Because this piece does not have an abstract, we have provided for your benefit the first 3 sentences of the full text.
The exclusion of psychosis secondary to a neurosurgical condition is mandatory whenever a psychiatric diagnosis is made. Meningiomas can cause psychiatric symptoms in up to 35% of patients, especially when localized in the frontal lobe and in correlation with edema. Frontal lobe meningiomas are known to cause not only mood changes but also florid psychotic syndromes, thus they should always be part of the differential diagnosis for both affective and nonaffective psychosis.

Left Frontal Lobe Meningioma Causing Secondary Schizophrenia Misdiagnosed for 25 Years
The exclusion of psychosis secondary to a neurosurgical condition is mandatory whenever a psychiatric diagnosis is made. Meningiomas can cause psychiatric symptoms in up to 35% of patients, especially when localized in the frontal lobe1 and in correlation with edema.2 Frontal lobe meningiomas are known to cause not only mood changes3 but also florid psychotic syndromes,4-11 thus they should always be part of the differential diagnosis for both affective and nonaffective psychosis. Unfortunately, many patients receive the diagnosis of primary psychosis (eg, schizophrenia spectrum disorder) without proper exclusion of a brain lesion. Here, the case is presented of a patient who had been labeled for a quarter of a century with the diagnosis of various primary psychotic disorders until the first neuroimaging examination revealed a large-sized left frontal lobe meningioma.
Case Report
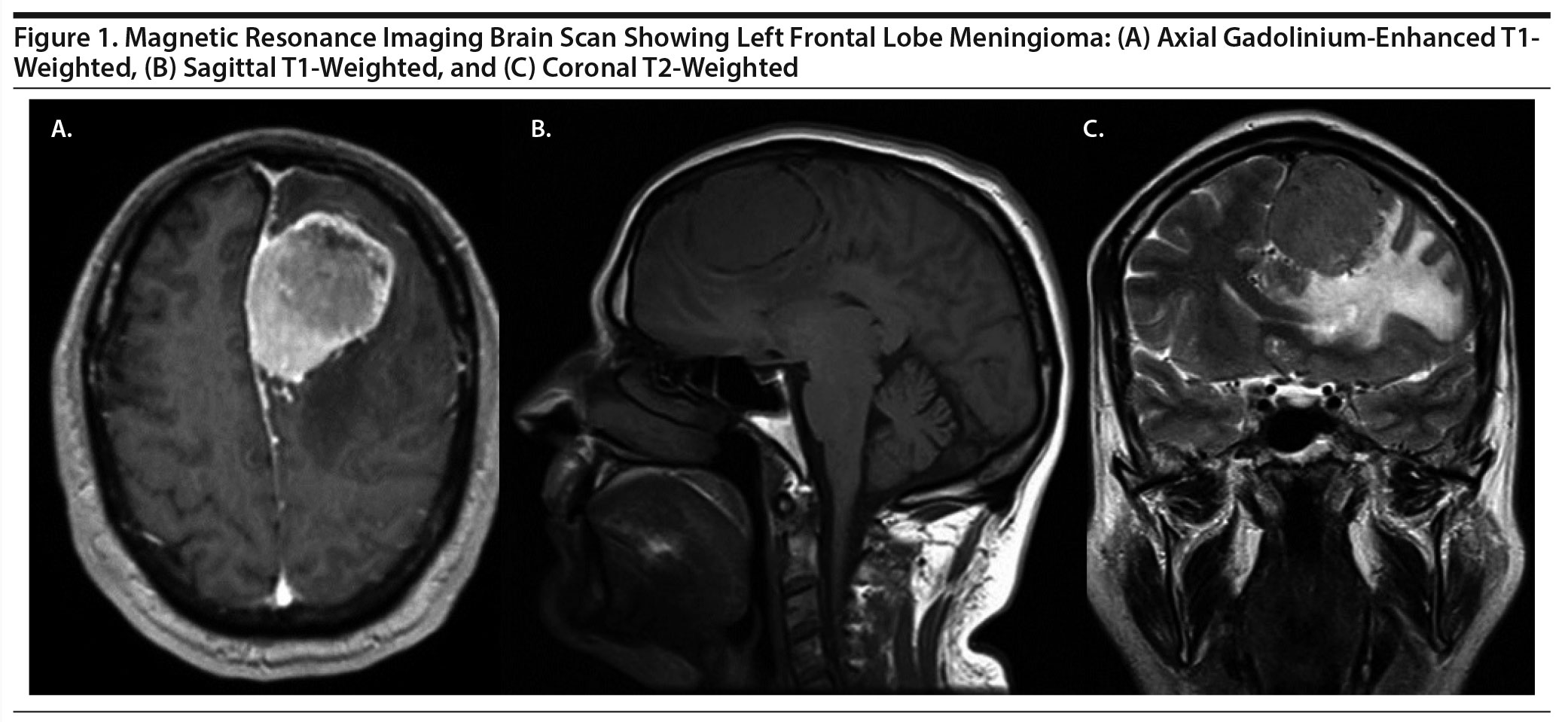
A 49-year-old man was admitted to the psychiatric emergency department of a general hospital for aggressive behavior and social isolation secondary to persecutory delusional ideation. His extensive clinical records revealed 15 psychiatric admissions over the last 25 years. There were various episodes of nonaffective (persecutory delusions with auditory pseudohallucinations) and affective psychotic episodes (mania and depression), suggesting a schizophrenia or schizoaffective spectrum disorder. The patient had been on many benzodiazepines, antidepressants, mood stabilizers, and antipsychotics and was successful in occupational therapy. He had lost his father in a workplace accident at 13 years of age and since then became introverted and emotionally dependent on his histrionic mother. He had a family history of stroke (paternal grandmother) and alcoholism and schizophrenia (maternal grandfather and uncle). His blood and urine tests were negative. The psychological assessment documented superior intelligence with intellectual snobbery, learning and memory impairments, and an immature and impulsive personality, with a particular interest in sexual and religious themes. Although 1 electroencephalogram was mildly irregular, no brain scans were included in the hundreds of pages of his clinical file. A routine magnetic resonance imaging (MRI) brain scan (Figure 1) showed a left frontal lobe extra axial expansive lesion with well-defined limits (47 ×— 46 ×— 57 mm) suggestive of cerebral falx meningioma. The patient was referred to the neurosurgery department, and neuropathology confirmed a grade II meningioma. His aggression and social isolation remitted during the next 2 years of postsurgical follow-up, but there was no full remission of previously described (older) psychotic symptoms. Psychopharmacologic treatment was reintroduced with escitalopram 20 mg (morning), clozapine 100 mg (evening), and paliperidone palmitate 350 mg (1 injection every 3 months).
