Fainting, Swooning, and Syncope
Have you ever been curious about how serious fainting, swooning, and syncope are or can be? Have you wondered whether, when, and how to work up these conditions? Have you ever considered how to best treat a patient with single or multiple episodes of syncope? If you have, then the following case vignette should provide a useful stimulus for discussion.
CASE VIGNETTE
Ms A, a 28-year-old single woman with several months of fainting episodes, was seen for an evaluation of anxiety. She appeared athletic and interpersonally appropriate. She worked in the financial services industry (where she achieved success and promotions) and, in her spare time, skated with a women’s roller derby team.
Most of her episodes of light-headedness and, at times, passing out occurred while warming up for roller derby games. She had been with the team for about 18 months. After 12 months, her skating had improved to the point that she was asked to take on the role of a “jammer.” In roller derby, each team has 2 jammers. Skaters from both teams form the “pack.” Jammers start behind the pack and, with the help of teammates, attempt to get free of the pack and then lap or overtake the pack. The jammers score points by passing members of the opposing team. After skating as a jammer for several games, Ms A began to experience light-headedness during warm-ups and, on a few occasions, passed out for less than 30 seconds.
Ms A’s medical history was notable for juvenile-onset diabetes (for which she had been taking insulin for years) and mitral valve prolapse. Following several episodes of fainting, she contacted her physician, who checked a variety of blood tests (eg, Chem-7, thyroid function tests, complete blood count [CBC]) and referred her to a cardiologist. Results of her stress test and a Holter monitor were unremarkable. When Ms A returned to skating in the pack, her episodes ceased. Ms A’s family history revealed that one of her father’s 2 siblings, a brother, had died suddenly in his early 40s.
Her parents, both excellent athletes, met playing college tennis. Not surprisingly, Ms A was a very good athlete; she had played competitive tennis since she was a child and was quite successful at sports until her early teens. Then, when Ms A started to play in regional tournaments, she began to lose matches after being significantly ahead. She reported feeling increasingly anxious as these tournaments approached and became especially anxious as she progressed to the championship round. Ms A’s father insisted that she undergo extensive medical testing and arranged for her glucose level to be checked during practice sessions and matches. She also played high school soccer and was an accomplished defensive player. However, when her coach moved her to the forward position, she became quite anxious (both in practice and before games) and recalled feeling light-headed during warm-ups. After enrolling in college, Ms A stopped playing competitive team sports. Nevertheless, she ran routinely. Roller derby marked Ms A’s return to organized competitive sports.
Ms A had no idea why she was anxious or what was responsible for her fainting. She engaged in a course of brief planned psychotherapy that targeted her emotional and physiologic response to being the aggressor and winning. Ms A used this opportunity to uncover aspects of her relationship with her father and his need for her to excel. She became much more comfortable with achieving her own goals, and her bouts of syncope ceased.
HOW ARE FAINTING, SWOONING, AND SYNCOPE DEFINED?
Syncope, the medical term for fainting/blacking out, is traditionally characterized by a sudden and temporary loss of consciousness (with spontaneous recovery) caused by insufficient oxygen delivery to the brain (via hypotension or other mechanisms).1 Syncope is a word that often induces fear in patients and their physicians, and the condition frequently leads to hospitalization for further evaluation. The term fainting (more familiar to laypersons) is less intimidating and rarely results in admission to a health care facility. These conditions are differentiated from presyncope or near-syncope, during which an individual can remember manifestations (eg, dizziness, blurred vision, weakness, the fall). Its signs and symptoms include pallor, rapid breathing, nausea, and weakness (particularly of the limbs, leading most individuals to sit down if there is time to do so).
Clinical Points
- Knowledge of predisposing factors and pathophysiologic underpinnings can guide the assessment and treatment of syncope.
- Measurement of vital signs, carefully recorded orthostatic/postural heart rate and blood pressure, along with a basic metabolic panel, a complete blood count, and an electrocardiogram, should be part of the initial evaluation of syncope.
- Unfortunately, approximately 20% to 40% of episodes that present as transient loss of consciousness remain unexplained, in part, because the evaluation of these episodes relies on retrospective information.
