The Psychiatric Consultation Service at Massachusetts General Hospital (MGH) sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Dr Lokko is a third-year resident in the Massachusetts General Hospital/McLean Hospital Psychiatry Residency Training Program and a clinical fellow in psychiatry at Harvard Medical School, Boston, Massachusetts. Dr Stern is chief of the Avery D. Weisman Psychiatry Consultation Service at Massachusetts General Hospital and the Ned H. Cassem professor of psychiatry in the field of psychosomatic medicine/consultation at Harvard Medical School, Boston, Massachusetts.
Dr Stern is an employee of the Academy of Psychosomatic Medicine, has served on the speaker’s board of Reed Elsevier, is a stock shareholder in WiFiMD (Tablet PC), and has received royalties from Mosby/Elsevier and McGraw Hill. Dr Lokko reports no conflict of interest related to the subject of this article.
Regression: Diagnosis, Evaluation, and Management
Have you ever treated an adult patient who was acting like a child? Has one of your patients thrown a temper tantrum when he or she was under distress? Have you wondered what could have caused such behavior and how it should be managed? If you have, then this article should prove useful when creating a differential diagnosis and managing regression.
CASE VIGNETTE
Ms A, a 26-year-old woman with panhypopituitarism (complicated by diabetes mellitus, gastroparesis, diabetes insipidus, and hypothyroidism) and schizoaffective disorder (with a history of inpatient psychiatric admissions) was admitted to a general hospital for worsening agitation, auditory hallucinations, and an inability to perform activities of daily living (eg, feeding, toileting, and grooming). Her preliminary evaluation and laboratory workup were unremarkable for acute medical problems.
During the psychiatric evaluation, Ms A repeatedly banged her head on her pillow (while clutching a stuffed animal) and endorsed auditory hallucinations that accused her of murder. She denied feeling depressed or having symptoms of mania. Her hair was in pigtails, and she appeared several years younger than her stated age. When her tension mounted, she threw pillows at the window and at the intravenous (IV) pole beside her bed while crying uncontrollably and pleading to go home.
WHAT IS REGRESSION?
According to Sigmund Freud,1 regression is an unconscious defense mechanism, which causes the temporary or long-term reversion of the ego to an earlier stage of development (instead of handling unacceptable impulses in a more adult manner). Regression is typical in normal childhood, and it can be caused by stress, by frustration, or by a traumatic event. Children usually manifest regressive behavior to communicate their distress. Addressing the underlying unmet need in the child usually corrects the regressive behavior.
Regression in adults can arise at any age; it entails retreating to an earlier developmental stage (emotionally, socially, or behaviorally). Insecurity, fear, and anger can cause an adult to regress. In essence, individuals revert to a point in their development when they felt safer and when stress was nonexistent, or when an all-powerful parent or another adult would have rescued them.
Regressive behavior can be simple or complex, harmful or harmless to the individual showing the behavior and to those around them. Regression becomes problematic, especially in a hospital, when it is employed to avoid difficult adult situations or stressors. Managing regression in a hospital is resource intensive and can prolong hospital stays.2–5
Regression has been portrayed in a more positive light by others (eg, psychologists like Carl Jung), who have argued that an individual’s regressive tendency is not just a relapse into infantilism, but an attempt to achieve something important (eg, a universal feeling of childhood innocence, a sense of security, reciprocated love, and trust).6,7
WHAT ARE THE MANIFESTATIONS OF REGRESSION?
Many psychoanalysts have observed that behaviors associated with regression are correlated with the psychological stage at which the person is fixated. For example, an individual fixated at the oral stage might suck on a pen, eat impulsively, vomit, or become verbally aggressive, while an individual fixated at the anal stage might be messy or untidy and an individual fixated at the phallic stage would revert to physical symptoms or to a state of conversion hysteria. Sometimes, a regressed patient might stop talking and give all the signs that a distressed baby would show during a preverbal stage. In adults, regressive behavior is manifest in myriad ways (Table 1 lists common regressive behaviors exhibited by hospitalized patients).

Many children (eg, when tired, hungry, or afraid) have temper tantrums (expressions of strong emotions) on a daily basis until they are 3 or 4 years old.8 In fact, preschoolers with a DSM-IV diagnosis (such as depression) displayed significantly more violence during tantrums (with a difficult recovery) compared to healthy preschoolers.9 Moreover, temper tantrums are a frequent reason for referral to behavior therapists and are among the most common behavior problems of childhood.10,11 Some of the behaviors associated with childhood tantrums include shouting, screaming, crying, falling to the floor, flailing their extremities, hitting, kicking, throwing items, and having breath-holding spells.11 Tantrums may also start with shouting and angry outbursts followed by sobbing, withdrawing, and seeking comfort.12
Adults with temper tantrums have them for the same reasons as children (ie, being distressed). Being hospitalized is stressful for some adults; this can fuel tantrums. Adults with temper tantrums exhibit some or all of the behaviors exhibited by children. Unfortunately, in hospital settings, temper tantrums can be disruptive and pose management problems for clinical staff members who have to care for more than 1 patient at a time.
