Trichotillomania (TTM), also known as hair pulling disorder, is characterized by the recurrent urge to pull one’s own hair. It is included in obsessive-compulsive disorder and other related disorders of the DSM-5.1 TTM onset is often reported in adolescents.2,3 Its prevalence in the community is reported to be between 0.5% and 2%.4 Onset at < 6 years of age is categorized as very early onset and accounts for less than 5% of total cases of TTM.5 Although female preponderance is reported in adults, it is unclear in the pediatric population. On most occasions, pediatricians, primary care physicians, or dermatologists are the first levels of contact with the hospital before psychiatrists. We report rare cases of very early onset TTM and its management difficulties.
Case 1
A 2.5-year-old girl was referred to the psychiatry outpatient clinic of a tertiary care hospital from the department of dermatology with complaints of an intense urge to twist and pull her hair since infancy. A month ago, her parents started noticing a bald patch over the left side of her scalp. They reported that her hair-pulling behavior increased when she was left alone to play or was unengaged. It was noted that, on all occasions, she would raise her hands to her head and start twisting the hair before pulling it forcefully. About 6 months ago, the parents started finding strands of hair in the child’s hands and noticed she would pull her hair with force. When they tried to take her hand away from her hair, she would cry instantly and would settle or be pacified only when she was left free to continue the behavior. Family members tried to reduce the behavior by physically restraining her hands with a handkerchief and covering her head with a cap, but most of these efforts were futile. There was no history suggestive of plucking hair in other parts of the body or eating plucked hair or any abdominal complaints. Thumb sucking and intermittent anger outburst were reported whenever she was stopped verbally or scolded. The child would throw her toys and break things if interrupted while playing with her hair.
The mother reported that the antenatal, natal, and perinatal periods were uneventful and denied exposure to any drugs or radiation during pregnancy. The patient was born full term via normal vaginal hospital delivery and cried immediately at birth. Her developmental milestones were appropriate, and she was immunized as recommended for her age. She had left hand dominance, belonged to a Muslim nuclear family of middle socioeconomic status, and lived in a metropolitan city with her parents. There was no history suggestive of comorbid depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder, or sibling rivalry. No significant family history was suggestive of psychiatric illness.
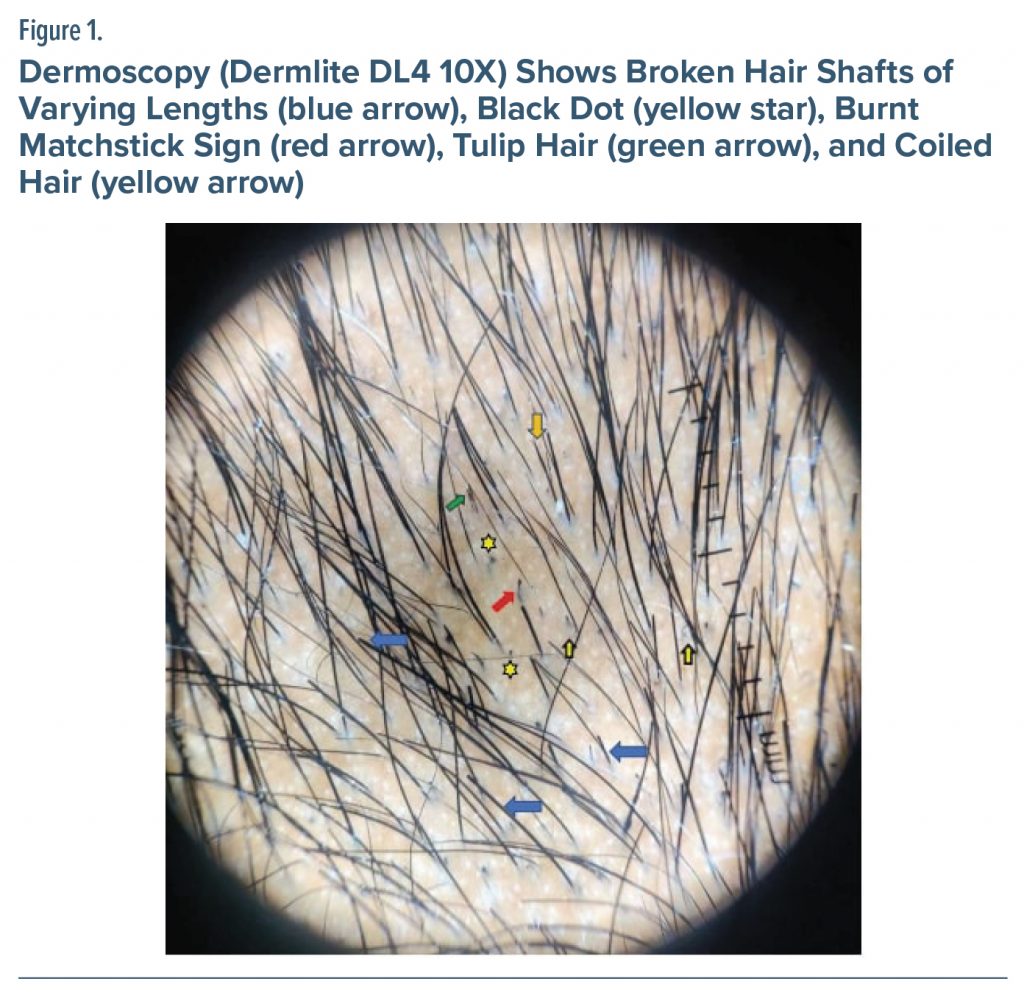
