Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
To the Editor: Selective serotonin reuptake inhibitors (SSRIs) are some of the most commonly prescribed medications. Although adverse skin reactions are commonly associated with psychotropic medications, SSRIs are generally not associated with serious cutaneous side effects, and evidence of an association is limited to case reports.
Case report. The patient is a 19-year-old woman with a history of asthma, allergic rhinitis, and Hashimoto’s thyroiditis.
To the Editor: Selective serotonin reuptake inhibitors (SSRIs) are some of the most commonly prescribed medications. Although adverse skin reactions are commonly associated with psychotropic medications,1,2 SSRIs are generally not associated with serious cutaneous side effects, and evidence of an association is limited to case reports.3,4
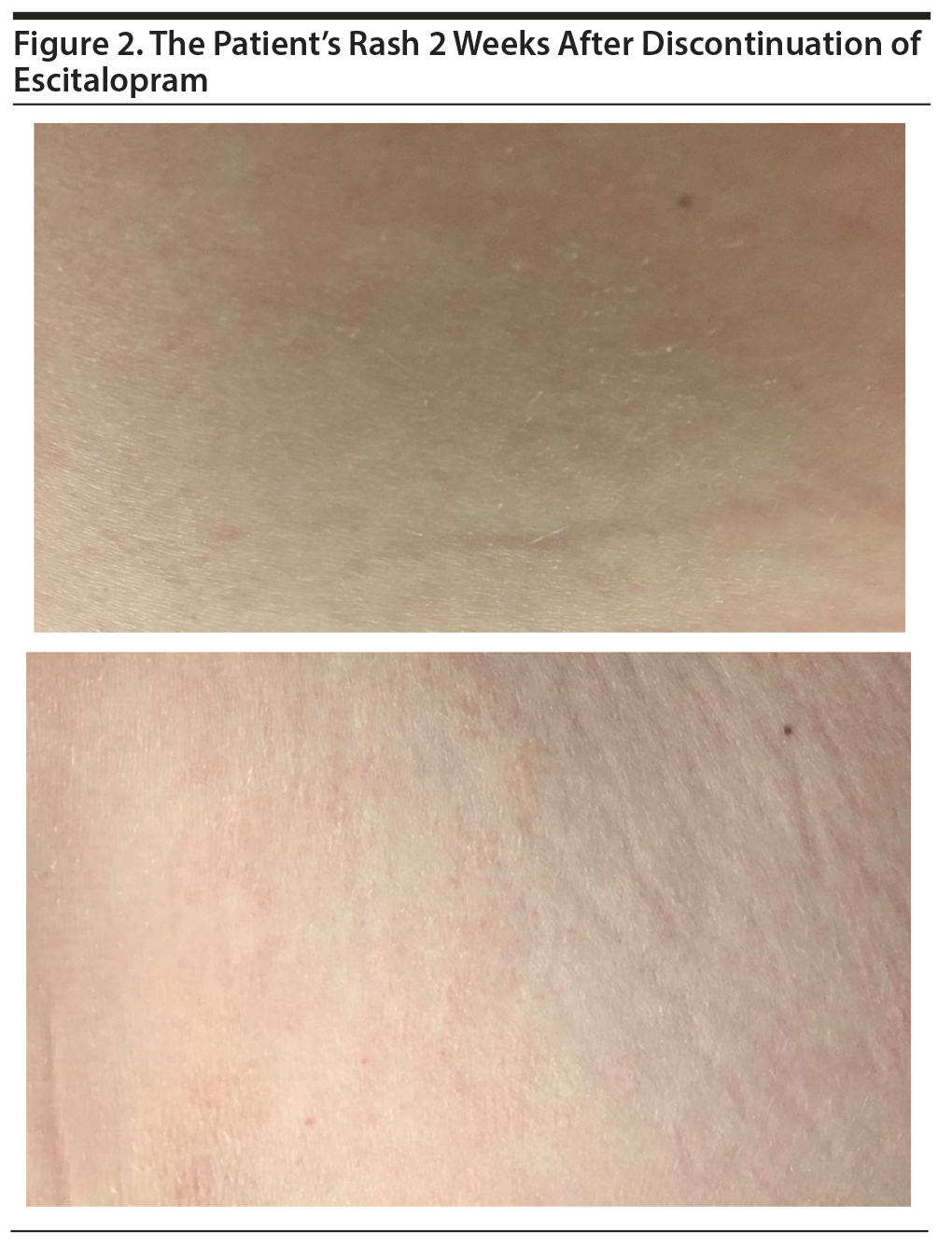
Case report. The patient is a 19-year-old woman with a history of asthma, allergic rhinitis, and Hashimoto’s thyroiditis. She was started on escitalopram 5 mg daily for symptoms of anxiety and depression. The patient had never taken antidepressants prior to the initiation of escitalopram. At baseline, the patient was taking loratadine for allergies, albuterol and budesonide/formoterol inhalers for asthma, and levothyroxine for hypothyroidism. She reported that about 4 weeks after starting the medication, a rash appeared on her right buttock and gradually spread to her lower back. The patient remained compliant with escitalopram, and at 2 months she continued to report a pruritic rash on her lower back and right buttock (Figure 1). On examination, we observed a rash with slightly elevated papules and localized erythema. No laboratory abnormalities were noted, and her thyroid-stimulating hormone level was within normal limits. Given that there were no other changes in the patient’s lifestyle or medication regimen and her preference, a decision was made to discontinue escitalopram. The patient reported resolution of the rash and associated itching 2 weeks after discontinuation of escitalopram (Figure 2). She was subsequently started on fluoxetine 10 mg and reported no reemergence of the rash.
