Prim Care Companion CNS Disord 2022;24(5):21cr03219
To cite: Gama Marques J. Diogenes, Plyushkin, or Havisham syndrome? syllogomania (hoarding with squalor) secondary to left cerebellopontine angle giant benign transitional meningioma. Prim Care Companion CNS Disord. 2022;24(5):21cr03219
To share: https://doi.org/10.4088/PCC.21cr03219
© 2022 Physicians Postgraduate Press, Inc.
aConsulta de Esquizofrenia Resistente, Hospital Júlio de Matos, Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal
bClínica Universitária de Psiquiatria e Psicologia Médica, Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal
*Corresponding author: João Gama Marques, MD, MSc, PhD, Pavilhão Salgado D’Araújo, Hospital Júlio de Matos, Centro Hospitalar Psiquiátrico de Lisboa, Avenida do Brasil, 53, 1749-002 Lisbon, Portugal ([email protected]).
Diogenes syndrome is not a specific disease but a real neuropsychiatric syndrome, characterized by severe domestic squalor, pathological hoarding, lack of insight, and no need for help.1 It was first described almost 50 years ago.2 Since then, many variant descriptions have been proposed, such as senile breakdown, social breakdown, senile squalor syndrome, or syllogomania.3 On the other hand, some do not approve of Diogenes syndrome as an eponym, named after a Greek cynic philosopher that lived in the fourth century before Christ, arguing it has little historical basis.4 At least, 2 alternative eponyms have been proposed. A masculine alternative version would be Plyushkin syndrome, inspired by a man from Nikolai Gogol’s book Dead Souls.5 The feminine alternative version would be Havisham syndrome, named after a woman from the novel Great Expectations by Charles Dickens.6
Case Report
A 67-year-old woman, living alone in an urban area, was brought to the emergency department for domestic hoarding and squalor in the last 6 months. At reception, a psychiatric disorder was hurriedly assumed by nurses, following the Manchester triage system. The patient looked disheveled and untidy. The interview was difficult because of moderate deafness, mental confusion, and perseverant speech. Vertigo, ataxic gait, and finger-to-nose dysmetria were also present. In her clinical file, there were no psychiatric records, but she was allergic to penicillin and suffered from arterial hypertension, gastritis, and constipation. Two months earlier she had fallen at home, resulting in a traumatic ischiopubic fracture, and was treated conservatively without surgery with dipyrone only. No neurologic or psychiatric disorders were known in her family.
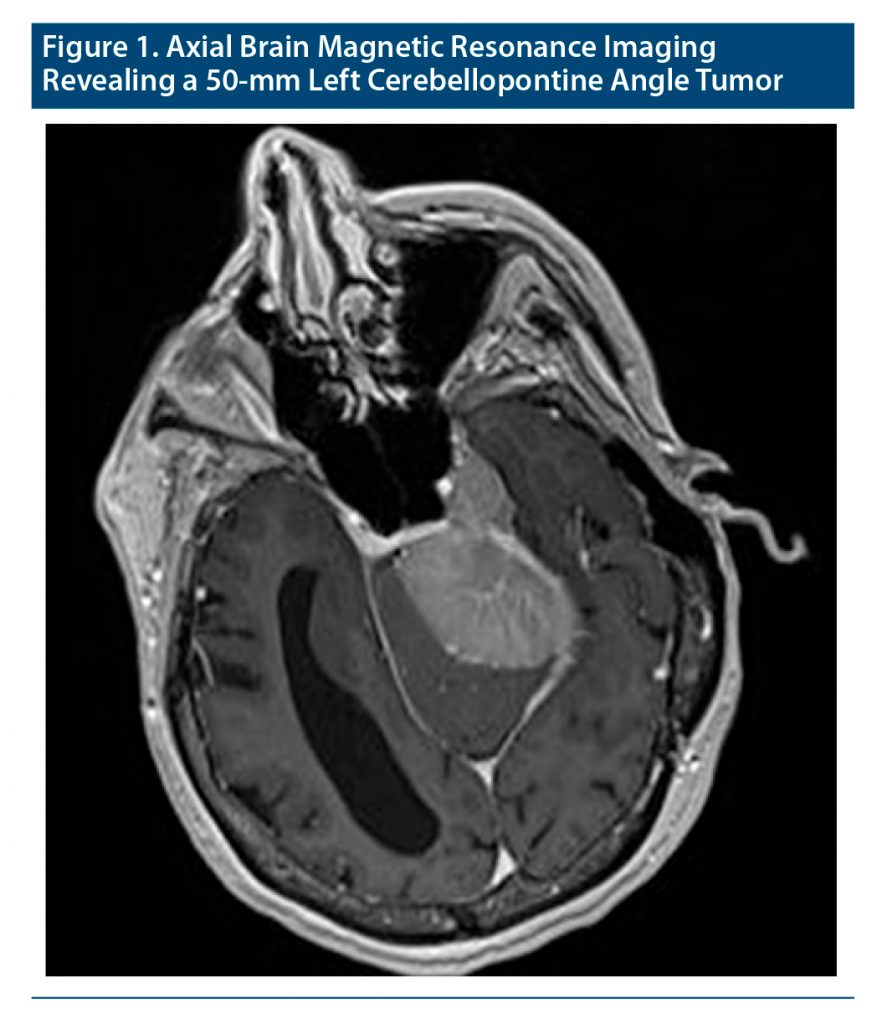