Engaging in quiet baby talk, also referred to as infant-directed speech, can be a manifestation of regression in adults. Compared to adult-directed talk, baby talk has a higher mean fundamental frequency, a wider range, and a more musical rhythm.13 While some scholars consider baby talk as a universal and a species-specific adaptation, others find it to be more prevalent in certain cultures.14,15 Baby talk is often employed by adults when communicating with babies and infants, and it can serve various functions (including communication of affective intentions essential in the emotional bonding between adults and babies).14,16 When it is not a show of regressive behavior, adults can also employ baby talk when characterizing victims as weak or cowards (eg, while bullying).
Adults who need assistance with grooming or feeding may also be considered as regressed. Among hospitalized patients, being incontinent of urine (or bed-wetting) or stool can also be a manifestation of regression. An inability to perform basic activities of self-care is often heightened during periods of stress, even if the underlying disability is caused by a medical or psychological illness.
While some acutely distressed individuals (eg, those in pain) can assume a fetal position and cry in response to their suffering (physical or emotional), others prefer to cuddle with a stuffed animal (eg, a teddy bear). It is important to note that crying in the hospital can communicate distress caused by a variety of challenging situations (including loss, pain, anxiety, or fear) or in response to positive emotions (such as joy and the news of a good prognosis).
HOW COMMON IS REGRESSION AMONG HOSPITALIZED PATIENTS?
Unfortunately, studies specifically addressing the prevalence of regressive behavior in general hospital patients are lacking. However, the crisis caused by illness leads to regressive behavior that is accompanied by utilization of primitive defense mechanisms.17,18 At times, hospitalized patients with regressive behavior are referred to as “agitated.” However, no studies have distinguished agitation and regressive behavior. Given the high prevalence of agitation among general hospital patients, it is likely that regressive behavior is also quite prevalent.19–21
WHAT IS THE DIFFERENTIAL DIAGNOSIS
FOR REGRESSION?
The source of regressive behavior is broad and includes both medical and psychiatric problems. Correctly identifying the etiology of the distress that leads to the regressive behavior informs management and provides insights into how the behaviors can be prevented. Potential etiologies of regressive behavior in patients in general medical hospitals are provided below.
Poor Coping
Coping is a normal adaptation to stress.22 Regressive behavior can be a manifestation of inadequate or maladaptive coping; some patients employ immature defense mechanisms to manage the stress of illness. A patient who is overwhelmed by a diagnosis might automatically exhibit 1 or many regressive behaviors. In addition to communicating one’s level of distress, regressive behaviors usually provoke others to provide them more attention, which reinforces the regressive behavior.
Catatonia
Catatonia, a syndrome with diverse motoric and behavioral signs, is seen most often in patients with general medical conditions and mood disorders.23 According to the DSM-5, catatonia is defined by the presence of 3 or more of the following features: catalepsy (ie, passive induction of a posture held against gravity), waxy flexibility (ie, slight and even resistance to positioning by the examiner), stupor (ie, a paucity of psychomotor activity; improper interactions with the environment), agitation not influenced by external stimuli, mutism (ie, no or very little verbal response), negativism (ie, opposing or not responding to instructions or external stimuli), posturing (ie, spontaneous and active maintenance of a posture against gravity), mannerisms (ie, odd caricature of normal actions), stereotypies (ie, repetitive, abnormally frequent, non–goal-directed movements), grimacing, echolalia (ie, mimicking another’s speech), and echopraxia (ie, mimicking another’s movement).24 A host of medical conditions and their complications are associated with catatonia. Some of the aforementioned signs associated with catatonia can be considered as, or confused with, regressive behavior.
Psychotic Disorders
Psychotic disorders are severe mental disorders characterized by an altered state of reality or by impairments in one’s ability to respond emotionally or to communicate effectively or behave appropriately. In the DSM-5, categories of psychotic disorders include brief psychotic disorder, schizophreniform disorder, schizophrenia, schizoaffective disorder, and catatonia.25 Patients with a psychotic disorder can have disorganized thoughts and behaviors (eg, having inappropriate emotional responses [like uncontrollable laughter], showing a lack of motivation, disrobing, being poorly groomed, and masturbating in public), which can easily be categorized as regressive behaviors.