Fainting, attributed to a variety of ailments, has been recognized as a problem for centuries (Table 1). It was described by Hippocrates (in his Aphorisms)2,3 as “passing out” and later by Galen4 as a sudden prostration of the vital powers or falling into a swoon. Depictions of fainting and swooning abound in the arts (eg, Tintoretto’s Esther before Ahasuerus)5 and have been the subject of cartoons and humor (such as cartoons on fainting found at CartoonStock.com), as well as popular YouTube videos (eg, of fainting goats).
Just as the term syncope is commonly used by physicians today, the word lipothymia (derived from leipo [to leave] and thymia [the mind]) was often employed in common parlance for centuries, and the documentation of lipothymia is as old as medicine itself.2 Indeed, this phenomenon has been so frequently seen that it led to the creation of types of furniture and clothing and even a room (that bears its name) in the homes of many affluent Victorian families. The fainting couch (commonly found on the stair landings of Victorian mansions) and the fainting parlor were status symbols among Victorian society (as meaningful a measure of wealth as the number of chimneys in a house).
HOW IMPORTANT IS IT TO KNOW THE CAUSE OF A PERSON’ S FAINTING?
Do we always need to know the etiology of fainting? While the obvious answer is no, it is worth analyzing how clinical decisions are made and how a diagnosis and treatment plan may be established following a syncopal episode.
There are very few disorders in clinical medicine for which the story (commonly called the “history of present illness”) is more valuable than it is in the initial evaluation of syncope. The context in which syncope occurs typically establishes the etiology. The history of present illness (the story), along with a few facts about the patient’s demographics and medical history (eg, age, comorbidities, family history of syncope), is the single most significant information when determining the cause of syncope and guiding the physician in the diagnostic evaluation.1,6-8 Nevertheless, the cause of syncope remains undetermined in up to 35% of cases despite extensive diagnostic work-ups.6 It is imperative for a physician to keep an optimistic, yet realistic, view of the value of proceeding with a “full” work-up following syncope when the story itself does not reveal the etiology.
Although most individuals with syncope can be diagnosed on the basis of their story and history, further work-up is indicated for those in whom the consequences of not knowing the etiology (and appropriately treating it) may negatively impact their outcome.7 Among these are patients who suffer from recurrent bouts of syncope, those with symptoms (chest pain, palpitations) that heralded the episode, those in whom fainting caused serious injury, those with a significant history of heart disease or a risk for it (eg, diabetes, peripheral vascular disease, cerebrovascular disease), those who remained unconscious for more that a few minutes, and those who are pregnant. In each of these categories, syncope may arise from a potentially lethal cause, or fainting may serve as the harbinger of a more serious clinical disorder.
WHAT SHOULD THE EVALUATION OF SYNCOPE INCLUDE?
History and Story
The story (along with a detailed past medical history and family history) should be obtained; particular attention should be paid to the prodrome, situation, position, and context that surrounds the syncopal episode (eg, its relationship with exercise, use of medications and recreational drugs), as well as the patient’s social history (Table 2).1,7-9
Physical Examination
Measurement of vital signs, along with carefully recorded orthostatic/postural heart rate and blood pressure, should always be included in the initial evaluation of syncope. Careful examination of the cardiovascular and neurologic systems can be quite revealing.1,7,9
Laboratory Tests (including serum studies)
A basic metabolic panel (including electrolytes, tests of renal function [blood urea nitrogen, creatinine], and serum glucose), a CBC count, and an electrocardiogram (ECG) should be obtained as part of the initial evaluation. Guided by other contributing factors, this list may be expanded to include other specialized tests (such as thyroid function tests, cardiac enzymes, and other serologic markers of disease).7,9
Once these basic steps have been completed in the initial evaluation of syncope, the work-up may be expanded if it is deemed appropriate by both the patient and physician.
WHAT IS THE DIFFERENTIAL DIAGNOSIS FOR SUDDEN LOSS OF CONSCIOUSNESS?
