. Her psychiatric history included major depressive disorder, an anxiety disorder, substance use disorders (opioid dependence treated with buprenorphine/naloxone, marijuana dependence, cocaine abuse), and several suicide attempts (by self-immolation and cutting her extremities and by drug overdoses), as well as a history of hepatitis C and a recent appendiceal inflammation.
From the start of her admission, Ms B was seen sobbing in her room while complaining of abdominal pain at a level of 8 out of 10 that failed to improve with intravenous morphine. After several tearful calls asking the nursing staff for analgesics, Ms B’s medical team became suspicious of her pain complaints and concerned that she was either depressed or drug-seeking, especially when a search for the source of her pain was unrevealing. Psychiatric consultation was requested to help evaluate whether Ms B had depression. During the psychiatric examination, Ms B was cooperative, but she sobbed and moaned (while complaining of significant pain). Although she had several neurovegetative symptoms of depression (including poor appetite, anhedonia, decreased energy, and difficulty with concentration), she denied having thoughts of suicide; she insisted that she wanted to get better and return to work.
Collateral information from her outpatient psychiatrist indicated that she was a high-functioning woman who was actively engaged in treatment despite her substance abuse disorder. The psychiatric consultant recommended use of a benzodiazepine, an increase in her antidepressant, and the involvement of the acute pain service to help manage her pain. Together with her primary medical team, the acute pain service, and a psychiatric consultant, a comprehensive plan for pain management was formulated and implemented. Ms B’s mood improved, her crying decreased, and she became more engaged with her treatment team, allowing for hospital discharge.
Case 2 Discussion
Ms B was depressed (endorsing several neurovegetative symptoms); collateral information confirmed that crying and emotional lability were atypical for her. A reasonable intervention for Ms B was pharmacologic management (an antidepressant and a benzodiazepine), as well as further assessment and evaluation of her pain. Ms B felt that her reports of pain went unrecognized by her care team until the acute pain service was involved in her care.
Ms B’s case also highlights the relatively high prevalence of pain that is undertreated in patients with significant substance use disorders.18 Although drug-seeking behaviors exist among some patients with substance use disorders, a thorough differential diagnosis not only helps to uncover the correct etiology of suffering but also informs appropriate management strategies.
CASE 3
Mr C, a 61-year-old man with a history of asthma, a recent-onset cardiomyopathy (with an ejection fraction of 15%), and a left-sided pleural effusion, was admitted to the medical service following a right middle cerebral artery cerebrovascular accident that was complicated by a left-sided posterior cerebral artery watershed infarct and obtundation. Since Mr C had recently had a thoracocentesis, tissue plasminogen activator was not administered.
Several days after his admission (in the setting of intermittent confusion, restlessness, and agitation that required physical restraints), Mr C was noted to have unprovoked bouts of crying, which seemed out of proportion to his reported mood and observed affect. His family expressed concerns about his new-found and heightened emotionality. After several unsuccessful attempts to manage his aggression and bouts of crying with intravenous haloperidol and oral quetiapine, psychiatric consultation was requested for the evaluation and treatment of agitation and depression. During the examination, Mr C was pleasant and capable of having a cogent conversation; his understanding of his medical diagnosis and treatment was good. He denied having any neurovegetative symptoms of depression (including thoughts of suicide). He had no signs or symptoms suggestive of delirium. The psychiatric consultant concluded that his presentation (with restlessness and discordance between his mood and emotional display) was secondary to pseudobulbar affect instead of a mood disorder (such as major depressive disorder or bipolar disorder). Pharmacologic treatment with dextromethorphan plus quinidine resulted in a diminished frequency and severity of Mr C’s crying episodes.