Delirium
Delirium (an acute, transient, fluctuating, and reversible neuropsychiatric syndrome characterized by global cognitive dysfunction and impaired attention) is common.26 Fifteen percent to 60% of general hospital patients have delirium,27 rising to about 80% in intensive care unit patients.28 The etiology of delirium is very broad and can be recalled with the mnemonic: “I WATCH DEATH,” representing: Infection, Withdrawal from substances, Acute metabolic disturbances, Trauma, CNS pathology, Hypoxia, Deficiencies (vitamin B, thiamine, niacin, folate), Endocrinopathies, Acute vascular disease, Toxic drugs, and Heavy metal poisoning.23 For a diagnosis of delirium, a patient must have a disturbance of consciousness with a diminished ability to focus or to maintain or shift attention, a change in cognition or the development of a perceptual disturbance not attributed to dementia, fluctuations over the course of the day, and evidence of the disturbance caused by a general medical condition. The clinical features of delirium are diverse and include disorganized behavior, aggression, agitation, disorientation, and an inability to perform activities of grooming and feeding, all of which could be viewed as regressive behaviors.
Major Depressive Disorder
According to the DSM-5, a diagnosis of major depressive disorder requires that an individual have a depressed mood or a loss of interest or pleasure (anhedonia) and at least 4 other neurovegetative changes (including significant weight loss or gain, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished concentration, and recurrent thoughts of death or suicide). These changes must last for at least 2 weeks and must interfere with the patient’s level of functioning. Major depressive disorder can result in regressive behavior and emotions including anhedonia and poor self-care (which might include poor hygiene and grooming).29
Dementia
The DSM-5 categorizes dementia, mild cognitive disorder, and delirium as neurocognitive disorders.30 The prevalence of dementia increases with age—about 20% of individuals over the age of 65 years and about 45% of individuals over the age of 80 years have a dementing illness.31 Of all causes of dementia, Alzheimer’s dementia accounts for the majority.32 Patients with dementia frequently show a regression in function as evidenced by problems in performing activities of daily living.33,34 The severity of memory decline and the neurodegenerative changes of the brain vary and can be associated with motor deficits35 that account for some of the functional deficits seen in patients with dementia. Regressive behavior in patients with dementia can correlate with the severity of the disease. While patients with early dementia have difficulties completing routine tasks (like writing or driving or cooking), patients with a later stage of dementia require assistance with toileting, feeding, or ambulating.
Dissociative Disorders
Several disorders are characterized by dissociation including depersonalization/derealization disorder (characterized by pervasive and repeated episodes of detachment or estrangement from one’s self [thoughts and body] or a sense that things in one’s environment are not real or both36), dissociative amnesia37 (extreme forgetfulness and inability to recall pertinent personal information [usually traumatic]),23 and dissociative identity disorder (a complex, chronic, posttraumatic psychopathology characterized by alternating subjectively separate identities with recurrent episodes of memory disruption or frank amnesia). Patients with a history of significant trauma often dissociate in stressful situations (such as with hospitalization), and their behaviors are characterized by an inability to regulate body functions and emotions.
Borderline Personality Disorder
According to Stone,38 patients with a borderline personality disorder are especially vulnerable to regression because of their lack of a cohesive self. Toplin39 added that borderline patients have a cohesive self, but it is a specious and fragile integration sustained through complex defenses rather than an underlying psychic structure. Environments that lack structure promote regression in patients with borderline personality disorder. General hospital inpatient floors can be chaotic for patients with borderline personality, threatening their sense of object constancy and fostering regression. The patient with borderline personality is vulnerable and lacks ego development; as a result, he or she becomes exposed in hospital settings and destabilizes, especially in situations in which there is lack of collaboration and coordination among members of the care team.
Substance Abuse Disorders
Patients who are intoxicated or undergoing withdrawal from substances may display regressive behaviors. Patients with opioid intoxication can be psychomotorically agitated or retarded, have slurred speech, or have impairments in memory and cognition.40 Alcohol intoxication also causes impairment in attention and memory coupled with impulsivity; patients who are intoxicated with alcohol display impaired coordination (eg, stumbling, loss of fine motor skills), speech difficulties (slurred speech), mood lability, poor attention, and disorganization, all of which can be considered regressive.
HOW CAN REGRESSION IN HOSPITALIZED
PATIENTS BE EVALUATED?