Transient loss of consciousness has a rapid onset and a short duration; it is usually associated with loss of postural tone. Not included in this category are conditions (such as intoxications, infections, hepatic encephalopathy, or underlying metabolic derangements [eg, sodium abnormalities]) that induce an altered sensorium.10 Transient loss of consciousness has a myriad of causes (some are time limited, such as breath holding, and others are potentially lethal, such as pacer malfunctions). A practical approach to the evaluation of a seemingly overwhelming number of potential etiologies for transient loss of consciousness starts with exclusion of obvious causes (eg, head trauma, aborted cardiac arrest).
Causes of transient loss of consciousness can, in general, be divided into 4 major categories: neurocardiogenic (also known as reflex or neurally mediated loss of consciousness), orthostatic hypotension, cardiovascular, or neurogenic.7,11 The first 3 categories (called syncope) arise from a global decrease in cerebral blood flow. Neurologic causes typically involve more focal brain disturbances (eg, seizures, transient ischemic attacks, strokes, or vertebrobasilar insufficiency) that result in impaired blood flow in the posterior circulation of the brain (eg, as occurs with overextension of the neck).
Unfortunately, as previously stated, approximately 20% to 40% of episodes that result in transient loss of consciousness remain unexplained.1 Since the evaluation of these episodes relies on a retrospective history and potentially dysfunctional doctor-patient communication (eg, when the patient cannot or will not provide details surrounding the episode), the differential diagnosis needs to be broad (including drop attacks, psychogenic causes, hypoglycemia, and a postfall concussion with retrograde amnesia).7
WHAT CAUSES SYNCOPE?
To sustain consciousness, the brain requires a minimum of 3 mL O2 per 100 g of tissue per minute; syncope may develop when less than this amount of oxygen reaches the brain.7 Fortunately, under normal circumstances, there is sufficient reserve in both the supply and delivery of oxygen from the lungs to the brain.
A severe reduction in oxygen delivery to the brain can result from an inability to extract oxygen from the environment. For example, in conditions of extreme hypoxia, loss of consciousness may occur.12,13 Additional modifiers of oxygenation include atmospheric pressure, underlying pulmonary function, red blood cell mass, or conditions that alter oxygen-carrying capacity (eg, carbon monoxide poisoning, methemoglobinemia, cyanide poisoning, hypophosphatemia, hypothermia or hyperthermia, and an abnormal acid base status).14
Although impaired oxygen extraction and altered oxygen-carrying capacity can play a role in the development of syncope, the most common mechanism for impaired oxygen delivery to the brain involves a decrease in global cerebral perfusion.15 Cerebral blood flow is determined primarily by both cerebral perfusion pressure and intracranial pressure, as well as by the partial arterial pressures of oxygen (PaO2) and of carbon dioxide (PaCO2).15 In general, as the PaCO2 falls (as can occur with hyperventilation in the presyncopal period), cerebral blood flow diminishes, hastening the onset of syncope.15
Reduction in cerebral perfusion pressure is the fundamental mechanism behind most causes of syncope.15 Cerebral blood flow is kept constant by autoregulatory mechanisms across a range of cerebral perfusion pressures (approximately 50-150 mm Hg). However, at lower cerebral perfusion pressures, the relationship between cerebral perfusion pressure and cerebral blood flow becomes linear.15 Perfusion of the brain typically decreases as cerebral perfusion pressure falls. The primary determinant of cerebral perfusion pressure is the mean arterial pressure, which is in turn related to cardiac output and to systemic vascular resistance.15 Therefore, any factor that lowers either of these parameters can cause syncope by impairing global brain perfusion.
Syncope most often results from neurocardiogenic causes, cardiovascular causes, and orthostatic hypotension; these categories of conditions account for approximately 30%, 20%, and 10% of syncopal episodes, respectively.1,9 Overall, the incidence of syncope increases with advancing age.6 In addition, syncope in young patients is most often secondary to neurocardiogenic causes, but as individuals age, cardiovascular causes of syncope increase in prevalence.16
The primary mechanism by which disorders in each of these broad categories results in syncope varies. A decrease in cardiac output is the primary mechanism for cardiovascular causes of syncope, while a drop in vascular tone is the primary pathologic correlate of loss of consciousness associated with orthostatic hypotension.13,17 Both mechanisms are involved in neurocardiogenic syncope.