Case 3 Discussion
Mr C’s tearfulness and crying could be explained by several factors, including depression, demoralization, delirium, and negative emotions (such as anxiety, fear, helplessness) about the neurologic sequelae following his stroke. Mr C’s engagement in the psychiatric interview, inappropriate affect in relation to the content of the conversation, and inability to control his crying made his presentation more consistent with pseudobulbar affect. His denial of neurovegetative symptoms and suicidal ideation made depression less likely. A detailed course of his history and presentation was not suggestive of delirium. Pharmacologic interventions (including the use of antipsychotic medications) failed to provide relief because his presentation was not secondary to delirium. He responded well to treatment with dextromethorphan plus quinidine after the underlying etiology of his crying spells was established. We use the case of Mr C to further elaborate on how crying should be evaluated and managed in general hospital patients.
HOW SHOULD CRYING BE EVALUATED AND TREATED?
Developing a comprehensive differential diagnosis guides the appropriate evaluation of a patient who cries. There is no evidence-based approach to the assessment and evaluation of a patient who cries. However, primary medical and neurologic syndromes should be ruled out by obtaining a thorough medical history (including a psychiatric history), laboratory screening (eg, a basic metabolic panel, complete blood count, head imaging and other radiologic studies, and an electroencephalogram), and physical examination (eg, uncovering pain and its mechanism)—each provides clues about the etiology of crying. Collaborating with neurologists and other medical specialists can also provide useful insights and shape the assessment.
Crying is not always pathological. It can arise from positive emotions that do not require an intervention. Both pharmacologic and nonpharmacologic interventions can reduce the distress associated with crying, but treatment depends on the specific etiology. Pharmacologic interventions (including use of antidepressants, antipsychotics, benzodiazepines, mood-stabilizing anticonvulsants, amantadine, and dextromethorphan plus quinidine19) can reduce the frequency and severity of crying, especially in those with pseudobulbar affect.17 While there are no evidence-based nonpharmacologic interventions for crying, reassurance and expressions of empathy can provide relief to tearful patients. Reassurrance, education, cognitive-behavioral therapy,20 biofeedback, and relaxation techniques (such as deep breathing, meditation, and rhythmic movement of various muscle groups) can also be helpful.
HOW DO CLINICIANS REACT TO PATIENTS WHO CRY?
Most clinicians feel something (eg, sadness, irritation) when they encounter a patient crying and often attempt to express empathy.21 However, responses vary widely (eg, in the timing, tone, and content of expression).22 Empathy can be conveyed verbally and nonverbally.6 Verbal forms of empathic expression often involve statements such as, "This news must be very frightening for you to hear" or "I cannot imagine how unbearable your pain is at this time" or "This must be difficult for you, but we will do our best to help you through it."
Active listening with appropriate reflective statements and pauses (changes in pitch, prosody, and speed) allow patients to express themselves; these maneuvers can also convey empathy. Nonverbal expressions of empathy, including having a concerned facial expression, nodding to communicate understanding, nonsexual touching of the patient to provide comfort, sitting at eye level with the patient, or making direct eye contact (but not staring) with the patient, offer reassurance. Countertransference reactions to crying (such as frustration, helplessness, annoyance, anger, joy, and hopefulness) can lead to exploration of reactions, which informs evaluation and management.
CONCLUSION
Crying is a common and complex physiologic phenomenon; it is a universal experience in humans because of the various functions it serves and is frequent among general hospital patients. Our cases highlight several issues that impact evaluation and management. First, acknowledging a patient’s continuous crying and evaluating it can affect a patient’s treatment. Second, creating a broad differential diagnosis for crying is necessary since many clinicians erroneously assume that patients who cry are depressed. Management depends on the etiology of the crying; pharmacologic or nonpharmacologic interventions should be informed by the suspected etiology of the crying. The efficacy of different approaches and forms of empathic expression by clinicians is not evidence-based, and patients may respond differently to verbal and nonverbal forms of empathic expression. Crying evokes helping behaviors from others; most clinicians react with empathic expressions, although their reaction time and their mode of expression often vary.
REFERENCES
1. Rottenberg J, Gross JJ, Wilhelm FH, et al. Crying threshold and intensity in major depressive disorder. J Abnorm Psychol. 2002;111(2):302-312. PubMed doi:10.1037/0021-843X.111.2.302
2. Hendriks MC, Croon MA, Vingerhoets AJ. Social reactions to adult crying: the help-soliciting function of tears. J Soc Psychol. 2008;148(1):22-41. PubMed doi:10.3200/SOCP.148.1.22-42
3. Kipfer BA, ed. Roget’s 21st Century Thesaurus. 3rd ed. Princeton Language Institute. Princeton, NJ: Philip Lief Group; 2009.
