Prim Care Companion CNS Disord 2022;24(5):21cr03114
To cite: Mota-da-Silva D, Estalagem AP, Teles C, et al. Multiple violent suicide attempts in a not so depressed, not so psychotic patient: a diagnostic challenge. Prim Care Companion CNS Disord. 2022;24(5):21cr03114.
To share: https://doi.org/10.4088/PCC.21cr03114
© 2022 Physicians Postgraduate Press, Inc.
aDepartment of Psychiatry and Mental Health, Centro Hospitalar e Universitário do Algarve, Portimão, Portugal
*Corresponding author: Diogo Mota-da-Silva, MD, Department of Psychiatry and Mental Health, Centro Hospitalar e Universitário do Algarve, Sítio do Poço Seco, 8500-338 Portimão, Portugal ([email protected]).
Violent suicide is generally defined by method. Strangulation, firearm or deep blade wounds, fall from significant heights, or vehicle collision are examples of violent suicidal behavior, as opposed to medication or substance poisoning, which are usually regarded as nonviolent.1 The multitude of comorbid conditions, personality traits, and psychosocial factors motivating suicide may pose diagnostic and management challenges. We present the case of a middle aged African-Portuguese man admitted to the inpatient psychiatry unit after attempting suicide by repeatedly stabbing himself in the neck and abdomen.
Case Report
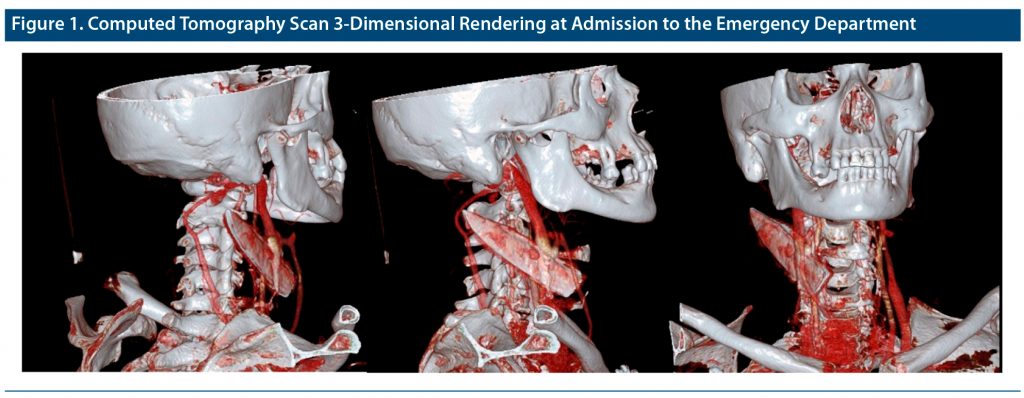
A 50-year-old man presented to the emergency department (ED) displaying multiple self-inflicted penetrating wounds in his neck and abdomen and a kitchen knife lodged within cervical muscular tissues and tendons. Radiologic study identified an internal jugular vein lesion (Figure 1), prompting urgent intervention by vascular and plastic reconstructive surgery. After stabilization, a psychiatric evaluation was conducted.
The patient’s history revealed a depressive syndrome for the last 2 months, which he associated with financial struggles. He described this event as unpremeditated, unrelated with any trigger or stressor event, and unpreceded by alcohol or substance intake, yet with a clear suicidal intention. We found 2 previous attempts: jumping out of a window of his fourth floor flat 5 years ago, from which physical sequelae limited his ability to work and forced him into early retirement and subsequent financial hardship, and deliberate benzodiazepine intoxication 2 years ago. He denied chronic suicidal ideation, instead referring to a “momentary urge to do it.”
The history also revealed brief self-limited psychotic experiences (hallucinatory commanding voices saying, “do it, do it, do it” and calling his name) that he had experienced intermittently for 7 years but that were not present during our assessment or during the current suicidal behavior. The patient’s wife confirmed a history of heavy drinking for 25 years, which he disregarded, and transient persecutory and infidelity delusions associated with periods of increased alcohol consumption.
However, he had received no prior psychiatric or addiction treatment. There was no family history of psychiatric illness or suicide, and he reported no adverse childhood experiences or adulthood trauma. On admission, a full workup including laboratory evaluation, cerebral magnetic resonance imaging, and the Montreal Cognitive Assessment2 revealed no pathological findings.