Syncope due to orthostatic hypotension results from a postural decrease in cerebral perfusion caused by a decrease in vascular tone.13,17 Inadequate vascular tone can result in decreased preload or decreased systemic vascular resistance or both. The cycle of sudden loss of consciousness and quick recovery after loss of postural tone characteristic of syncope can be understood by reviewing the physiologic responses that are commonly seen in orthostatic hypotension. When a patient stands, there is a sudden drop in mean arterial pressure due to pooling of blood in the lower extremities or a drop in systemic vascular resistance. Most often, this is accompanied by a compensatory increase in heart rate. The sudden decrease in cerebral perfusion results in syncope with a loss of postural tone. As a patient collapses, the increased venous return and subsequent increased left ventricular filling restores blood pressure and cerebral perfusion with restoration of cerebral oxygen flow and the patient awakens.13
The causes of impaired vascular tone include hypovolemia (eg, from dehydration, hemorrhage, adrenal insufficiency, diuretics), autonomic neuropathy (eg, associated with diabetes, amyloidosis, Parkinson’s disease, Shy-Drager syndrome, Lewy body dementia, use of alcohol or anticholinergics), or use of vasodilators (eg, antihypertensives, nitrates, histamines, alcohol).13,17
The most common cardiopulmonary causes of syncope are bradyarrhythmias and tachyarrhythmias (eg, heart block, sick sinus syndrome, ventricular or supraventricular tachycardias, Wolff-Parkinson-White syndrome, and torsades de pointes, usually in the setting of corrected QT interval prolongation).1,7 Bradyarrhythmias, especially when of sudden onset, can become symptomatic and result in syncope. Several structural problems (eg, valvular defects [aortic stenosis, mitral stenosis, or pulmonic stenosis] or other conditions that impair cardiac outflow, eg, systolic dysfunction, cardiomyopathies, tamponade, and atrial myxomas) result in decreased cardiac output (either at rest or with exertion). Pulmonary and vascular abnormalities (eg, pulmonary embolism, tension pneumothorax, pulmonary hypertension, compression of the inferior vena cava [as can occur in pregnancy], aortic dissection, and subclavian steal syndrome [that results in retrograde blood flow in the vertebral artery in the setting of a proximal subclavian artery stenosis and ipsilateral arm exercise]) also decrease cardiac output or impair cerebral perfusion.7
Neurocardiogenic syncope (also referred to as vasovagal syncope, neurally mediated syncope, or reflex syncope) frequently involves a decrease in both cardiac output and systemic vascular resistance.7,13,18 Neurocardiogenic syncope can occur in emotionally challenging (eg, scary or embarrassing) situations, such as during blood drawing, while observing one’s first autopsy, seeing blood or needles, or receiving bad news, or from carotid sinus hypersensitivity.
Regardless of the trigger, neurocardiogenic syncope is caused by a hyperactive vagal response to mechanoreceptor stimulation in the left ventricle (vasovagal), carotid sinus (carotid sinus hypersensitivity), bladder (postmicturition), gastrointestinal tract (postdefecation), or trachea (posttussive). Stimulation of mechanoreceptors at these sites results in both a drop in the heart rate and a decrease in the blood pressure due to decreased systemic vascular resistance from an exaggerated vagal response. The enhanced parasympathetic tone causes a drop in heart rate and heart contractility, whereas the withdrawal of sympathetic tone in blood vessels results in vasodilation.7,18 The ensuing drop in blood pressure decreases blood flow and results in syncope. In some individuals, maneuvers known to activate the vagal response (such as bearing down, laughing intensely, pressing on the eyes, or having cold water come in contact with the face) can trigger the exaggerated neural reflex that results in syncope. Occasionally, however, the blood pressure and heart rate may be affected independently. These “nonclassical” causes include pure autonomic failure or postural tachycardia syndrome.16
WHICH PSYCHIATRIC CONDITIONS OR TREATMENTS PREDISPOSE TO SYNCOPE?