Discussion
For decades, psychiatrists trusted in Schneiderian first-rank symptoms (eg, delusional perceptions and complex hallucinations) as pathognomonic and sufficient for schizophrenia diagnosis.12 Nevertheless, systematic review revealed that those symptoms may lead to 40% of schizophrenia diagnosis failure.13 On the other hand, it is important to remember that these symptoms can occur in many other disorders, especially neurologic conditions.14
Many meningiomas are slow-growing neoplasms.15 Therefore, the patient presented here most likely suffered a sluggish sequence of events involving the local neurocircuits in relation with the compression over the frontal lobes, leading to many different psychiatric symptoms for more than 2 decades, including social isolation and aggressive behavior. In this particular case, we will never know how old the lesion was or if the prognosis would have been different had a brain scan been done earlier.
Unfortunately, this was not the first (or even second) patient to present to this hospital with a serious psychiatric misdiagnosis and no previous brain-imaging examination.16-20 Every case of first-episode psychosis deserves a full medical workup,21,22 and physicians should ask themselves: Why in the age of MRIs is a brain tumor mistaken for a psychiatric illness?23 Awareness of secondary schizophrenia should be raised24,25 to minimize diagnosis errors that may compromise treatment and prognosis.
Published online: February 27, 2020.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Permission was obtained from the patient to publish this case report, and information was de-identified to protect anonymity.
REFERENCES
1.Bommakanti K, Gaddamanugu P, Alladi S, et al. Pre-operative and post-operative psychiatric manifestations in patients with supratentorial meningiomas. Clin Neurol Neurosurg. 2016;147:24-29. PubMed CrossRef
2.Lampl Y, Barak Y, Achiron A, et al. Intracranial meningiomas: correlation of peritumoral edema and psychiatric disturbances. Psychiatry Res. 1995;58(2):177-180. PubMed CrossRef
3.Madhusoodanan S, Opler MG, Moise D, et al. Brain tumor location and psychiatric symptoms: is there any association? a meta-analysis of published case studies. Expert Rev Neurother. 2010;10(10):1529-1536. PubMed CrossRef
4.Hunter R, Blackwood W, Bull J. Three cases of frontal meningiomas presenting psychiatrically. BMJ. 1968;3(5609):9-16. PubMed CrossRef
5.Sengstaken EA, King SA. Chronic schizophrenia or meningioma? J Am Board Fam Pract. 1994;7(1):71-73. PubMed
6.Kaur D, Ajinkya S, Nabi J, et al. Meningioma masquerading as acute psychosis with symptoms of schizophrenia. Bombay Hosp J. 2012;54(2):316-318.