On general examination, an 8 x 8–cm bald patch over the left scalp was noted (Figure 1). No other significant physical or neurologic examination findings were reported in the pediatric consultation. During behavioral observation (done serially by doctors and nursing staff), the child was uncooperative when staff tried to talk with her about the hair pulling. She engaged in playing with toys and indulged in hair pulling when alone and would scream and at times cry when stopped from this behavior. Her speech was appropriate for her age, her affect was euthymic, and she expressed an intense urge to pull her hair. Her attention span was sustained, intellectual capacity was normal, and she acknowledged the problem behavior. Dermatology consultation was obtained to rule out other causes of patchy alopecia (alopecia areata, noninflammatory tinea capitis). Skin, nails, and mucosa were normal, and the hair pull test was negative. Frequency of hair pulling was decreased when started on syrup valproate 100 mg/d.
Case 2
A 3-year-old, right-handed Hindu girl of middle socioeconomic status was referred from the pediatric outpatient unit to the psychiatry outpatient unit with a bald patch over the right parietotemporal region. History revealed that the child started pulling her hair at 2 years of age, and the behavior had increased over time. History of eating sand was also reported by her parents. Pulling was frequent when the child was idle and decreased with distraction. Her parents were unsuccessful in preventing the habit by punishments. Although the child would not cry when her hands were removed from her hair, she would automatically take her hand to the head when the hands were set free. Her parents tried to stop the behavior by having the child wear a cap and cutting the hair short. Although the behavior was reduced when the hair was cut short, it recurred as the length of the hair increased. There was no history of plucking hair in other parts of the body or eating plucked hair or any abdominal complaints. Thumb sucking was reported. The prenatal and postnatal period had been uneventful, and she was delivered full term via normal vaginal delivery, with no complications reported during infancy. The child’s developmental milestones were appropriate, and she was immunized as recommended for her age. Hemoglobin was 10.2 g/dL, and mean corpuscular volume was 75 fL. No other remarkable findings were reported on examination or in any investigations or pediatric or dermatology consultations apart from an 8 x 8–cm bald patch over the right scalp. No history was suggestive of other comorbidity. Anemia was diagnosed, and hematinics were given to the patient. Nonpharmacologic interventions of distraction, rewarding desirable behaviors, engaging the child in both indoor and outdoor sports, healthy nutritious diet, and habit reversal measures were advised for both patients.