While it is well known that strong affective experiences are associated with neurocardiogenic syncope, a comprehensive literature search of psychiatry and syncope fails to yield a wealth of information. A MEDLINE query, using the keywords syncope, psychiatry, and fainting, yields no more than 10 articles since 1996. This is partly explained by the fact that most episodes of syncope cannot (by definition) be well described by the patient and are not witnessed by others. Additionally, most presentations of fainting are evaluated by emergency room and primary care physicians19,20; only those patients who suffer repeated episodes that are deemed largely psychogenic are seen by a psychiatrist. Therefore, a large proportion of patients who are vulnerable to emotionally driven syncopal episodes never receive formal psychiatric screening. While up to one-fourth of syncopal episodes are of psychiatric origin,21 fainting is perhaps the best predictor of an as yet undiagnosed occult psychiatric syndrome.22,23 However, “psychiatric origin” is often ill defined. Although certain syndromes (panic disorder and hypochondriasis) are the psychiatric conditions most commonly associated with syncope, psychiatric origin can also suggest strong emotional reactions in the absence of a DSM-IV-defined24 psychiatric disorder.
Neurocardiogenic syncope is associated with a powerful emotional response derived from strong adrenergic responses (fight-or-flight mechanisms) followed by a “rebound” of parasympathetic tone and a decrease in mean arterial pressure. Cardiac output drops, vasodilatation increases, blood pressure falls, and a patient faints as his/her brain responds to rapid and uncompensated transient hypoxia.
“Going to ground” utilizes decreased gravitational demands on blood flow to quickly restore oxygen return to the central nervous system, and both sympathetic and parasympathetic responses return to normal quickly. In fact, for these physiologic reasons, rapid recovery—in seconds to a few minutes—is pathognomonic for neurocardiogenic syncope.13 Longer episodes of decreased consciousness require a search for other causes.
Prodromal symptoms characteristic of neurocardiogenic syncope are similar to those of a panic attack. In fact, given the comorbidity of panic disorder and syncope, it stands to reason that symptoms preceding syncope will be consistent with panic attacks (with diaphoresis, palpitations, tremor), as well as a diminishing field of vision as blood supply to the brain decreases. Psychological symptoms, as with panic attacks, often include feelings of dread or intense fear.25 As parasympathetic tone increases, dissociative experiences are often noted, and syncope usually occurs within seconds to minutes of the initially reported fear or dread.26,27 Quick recovery is the rule; if a patient does not revive almost immediately, another cause of syncope should be sought.
Psychiatric treatment of syncope includes behavioral therapy aimed at decreasing arousal to the identified stimulus, as well as pharmacologic interventions that decrease immediate anxiety and prevent the onset of downstream anxiety.28 Medications (such as benzodiazepines, selective serotonin reuptake inhibitors, and β-blockers) have all been efficacious.28-30 It is also important to explore the patient’s narrative related to syncopal events. Thus, interventions for psychiatric syncope tend to be integrative and individualized (depending on the patient’s needs and preferences).27-30
Given the apparent maladaptive nature of syncope, one might wonder how a behavior driven by the brainstem itself would persist within our species. Since the brainstem is primitive, its impact on neurocardiogenic syncope can be understood in an evolutionary context. Evolutionary biologists and behaviorists have noted that it is primarily humans and primates that experience syncope in the setting of strong emotional reactions.31 From this observation, some have postulated that the initial fight-or-flight mechanism that is activated upon seeing blood, for example, is a natural response to what might be viewed as a threatening situation.32 If the fight-or-flight response does not diminish the threat, blood is likely to continue flowing in the threatened individual, and the parasympathetic rebound leads to syncope in an effort to maintain hemostasis. This explanation, like all evolutionary postulates, is teleological; however, it does offer some insight into how a maladaptive behavior (such as fainting) continues to be preserved.32
In summary, syncope of psychiatric origin is most often neurocardiogenic. Treatment of syncope is often identical to the treatment for severe anxiety; it involves both psychotherapy and use of medications. As epidemiologic data suggest, many more patients experience syncope than their doctors might expect, and it behooves clinicians to screen for past episodes of syncope in any initial evaluation and treatment plan.24
CLINICAL EVALUATION FOLLOWING SYNCOPE
Neurocardiogenic Causes of Syncope
In cases wherein neurally mediated syncope is suspected (eg, vasovagal, situational, postmicturition) and when the story and the basic laboratory assessment are insufficient to substantiate a diagnosis, tilt table testing and/or the careful evaluation of vital signs and symptoms after applying carotid massage may be appropriate.6,9 Although not highly sensitive, these maneuvers may assist in exonerating positional syncope and carotid hypersensitivity syndrome as potential causes of fainting.