A dual diagnosis of major depressive episode of moderate severity (ICD-10 code F32.1) and alcohol-induced psychosis (ICD-10 code F10.259) was proposed. Despite impulsivity manifestations, diagnostic criteria for personality disorder, attention-deficit/hyperactivity disorder, and impulse control disorders were not met.
Treatment with sertraline and lorazepam and psychotherapy interventions to gain insight into his substance abuse and motivation for avoidance produced significant clinical improvement. He maintained clinical remission and alcohol abstinence at discharge and follow-up.
Discussion
In this case, depressive and psychotic symptoms were not sustained or severe enough to fulfill criteria for a severe depressive episode with psychotic characteristics or a primary psychotic disorder, while the robust association between psychopathology and alcohol intake indicated an evolving dual diagnosis. Furthermore, all his suicide attempts were carried out with various methods and levels of lethality and violence, suggesting an association with impulsivity and low tolerance to frustration traits, but also an important role of access to different means.
Recognition of violent attempts as a poor prognosis factor is well established.3 Numerous factors such as male sex, history of mental illness,4–6 substance abuse,7,8 and impulsivity and aggressiveness traits,9 but also genetic polymorphisms,10,11 altered serotoninergic neurotransmission,1 and metabolic syndrome1,12 appear to be correlated with violent suicide attempts. In the interest of prevention, expanding and translating this knowledge into clinical guidelines and public health interventions is paramount for an evidence-based approach to suicidality.
Published online: August 30, 2022.
Relevant financial relationships: None.
Funding/support: None.
Patient consent: The patient provided consent to publish this case report, and information has been de-identified to protect anonymity.
References (12)

- Ludwig B, Dwivedi Y. The concept of violent suicide, its underlying trait and neurobiology: a critical perspective. Eur Neuropsychopharmacol. 2018;28(2):243–251. PubMed CrossRef
- Freitas S, Simões MR, Martins C, et al. Estudos de adaptação do Montreal Cognitive Assessment (MoCA) para a população portuguesa. (Montreal Cognitive Assessment (MoCA): Portuguese adaptation studies) Aval Psicol. 2008;9(3):345–357.
- Runeson B, Tidemalm D, Dahlin M, et al. Method of attempted suicide as predictor of subsequent successful suicide: national long term cohort study. BMJ. 2010;341(jul13 1):c3222. PubMed CrossRef
- Fico G, Caivano V, Zinno F, et al. Affective temperaments and clinical course of bipolar disorder: an exploratory study of differences among patients with and without a history of violent suicide attempts. Medicina (Kaunas). 2019;55(7):E390. PubMed
- Stenbacka M, Jokinen J. Violent and non-violent methods of attempted and completed suicide in Swedish young men: the role of early risk factors. BMC Psychiatry. 2015;15(1):196. PubMed CrossRef
- Persett PS, Grimholt TK, Ekeberg O, et al. Patients admitted to hospital after suicide attempt with violent methods compared to patients with deliberate self-poisoning: a study of background variables, somatic and psychiatric health and suicidal behavior. BMC Psychiatry. 2018;18(1):1–10. PubMed CrossRef
- Ilgen MA, Conner KR, Valenstein M, et al. Violent and nonviolent suicide in veterans with substance-use disorders. J Stud Alcohol Drugs. 2010;71(4):473–479. PubMed CrossRef
- Sørensen EH, Thorgaard MV, Østergaard SD. Male depressive traits in relation to violent suicides or suicide attempts: a systematic review. J Affect Disord. 2020;262:55–61. PubMed CrossRef
- Dumais A, Lesage AD, Lalovic A, et al. Is violent method of suicide a behavioral marker of lifetime aggression? Am J Psychiatry. 2005;162(7):1375–1378. PubMed CrossRef
- Bayle FJ, Leroy S, Gourion D, et al. 5HTTLPR polymorphism in schizophrenic patients: further support for association with violent suicide attempts. Am J Med Genet B Neuropsychiatr Genet. 2003;119B(1):13–17. PubMed CrossRef
- Peñas-Lledó E, Guillaume S, Delgado A, et al. ABCB1 gene polymorphisms and violent suicide attempt among survivors. J Psychiatr Res. 2015;61:52–56. PubMed CrossRef
- Rosso G, Albert U, Bramante S, et al. Correlates of violent suicide attempts in patients with bipolar disorder. Compr Psychiatry. 2020;96:152136. PubMed CrossRef
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top