Discussion
In this report, we highlight the very early onset of TTM. Scalp lesions in such a young age group are often not detected, and these children miss out on receiving treatment interventions. As available psychopharmacologic/psychological interventions are limited, a multidisciplinary approach is required involving dermatologists, pediatricians, and psychiatrists. Clinical presentation of childhood and adolescent TTM may vary in hair-pulling sites, but there is no difference in phenomenology, comorbidity, functional impact, and perceived treatment response.5 A hereditary component should be ruled out in toddlers who present with TTM. Evidence from family and twin studies report that a genetic factor (SAPAP3 gene) plays a significant role in TTM.6 Management is complicated, as the medications proved to be efficacious in adults are not approved for use in children. For instance, literature supports the use of fluoxetine, clomipramine, olanzapine, and N-acetylcysteine in the management of TTM in adults, but there is limited evidence for its use in children.7 This lack of evidence narrows down the management to solely focus on nonpharmacologic/psychological intervention in toddlers. There is some evidence for the use of behavior therapy in the management of TTM in children and adolescents.8 Pharmacotherapy is recommended only when a patient presents with comorbidities, poor or partial response to psychological intervention, and poor insight.9 Research has shown that sleep hygiene intervention could reduce the hair-pulling behavior.10 In addition, other comorbid psychiatric conditions like ADHD, depression, anxiety disorders, obsessive-compulsive disorder, and autistic spectrum disorder should be promptly managed. In a study11 that included more than 10,000 subjects, natural recovery in lifetime diagnosis of TTM was associated with significantly low rates of comorbidity.
Article Information
Published Online: August 15, 2023. https://doi.org/10.4088/PCC.22cr03426
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2023;25(4):22cr03426
Submitted: September 29, 2022; accepted January 20, 2023.
To Cite: Srivastava S, Nandakumar D, Khakha R, et al. Rare cases of trichotillomania in toddlers. Prim Care Companion CNS Disord. 2023;25(4):22cr03426.
Author Affiliations: University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India (all authors).
Corresponding Author: Shruti Srivastava, MBBS, DNB, MNAMS, Department of Psychiatry, Room No. 719, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi 110095, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Patient Consent: Consent was obtained from the legal guardians of the patients to publish the case reports, and information has been de-identified to protect anonymity.
References (11)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. Arlington, VA: American Psychiatric Publishing; 2013.
- Ricketts EJ, Snorrason I, Kircanski K, et al. A latent profile analysis of age of onset in trichotillomania. Ann Clin Psychiatry. 2019;31(3):169–178. PubMed
- Grant JE, Dougherty DD, Chamberlain SR. Prevalence, gender correlates, and co-morbidity of trichotillomania. Psychiatry Res. 2020;288:112948. PubMed CrossRef
- Grant JE, Chamberlain SR. Trichotillomania. Am J Psychiatry. 2016;173(9):868–874. PubMed CrossRef
- Flessner CA, Lochner C, Stein DJ, et al. Age of onset of trichotillomania symptoms: investigating clinical correlates. J Nerv Ment Dis. 2010;198(12):896–900. PubMed CrossRef
- Chattopadhyay K. The genetic factors influencing the development of trichotillomania. J Genet. 2012;91(2):259–262. PubMed CrossRef
- Hoffman J, Williams T, Rothbart R, et al. Pharmacotherapy for trichotillomania. Cochrane Database Syst Rev. 2021;9(9):CD007662. PubMed CrossRef
- Franklin ME, Zagrabbe K, Benavides KL. Trichotillomania and its treatment: a review and recommendations. Expert Rev Neurother. 2011;11(8):1165–1174. PubMed CrossRef
- Torales J, Ruiz Díaz N, Ventriglio A, et al. Hair-pulling disorder (Trichotillomania): etiopathogenesis, diagnosis and treatment in a nutshell. Dermatol Ther (Heidelb). 2021;34(1):e13466. PubMed CrossRef
- Fodstad JC, Greve KT, Curtin MJ, et al. Treatment of typically developing toddlers with hair-pulling behavior and concurrent poor sleep hygiene: a case series. J Dev Behav Pediatr. 2021;42(8):677–681. PubMed CrossRef
- Grant JE, Chamberlain SR. Natural recovery in trichotillomania. Aust N Z J Psychiatry. 2022;56(10):1357–1362. CrossRef
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top