Cardiac Causes of Syncope
Although cardiogenic syncope is often heralded by a substantial history of structural and/or vascular heart disease,8 several technologies and tests (eg, ECG, Holter monitors, electrophysiologic studies) can be employed to fully evaluate syncope. An echocardiogram can screen for structural and valvular heart disease as well as functional disease of the myocardium. A Holter monitor (or a more advanced tool, such as a loop recorder monitor) may assist in screening for dysrhythmias. In some individuals, full electrophysiologic testing (to include pharmacologic stimulation and testing) may uncover more unusual or difficult-to-diagnose etiologies of arrhythmogenic syncope.1,6,7,9
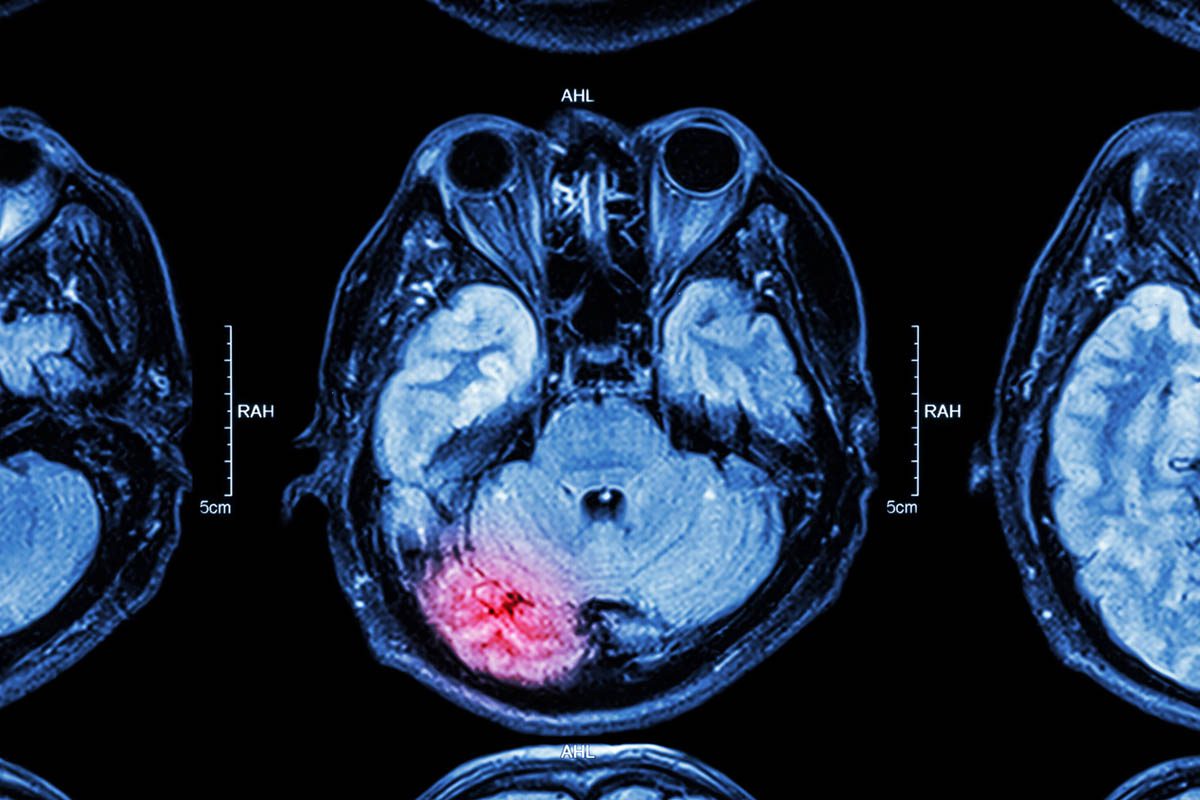
Neurologic Causes of Syncope
Although neurologic problems are among the least common causes of syncope (5%-10%),6,7,33 diagnosis of neurologic dysfunction (eg, from vascular, parenchymal, or electrical etiologies) may require more advanced testing. Imaging, via contrast-enhanced computed tomography or magnetic resonance imaging, carotid or transcranial ultrasonography, and even full electroencephalographic evaluation, may be necessary to uncover potential pathologic entities (eg, cerebrovascular disease, encephalomalacia, epileptic foci).9
Although the vast majority of patients who present with fainting relate a story that points toward a potential diagnosis, clinicians should be mindful of basic and more advanced tools that assist in the work-up of syncope. In summary, fainting results from transient hypoxia to the brain; thus, our goal is to return blood to the brain as soon as possible. Simple maneuvers (such as calling 911, measuring vital signs, giving reassurance) may be sufficient in the immediate aftermath of syncope. However, elevation of the legs and administration of fluids, when appropriate, may help the patient restore perfusion; only when the cause of syncope is clear should further disease-specific treatment be undertaken.