Given the temporal association and lack of an alternative explanation, we believe that the patient’s rash was secondary to escitalopram. In animal models, SSRI-induced skin reactions, specifically itching, are thought to be mediated by 5-hydroxytryptamine receptor 7 and transient receptor potential cation channel, subfamily A, member 1 receptors.5 However, such an association has not been established in humans.
It is noteworthy that our patient has a history of asthma as well as an autoimmune disease, which may have rendered her vulnerable to skin reactions. Further, that the patient had no adverse skin reaction after being started on fluoxetine suggests that her specific skin reaction was not SSRI class dependent; this finding is different from what has been reported in the literature wherein a class-dependent effect was observed between sertraline and escitalopram.4 Some patients do experience serious skin reactions secondary to antidepressant medications, and this risk should be considered in patients who may be uniquely vulnerable. If a reaction is observed, switching to another antidepressant may be a safe option for ongoing treatment.
References
1. Bliss SA, Warnock JK. Psychiatric medications: adverse cutaneous drug reactions. Clin Dermatol. 2013;31(1):101-109. PubMed CrossRef
2. Herstowska M, Komorowska O, Cubała WJ, et al. Severe skin complications in patients treated with antidepressants: a literature review. Postepy Dermatol Alergol. 2014;31(2):92-97. PubMed CrossRef
3. Sannicandro TJ, Farrar MC, Markowitz JS. Selective serotonin reuptake inhibitor-induced rash: case report and review of the literature. Pharmacotherapy. 2002;22(4):516-518. PubMed CrossRef
4. Dadić-Hero E, Ružić K, Grahovac T, et al. Allergic reactions: outcome of sertraline and escitalopram treatments. Psychiatr Danub. 2011;23(1):120-122. PubMed
5. Morita T, McClain SP, Batia LM, et al. HTR7 mediates serotonergic acute and chronic itch. Neuron. 2015;87(1):124-138. PubMed CrossRef
aDepartment of Psychiatry, Behavioral Health Services, Henry Ford Health System, Detroit, Michigan
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Written consent was obtained from the patient to publish this report including images. Information has been de-identified to protect anonymity.
Published online: January 31, 2019.
Prim Care Companion CNS Disord 2019;21(1):18l02302
To cite: Prabhakar D, Sablaban I. Escitalopram-induced rash. Prim Care Companion CNS Disord. 2019;21(1):18l02302.
To share: https://doi.org/10.4088/PCC.18l02302
© Copyright 2019 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top