Complaints of hypoglycemia resemble the sedative effect of antipsychotics. As such, clinicians may overlook hypoglycemia in patients with psychiatric disorders. Here, a case of hypoglycemia associated with hyperinsulinemia induced by quetiapine in a female patient with bipolar disorder is reported. The case suggests that clinicians should be aware of the potential for hypoglycemia induced by second-generation antipsychotics.
Second-Generation Antipsychotic-Induced Hypoglycemia

ABSTRACT
Complaints of hypoglycemia resemble the sedative effect of antipsychotics. As such, clinicians may overlook hypoglycemia in patients with psychiatric disorders. Here, a case of hypoglycemia associated with hyperinsulinemia induced by quetiapine in a female patient with bipolar disorder is reported. The case suggests that clinicians should be aware of the potential for hypoglycemia induced by second-generation antipsychotics.
Prim Care Companion CNS Disord 2018;20(1):17br02186
To cite: Fujita T, Mizoguchi Y, Kunitake Y, et al. Second-generation antipsychotic-induced hypoglycemia. Prim Care Companion CNS Disord. 2018;20(1):17br02186.
To share: https://doi.org/10.4088/PCC.17br02186
© Copyright 2018 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry, Faculty of Medicine, Saga University, Saga City, Japan
bDepartment of Neuropsychiatry, Faculty of Medicine, Graduate School of Medical Sciences, Kyushu University, Fukuoka City, Japan
*Corresponding author: Akira Monji, MD, Department of Psychiatry, Faculty of Medicine, Saga University, Nabeshima5-1-1, Saga-city 849-8501, Japan ([email protected]).
Quetiapine, a second-generation antipsychotic (SGA), is regularly prescribed for the treatment of psychotic and mood disorders. Quetiapine use is associated with various metabolic side effects, including obesity and diabetes.1-4 SGAs increase risk for type 2 diabetes mellitus, and the proposed mechanism for this development centers on drug-induced weight gain. This mechanism initiates the dysmetabolic cascade of insulin resistance, increases insulin production, and causes pancreatic β cell failure. In SGA-treated patients with drug-induced weight gain, metabolic syndrome, or prediabetes, fasting hyperinsulinemia has been identified as a biomarker of insulin resistance.3,4 Conversely, few reports5-12 have shown treatment with SGAs to be associated with hypoglycemia. Complaints of hypoglycemia resemble the sedative effect of SGAs. As such, clinicians may overlook hypoglycemia in patients with psychiatric disorders. Hypoglycemia can cause seizures, permanent neurologic damage, or death and can also generate symptoms of adrenergic stimulation, such as irritability and anxiety. Recurrent hypoglycemia may lead to cognitive impairment and the onset of dementia.13
We report a case of hypoglycemia associated with hyperinsulinemia induced by quetiapine in a female patient with bipolar disorder. Relevant literature is also reviewed.
CASE REPORT
Ms A is a 62-year-old woman with no personal history of psychiatric or physical illness, including diabetes mellitus. Her family history includes a younger sister with major depressive disorder. She presented to the psychiatry clinic of a university hospital with psychiatric symptoms, including depressed mood, insomnia, appetite loss, and loss of motivation. She began to experience these symptoms at age 61 years and soon became unable to do housework. Initially, dementia was suspected, but neuroimaging and neurocognitive examination revealed no definite abnormalities. She was diagnosed with major depressive disorder (DSM-5 criteria), and duloxetine was prescribed. However, she began to complain of constipation and diarrhea. No definite abnormalities were observed during the gastrointestinal examination. However, appetite loss led to extreme emaciation, and she became unable to walk. She was subsequently admitted to the hospital.

- Complaints of hypoglycemia resemble the sedative effects of antipsychotics.
- Clinicians should be aware of the potential for hypoglycemia induced by second-generation antipsychotics.