CONCLUSIONS
Fainting, swooning, and syncope (conditions with multiple etiologies) are prevalent and can be problematic. Knowledge of syncope’s predisposing factors and pathophysiologic underpinnings can guide the evaluation. Unfortunately, in approximately 40% of cases (despite an extensive work-up), the specific etiology of syncope remains a mystery. Initial supportive treatment can be followed by disease-specific interventions.
REFERENCES
1. Kapoor WN. Syncope. N Engl J Med. 2000;343(25):1856-1862. PubMed doi:10.1056/NEJM200012213432507
2. Forbes F, ed. The Cyclopaedia of Practical Medicine. Vol 4. London, UK: Sherwood, Gilbert, and Piper; 1835.
3. “Aphorisms” by Hippocrates, written 400 BCE. http://classics.mit.edu/Hippocrates/aphorisms.html. Accessed June 2, 2011.
4. Papavramidou N, Tziakas D. Galen on “syncope.” Int J Cardiol. 2010;142(3):242-244. PubMed doi:10.1016/j.ijcard.2008.12.109
5. Works of art. Esther before Ahasuerus. http://www.metmuseum.org/works_of_art/collection_database/european_paintings/esther_before_ahasuerus_artemisia_gentileschi/objectview.aspx?page=1&sort=6&sortdir=asc&keyword=Esther&fp=1&dd1=11&dd2=0&vw=0&collID=11&OID=110000895&vT=1&hi=0&ov=0. Accessed June 2, 2011.
6. Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347(12):878-885. PubMed doi:10.1056/NEJMoa012407
7. Brignole M, Alboni P, Benditt DG, et al. Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope: update 2004. Europace. 2004;6(6):467-537. PubMed doi:10.1016/j.eupc.2004.08.008
8. Alboni P, Brignole M, Menozzi C, et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001;37(7):1921-1928. PubMed doi:10.1016/S0735-1097(01)01241-4
9. Ammirati F, Colivicchi F, Santini M. Diagnosing syncope in clinical practice: implementation of a simplified diagnostic algorithm in a multicentre prospective trial—the OESIL 2 study (Osservatorio Epidemiologico della Sincope nel Lazio). Eur Heart J. 2000;21(11):935-940. PubMed doi:10.1053/euhj.1999.1910
10. Caplan JP, Rabinowitz T. An approach to the patient with cognitive impairment: delirium and dementia. Med Clin North Am. 2010;94(6):1103-1116, ix [ix.]. PubMed doi:10.1016/j.mcna.2010.08.004
11. Sutton R, Brignole M, Benditt D, et al. The diagnosis and management of syncope. Curr Hypertens Rep. 2010;12(5):316-322. PubMed doi:10.1007/s11906-010-0144-0
12. Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol. 2009;106(1):284-292. PubMed doi:10.1152/japplphysiol.90991.2008
13. Wieling W, Thijs RD, van Dijk N, et al. Symptoms and signs of syncope: a review of the link between physiology and clinical clues. Brain. 2009;132(Pt 10):2630-2642. PubMed doi:10.1093/brain/awp179
14. Thomas HM 3rd, Lefrak SS, Irwin RS, et al. The oxyhemoglobin dissociation curve in health and disease: role of 2,3-diphosphoglycerate. Am J Med. 1974;57(3):331-348. PubMed doi:10.1016/0002-9343(74)90129-6
15. Franco Folino A. Cerebral autoregulation and syncope. Prog Cardiovasc Dis. 2007;50(1):49-80. PubMed doi:10.1016/j.pcad.2007.01.001