7.Coetzer R. Auditory hallucinations secondary to a right frontal meningioma. J Neuropsychiatry Clin Neurosci. 2014;26(3):E15. PubMed CrossRef
8.Jahangard L, Ghaleiha A, Haghighi M, et al. Musical hallucination in a patient with frontal lobe meningioma. Avicenna J Neuro Psych Physio. 2014;1(1):E20156. CrossRef
9.Maia-de-Oliveira JP, Brasileiro LE, Correia CE, et al. Psychotic syndrome secondary to meningioma treated with a low dose of olanzapine. Br J Psychiatry. 2015;37(2):179-180. PubMed CrossRef
10.Madhusoodanan S, Patel S, Reinharth J, et al. Meningioma and psychiatric symptoms: a case report and brief review. Ann Clin Psychiatry. 2015;27(2):126-133. PubMed
11.Moyal D, Garg A. Meningioma in an elderly presenting as psychosis: a case report. Clinical Cancer Drugs. 2017;4(1):65-68. CrossRef
12.Heinz A, Voss M, Lawrie SM, et al. Shall we really say goodbye to first rank symptoms? Eur Psychiatry. 2016;37:8-13. PubMed CrossRef
13.Soares-Weiser K, Maayan N, Bergman H, et al. First rank symptoms for schizophrenia. Cochrane Database Syst Rev. 2015;1:CD010653. PubMed
14.Marneros A. Schizophrenic first-rank symptoms in organic mental disorders. Br J Psychiatry. 1988;152(5):625-628. PubMed CrossRef
15.Zeidman LA, Ankenbrandt WJ, Du H, et al. Growth rate of non-operated meningiomas. J Neurol. 2008;255(6):891-895. PubMed CrossRef
16.Gama Marques J. Psychotic polyembolokoilamania secondary to left parietal lobe glioblastoma. Acta Neurol Belg. 2019;119(2):279-280. PubMed CrossRef
17.Gama Marques J. Brain metastasis affecting frontal lobe misdiagnosed as bipolar disorder, without any neuroimaging exam: two case reports with fatal outcomes. CNS Spectr. 2019;24(2):229-230. PubMed CrossRef
18.Gama Marques J. Twenty years of misdiagnosis of schizophrenia in a patient with Dandy-Walker variant syndrome. Gen Psychiatr. 2019;32(1):e100031. PubMed CrossRef
19.Gama Marques J, Saraiva S, Brissos S. Frontotemporal dementia mimicking bipolar affective disorder, normal pressure hydrocephalus and Klüver-Bucy syndrome. Asian J Psychiatr. 2015;18:106-107. PubMed CrossRef
20.Gama-Marques J, Palhav×£ F, Brissos S. Subarachnoid hemorrhage misdiagnosed as adjustment disorder. Br J Psychiatry. 2015;37(1):81. PubMed CrossRef
21.Freudenreich O, Schulz SC, Goff DC. Initial medical work-up of first-episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3(1):10-18. PubMed CrossRef
22.Falkai P. Differential diagnosis in acute psychotic episode. Int Clin Psychopharmacol. 1996;11(suppl 2):13-17. PubMed CrossRef
23.Caruso R, Piro A. Why in the age of CT scans and MRIs is a brain tumour mistaken for a psychiatric illness? BMJ Case Rep. 2017;2017:bcr-2017-220131. PubMed CrossRef
24.Hambidge D. Secondary schizophrenia. PLoS Med. 2005;2(9):e279, author reply e300. PubMed CrossRef
25.Gama Marques J. Raising awareness about secondary schizophrenia [article in Portuguese]. Acta Med Port. 2019;32(2):169. PubMed CrossRef
aHospital Júlio de Matos, Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal
bClínica Universitária de Psiquiatria e Psicologia Médica, Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal
*Corresponding author: João Gama Marques, MD, Hospital Júlio de Matos, Avenida do Brasil, 53, 1749-002 Lisbon, Portugal ([email protected]).
Prim Care Companion CNS Disord 2020;22(2):19l02466
To cite: Gama Marques J. Left frontal lobe meningioma causing secondary schizophrenia misdiagnosed for 25 years. Prim Care Companion CNS Disord. 2020;22(2):19l02466.
To share: https://doi.org/10.4088/PCC.19l02466
© Copyright 2020 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top