Ms A’s fasting blood sugar level at admission was 85 mg/dL. She was initially prescribed mirtazapine 15 mg/day for her depressive symptoms. Her body mass index at admission was 11.8, but she refused to eat. Delirium soon emerged, most likely due to undernutrition, and tube feeding and quetiapine 25 mg/day were started. Laboratory data revealed hypoglycemia with no clinical symptoms immediately after prescription of quetiapine. Therefore, quetiapine was discontinued, and risperidone 0.5 mg/day was prescribed. The patient’s hypoglycemia gradually ameliorated. After 1 month, she began to eat, and tube feeding was stopped. After another month, she began to show hypomanic symptoms, such as talkativeness, mood elevation, grandiosity, and delusions of grandeur. Ms A was diagnosed with bipolar disorder (DSM-5 criteria), and, thus, mirtazapine 15 mg/day was stopped. Lithium 400 mg/day was effective in treating her mood and psychiatric symptoms, which gradually ameliorated within 4 months. Since discontinuation of quetiapine, hypoglycemia has not been observed for a year and 6 months.
DISCUSSION
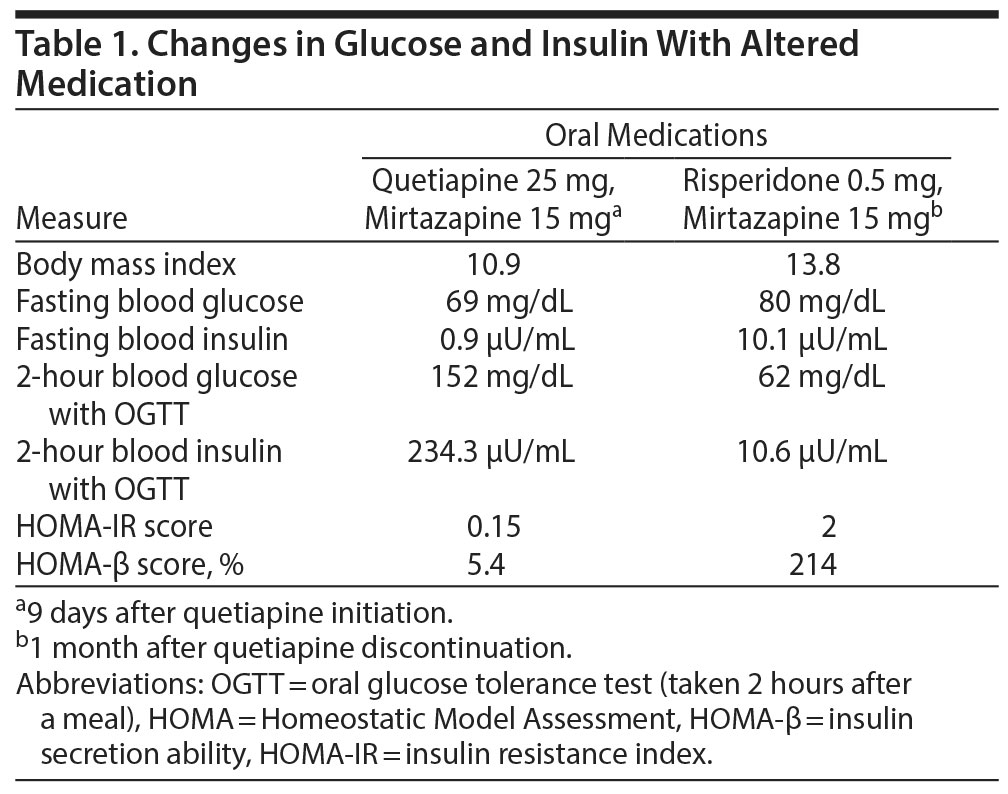
Hypoglycemia observed in the present case appeared immediately after the prescription of quetiapine and disappeared after the switch from quetiapine to risperidone. Therefore, quetiapine seemed to be the cause of hypoglycemia in Ms A. As shown in Table 1, an oral glucose tolerance test (OGTT) revealed remarkable hyperinsulinemia during the administration of quetiapine but not risperidone. Hyperinsulinemia thus seemed to cause persistent hypoglycemia during the administration of quetiapine. The patient’s HOMA-IR14 (Homeostatic Model Assessment-insulin resistance) score remained below 4, indicating no insulin resistance. It has been reported that hyperinsulinemia can lead to an increased and more rapid feeling of satiety in anorexia nervosa and depression.13 Increased suppression of serum ghrelin concentration by hyperinsulinemia in women with anorexia has also been reported.15 These results may account for severe appetite loss during the administration of quetiapine. A decreased level of HOMA-β may be attributable to a low nutritional state due to severe appetite loss during the administration of quetiapine. A switch to risperidone resulted in the increase of HOMA-β and appetite promotion in the present case.