16. Vaddadi G, Lambert E, Corcoran SJ, et al. Postural syncope: mechanisms and management. Med J Aust. 2007;187(5):299-304. PubMed
17. Freeman R. Clinical practice: neurogenic orthostatic hypotension. N Engl J Med. 2008;358(6):615-624. PubMed doi:10.1056/NEJMcp074189
18. Grubb BP. Clinical practice: neurocardiogenic syncope. N Engl J Med. 2005;352(10):1004-1010. PubMed doi:10.1056/NEJMcp042601
19. Reed MJ. Management of syncope in the emergency department. Minerva Med. 2009;100(4):259-273. PubMed
20. Kessler C, Tristano JM, De Lorenzo R. The emergency department approach to syncope: evidence-based guidelines and prediction rules. Emerg Med Clin North Am. 2010;28(3):487-500. PubMed doi:10.1016/j.emc.2010.03.014
21. Luzza F, Di Rosa S, Pugliatti P, et al. Syncope of psychiatric origin. Clin Auton Res. 2004;14(1):26-29. PubMed doi:10.1007/s10286-004-0141-y
22. Rasmussen NH, Bernard ME, Harmsen WS. Physical symptoms that predict psychiatric disorders in rural primary care adults. J Eval Clin Pract. 2008;14(3):399-406. PubMed doi:10.1111/j.1365-2753.2007.00879.x
23. Kouakam C, Lacroix D, Klug D, et al. Prevalence and prognostic significance of psychiatric disorders in patients evaluated for recurrent unexplained syncope. Am J Cardiol. 2002;89(5):530-535. PubMed doi:10.1016/S0002-9149(01)02292-5
24. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
25. Simon NM, Fischmann D. The implications of medical and psychiatric comorbidity with panic disorder. J Clin Psychiatry. 2005;66(suppl 4):8-15. PubMed
26. Yardley L, Owen N, Nazareth I, et al. Panic disorder with agoraphobia associated with dizziness: characteristic symptoms and psychosocial sequelae. J Nerv Ment Dis. 2001;189(5):321-327. PubMed doi:10.1097/00005053-200105000-00009
27. Morgan H, Blashki G. Fits, faints and funny turns: could it be a mental disorder? Aust Fam Physician. 2003;32(4):211-213, 216-219. PubMed
28. Leftheriotis D, Michopoulos I, Flevari P, et al. Minor psychiatric disorders and syncope: the role of psychopathology in the expression of vasovagal reflex. Psychother Psychosom. 2008;77(6):372-376. PubMed doi:10.1159/000151517
29. Newton JL, Kenny RA, Baker CR. Cognitive behavioural therapy as a potential treatment for vasovagal/neurocardiogenic syncope: a pilot study. Europace. 2003;5(3):299-301. PubMed doi:10.1016/S1099-5129(03)00030-8
30. Sokolowski CJ, Giovannitti JA Jr, Boynes SG. Needle phobia: etiology, adverse consequences, and patient management. Dent Clin North Am. 2010;54(4):731-744. PubMed doi:10.1016/j.cden.2010.06.012
31. van Dijk JG. Fainting in animals. Clin Auton Res. 2003;13(4):247-255. PubMed doi:10.1007/s10286-003-0099-1
32. Levi M. Vasovagal fainting as an evolutionary remnant of the fight against hemorrhage. Clin Auton Res. 2005;15(2):69-70. PubMed doi:10.1007/s10286-005-0252-0
33. Serrano LA, Hess EP, Bellolio MF, et al. Accuracy and quality of clinical decision rules for syncope in the emergency department: a systematic review and meta-analysis. Ann Emerg Med. 2010;56(4):362-373, e1. PubMed doi:10.1016/j.annemergmed.2010.05.013