Blood and urine tests, electrocardiography, and chest radiograph were unremarkable. A magnetic resonance imaging brain scan revealed ventriculomegaly plus a 50-mm left cerebellopontine angle tumor (Figure 1). The patient was diagnosed with hoarding disorder and delirium due to a primary neoplasm of meninges (World Health Association, ICD-11 revision codes 6B24, 6D70, 2A01) and transferred to neurosurgery. Brain surgery revealed a giant left petroclival tumor partly compressing the left cerebellum and the cranial nerves of the left brain stem. Pathology confirmed World Health Organization benign (grade I) transitional meningioma. After 4 months in the general hospital ward, the patient was discharged to a continuous care unit. She was submitted to intensive physiotherapy for postsurgical sarcopenia and speech therapy for dysphagia and hoarseness. Nine months later at a follow-up appointment, she was on daily oral omeprazole 20 mg/d for chronic gastritis, bisacodyl 5 mg for constipation, amlodipine 5 mg for arterial hypertension, levetiracetam 1,000 mg for seizure prevention, and quetiapine 100 mg for insomnia. At that time, complete remission of psychiatric and neurologic symptomatology was achieved.
Discussion
According to a systematic review,7 Diogenes syndrome can be easily associated with dementia (19%) and compromised mobility (19%) but also, less frequently, with falls (9%) and tumors (6%). Diogenes syndrome was also recently described by Sacchi et al,8 16 years after craniotomy for excision of a left parietal meningioma, in a patient with alcohol abuse and frontotemporal dementia. Both cases (Sacchi et al8 and the present case) will most likely become the first of many others to come, as this syndrome spectrum is getting more recognition. Many meningiomas are slow-growing neoplasms.9 But, as cerebellopontine angle is a sensible neuroanatomical area (especially compared with the parietal lobe), it is easy to understand the (years versus months) differences in the natural history of disease between these 2 cases. Indeed, the patient presented here most likely suffered a faster sequence of events involving the local neurocircuits that would correspond to her symptomatology. Presurgical cerebellum compression would explain dysmetria and ataxia, while vestibulocochlear nerve (VIII cranial nerve) compression would explain vertigo and left-side deafness. Indeed, petroclival meningiomas are regarded as one of the most formidable challenges in neurosurgery.10 Therefore, postsurgical damage at glossopharyngeal and vagus nerves (cranial nerves IX and X) could explain transitory dysphagia and hoarseness. Finally, although there were no signs of hydrocephalus, intracranial hypertension would compress frontal lobes, causing not only mental confusion, but also loss of self-awareness with a failure to discard and an innate impulse to take environmental items.11
This case is just another example of many patients sent to our care due to a psychiatric misdiagnosis with no previous brain-imaging examination.12–17 Yes, we are still paying the price for the Cartesian catastrophe.18 But, still, why? Why, in the age of brain scans, is a brain tumor mistaken for a psychiatric disorder?19
Published online: October 13, 2022.