Hypoglycemia Induced by Second-Generation Antipsychotics
Suzuki et al5 reported 3 cases of hypoglycemia induced by SGAs (quetiapine, risperidone, and olanzapine) in nondiabetic patients with schizophrenia. Researchers6 also reported a case of hypoglycemia induced by quetiapine in a patient with schizophrenia that improved after a switch to blonanserin, another SGA. Watanabe et al7 reported a case of hypoglycemia induced by dumping syndrome following surgery for gastric cancer in a patient with schizophrenia treated with olanzapine. Mondal et al8 reported oral aripiprazole-induced hypoglycemia in a case of psychosis with Parkinson’s disease. In their case,8 dechallenge and rechallenge with aripiprazole confirmed the close relationship between administration of aripiprazole and onset of hypoglycemic events. Haruta et al9 reported a case of olanzapine-induced hypoglycemia in anorexia nervosa. In their case,9 hyperinsulinemia was associated with hypoglycemia as seen in our patient. Omi et al10 reported a case of hypoglycemia associated with hyperinsulinemia induced by paliperidone in a patient with schizophrenia. Nagamine11 reported 3 cases of hypoglycemia associated with insulin hypersecretion following the addition of olanzapine to conventional antipsychotics in a patient with schizophrenia. Rowe et al12 reported a case of neonatal hypoglycemia following maternal olanzapine therapy during pregnancy in a patient with bipolar disorder.
Although van Winkel and De Hert16 demonstrated that there was little evidence that SGAs induce reactive hypoglycemia, the number of reports5-12 on hypoglycemia induced by SGAs has increased. There are several hypotheses on how SGAs induce hypoglycemia.10 The secretion of insulin by pancreatic β cells might be enhanced by atypical antipsychotics and consequently cause hypoglycemia, while SGAs seem to differ in their effect on insulin release in vitro.17,18 SGAs might antagonize muscarinic receptors so that insulin secretion continues after glucose levels return to normal, leading to hypoglycemia. Some studies19 also reported that SGAs significantly reduce glucose levels through induction of insulin release, and the effects might be caused by its potent antagonistic activity against α2-adrenoceptors. Patients with severe emaciation, as seen in the present case, can easily develop hypoglycemia because of deficient stored glucose levels.9,11
CONCLUSION
Complaints of hypoglycemia resemble the sedative effect of antipsychotics. As such, clinicians may overlook hypoglycemia in patients with psychiatric disorders. The present case suggests that, as clinicians, we should bear in mind the potential for hypoglycemia induced by antipsychotics.
Submitted: June 27, 2017; accepted September 18, 2017.
Published online: January 25, 2018.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Permission was received from the patient to publish this case, and the information was de-identified to protect anonymity.