4. GraÄanin A, Bylsma LM, Vingerhoets AJ. Is crying a self-soothing behavior? Front Psychol. 2014;5:502. PubMed
5. Rosenbaum L. Invisible risks, emotional choices—mammography and medical decision making. N Engl J Med. 2014;371(16):1549-1552. PubMed doi:10.1056/NEJMms1409003
6. Riess H, Kelley JM, Bailey RW, et al. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed doi:10.1007/s11606-012-2063-z
7. Stults CDLJ, Diamond L, MacLean L, et al. How do primary care physicians respond when patients cry during routine ambulatory visits? J Community Health. 2014;7(1):17-24. PubMed doi:10.1179/1753807614Y.0000000044
8. Green RL, McAllister TW, Bernat JL. A study of crying in medically and surgically hospitalized patients. Am J Psychiatry. 1987;144(4):442-447. PubMed doi:10.1176/ajp.144.4.442
9. American Psychiatric Association. Desk Reference to the Diagnostic Criteria From DSM-5. Washington, DC: American Psychiatric Publishing; 2013.
10. Calabrese LV, Becker A, Chamberlin E, et al. The impact of crying on length of stay in the general hospital. Paper presented at: Academy of Psychosomatic Medicine Meeting; November 11-14, 1993; New Orleans, LA.
11. Darwin C, Rachman S. The Expression of Emotions in Man and Animals. London, England; Dover, NH: F. Pinter; 1983.
12. Aubrey A. Teary-Eyed Evolution: Crying Serves a Purpose. National Public Radio. National Public Radio Web site. http://www.npr.org/templates/story/story.php?storyId=129329054. Updated August 23, 2010.
13. Vingerhoets AJ, Rottenberg J, Cevaal A, et al. Is there a relationship between depression and crying? A review. Acta Psychiatr Scand. 2007;115(5):340-351. PubMed doi:10.1111/j.1600-0447.2006.00948.x
14. Newman JD. Neural circuits underlying crying and cry responding in mammals. Behav Brain Res. 2007;182(2):155-165. PubMed doi:10.1016/j.bbr.2007.02.011
15. Andersen G, Ingeman-Nielsen M, Vestergaard K, et al. Pathoanatomic correlation between poststroke pathological crying and damage to brain areas involved in serotonergic neurotransmission. Stroke. 1994;25(5):1050-1052. PubMed doi:10.1161/01.STR.25.5.1050
16. Derex L, Ostrowsky K, Nighoghossian N, et al. Severe pathological crying after left anterior choroidal artery infarct. Reversibility with paroxetine treatment. Stroke. 1997;28(7):1464-1466. PubMed doi:10.1161/01.STR.28.7.1464
17. Pioro EP. Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs. 2011;71(9):1193-1207. PubMed doi:10.2165/11591450-000000000-00000
18. Chang YP, Compton P. Management of chronic pain with chronic opioid therapy in patients with substance use disorders. Addict Sci Clin Pract. 2013;8(1):21. PubMed doi:10.1186/1940-0640-8-21
19. Ahmed A, Simmons Z. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483-489. PubMed
20. Hofmann SG, Asnaani A, Vonk IJ, et al. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427-440. PubMed doi:10.1007/s10608-012-9476-1
21. Tai-Seale M, Lafata JE, Wunderlich T, et al. PS2-17: What happens when adult patients cry in primary care visits? Clin Med Res. 2012;10(3):180. doi:10.3121/cmr.2012.1100.ps2-17
22. PetriÄek G, Vrcić-Keglević M, Lazić D, et al. How to deal with a crying patient? A study from a primary care setting in Croatia, using the "critical incident technique." Eur J Gen Pract. 2011;17(3):153-159. PubMed doi:10.3109/13814788.2011.576339
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top