Relevant financial relationships: None.
Funding/support: None.
Patient consent: Permission was obtained from the patient to publish this case report, and information was de-identified to protect anonymity.
References (19)

- Assal F. Diogenes syndrome. Front Neurol Neurosci. 2018;41:90–97. PubMed CrossRef
- Clark AN, Mankikar GD, Gray I. Diogenes syndrome: a clinical study of gross neglect in old age. Lancet. 1975;305(7903):366–368. PubMed CrossRef
- Dossey L. Syllogomania. Explore (NY). 2005;1(6):415–419. PubMed CrossRef
- Marcos M, Gómez-Pellín MdeL. A tale of a misnamed eponym: Diogenes syndrome. Int J Geriatr Psychiatry. 2008;23(9):990–991. PubMed CrossRef
- Cybulska E. Senile squalor: Plyushkin’s not Diogenes’ syndrome. Psychiatr Bull. 1998;22(5):319–320. CrossRef
- Byard RW. Diogenes or Havisham syndrome and the mortuary. Forensic Sci Med Pathol. 2014;10(1):1–2. PubMed CrossRef
- Almeida R, Ribeiro O. Diogenes syndrome: systematic literature review. Rev Port Saude Publica. 2012;30(1):89–99.
- Sacchi L, Rotondo E, Pozzoli S, et al. Diogenes syndrome in dementia: a case report. BJPsych Open. 2021;7(2):e43. PubMed CrossRef
- Zeidman LA, Ankenbrandt WJ, Du H, et al. Growth rate of non-operated meningiomas. J Neurol. 2008;255(6):891–895. PubMed CrossRef
- Zhao Z, Yuan X, Yuan J, et al. Treatment strategy for petroclival meningiomas based on a proposed classification in a study of 168 cases. Sci Rep. 2020;10(1):4655. PubMed CrossRef
- Finney CM, Mendez MF. Diogenes syndrome in frontotemporal dementia. Am J Alzheimers Dis Other Demen. 2017;32(7):438–443. PubMed CrossRef
- Gama-Marques J, Palhavã F, Brissos S. Subarachnoid hemorrhage misdiagnosed as adjustment disorder. Br J Psychiatry. 2015;37(1):81. PubMed CrossRef
- Gama Marques J, Saraiva S, Brissos S. Frontotemporal dementia mimicking bipolar affective disorder, normal pressure hydrocephalus and Klüver-Bucy syndrome. Asian J Psychiatr. 2015;18:106–107. PubMed CrossRef
- Gama Marques J. Twenty years of misdiagnosis of schizophrenia in a patient with Dandy-Walker variant syndrome. Gen Psychiatr. 2019;32(1):e100031. PubMed CrossRef
- Gama Marques J. Brain metastasis affecting frontal lobe misdiagnosed as bipolar disorder, without any neuroimaging exam: two case reports with fatal outcomes. CNS Spectr. 2019;24(2):229–230. PubMed CrossRef
- Gama Marques J. Psychotic polyembolokoilamania secondary to left parietal lobe glioblastoma. Acta Neurol Belg. 2019;119(2):279–280. PubMed CrossRef
- Gama Marques J. Left frontal lobe meningioma causing secondary schizophrenia misdiagnosed for 25 years. Prim Care Companion CNS Disord. 2020;22(2):19l02466. PubMed CrossRef
- Stensson J. Editorial: shellac records, the Cartesian catastrophe and psychoanalysis. Int Forum Psychoanal. 1997;6(2):69–70. CrossRef
- Caruso R, Piro A. Why in the age of CT scans and MRIs is a brain tumor mistaken for a psychiatric illness? BMJ Case Rep. 2017;2017:bcr-2017-220131. PubMed CrossRef
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top