REFERENCES
1. Chen CH, Lin TY, Chen TT, et al. A prospective study of glucose homeostasis in quetiapine-treated schizophrenic patients by using the intravenous glucose tolerance test. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(4):965-969. PubMed CrossRef
2. Koller EA, Jena Weber J, Doraiswamy PM, et al. A survey of reports of quetiapine-associated hyperglycemia and diabetes mellitus. J Clin Psychiatry. 2004;65(6):857-863. PubMed CrossRef
3. Manu P, Correll CU, Van Winkel R, et al. Prediabetes in patients treated with antipsychotic drugs. J Clin Psychiatry. 2012;73(04):460-466. PubMed CrossRef
4. Manu P, Correll CU, Wampers M, et al. Insulin secretion in patients receiving clozapine, olanzapine, quetiapine and risperidone. Schizophr Res. 2013;143(2-3):358-362. PubMed CrossRef
5. Suzuki Y, Watanabe J, Fukui N, et al. Hypoglycemia induced by second-generation antipsychotic agents in schizophrenic nondiabetic patients. BMJ. 2009;338: a1792. PubMed
6. Suzuki Y, Sugai T, Watanabe J, et al. Improvement in quetiapine-induced hypoglycemia following a switch to blonanserin. Psychiatry Clin Neurosci. 2012;66(4):370-371. PubMed CrossRef
7. Watanabe A, Fukui N, Suzuki Y, et al. Improvement of dumping syndrome and oversecretion of glucose-dependent insulinotropic polypeptide following a switch from olanzapine to quetiapine in a patient with schizophrenia. Gen Hosp Psychiatry. 2015;37(4):372.e5. PubMed CrossRef
8. Mondal S, Saha I, Das S, et al. Oral aripiprazole-induced severe hypoglycemia. Ther Drug Monit. 2012;34(3):245-248. PubMed CrossRef
9. Haruta I, Asakawa A, Inui A. Olanzapine-induced hypoglycemia in anorexia nervosa. Endocrine. 2014;46(3):672-673. PubMed CrossRef
10. Omi T, Riku K, Fukumoto M, et al. Paliperidone-induced hypoglycemia by increasing insulin secretion [published online ahead of print July 10, 2016]. Case Rep Psychiatry. 2016: 1805414. PubMed
11. Nagamine T. Hypoglycemia associated with insulin hypersecretion following the addition of olanzapine to conventional antipsychotics. Neuropsychiatr Dis Treat. 2006;2(4):583-585. PubMed CrossRef
12. Rowe M, Gowda BA, Taylor D, et al. Neonatal hypoglycemia following maternal olanzapine therapy during pregnancy. Ther Adv Psychopharmacol. 2012;2(6):265-268. PubMed CrossRef
13. Licinio-Paixao J. Hyperinsulinemia: a mediator of decreased food intake and weight loss in anorexia nervosa and major depression. Med Hypotheses. 1989;28(2):125-130. PubMed CrossRef
14. Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21(12):2191-2192. PubMed doi:10.2337/diacare.21.12.2191
15. Karczewska-Kupczewska M, Straczkowski M, Adamska A, et al. Increased suppression of serum ghrelin concentration by hyperinsulinemia in women with anorexia. Eur J Endocrinol. 2010;162(2):235-239. PubMed CrossRef
16. van Winkel R, De Hert M. Reactive hypoglycemia in severe mental illness. BMJ. 2009;338:b2536. PubMed
17. Melkersson K, Jansson E. The atypical antipsychotics quetiapine, risperidone and ziprasidone do not increase insulin release in vitro. Neuroendocrinol Lett. 2005;26:205-208. PubMed
18. Ngai YF, Sabatini P, Nguyen D, et al. Quetiapine treatment in youth is associated with decreased insulin secretion. J Clin Psychopharmacol. 2014;34(3):359-364. PubMed CrossRef
19. Savoy YE, Ashton MA, Miller MW, et al. Differential effects of various typical and atypical antipsychotics on plasma glucose and insulin levels in the mouse: evidence for the involvement of sympathetic regulation. Schizophr Bull. 2010;36(2):410-418. PubMed CrossRef
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top