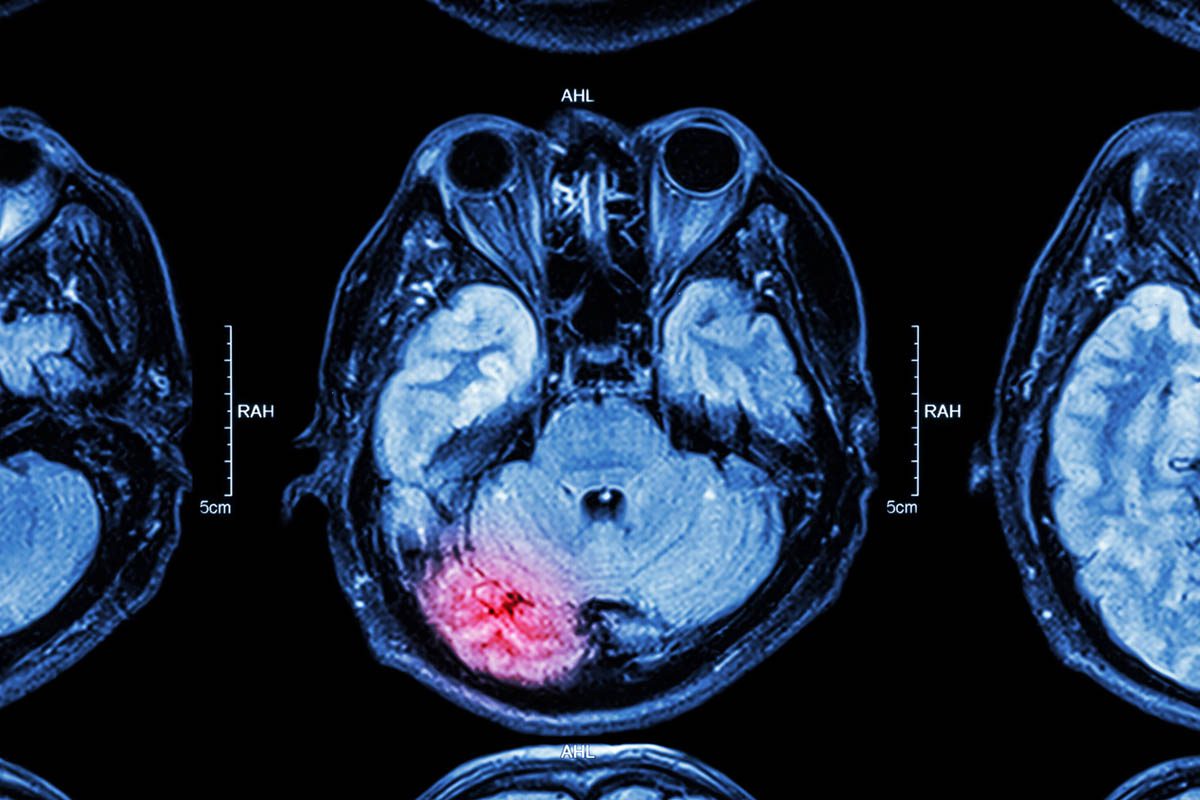
Although there are no evidence-based studies on how to evaluate patients with regressive behaviors, the differential diagnosis for regression is broad, and it should guide the evaluation of its potential etiologies. A thorough medical history, including a psychiatry history, a substance abuse history, a social history, medication use (both previous and current), a trauma/abuse history, and a family history can all provide clues about the etiology. Laboratory screening should include a basic metabolic panel, complete blood count, urinalysis, and toxicology screens. Head imaging and other radiologic studies can be obtained when there is a greater index of suspicion of disease. Consultants, not limited to neurologists or psychiatrists, can be involved for further evaluations and testing if a neurologic or psychiatric illness is suspected.
WHO SHOULD EVALUATE REGRESSION
IN HOSPITALIZED PATIENTS?
Any clinician who notices or suspects regressive behavior should explore and evaluate the patient, since some of the potential etiologies (like delirium and catatonia) require urgent treatment. In adults, just as in children, regressive behavior is often exacerbated when it is ignored, especially when a patient resorts to regression to communicate distress or a cry for help.
HOW CAN ONE MANAGE REGRESSION IN HOSPITALIZED PATIENTS?
Although there are no evidence-based studies on how to manage regression in hospitalized patients, clinical experience suggests that the first step in managing regression is to address any underlying medical, neurologic, or psychiatric problem. Depending on the etiology, several interventions (behavioral, pharmacologic, nonpharmacologic) can be employed.
Behavioral interventions include empathizing with patients regarding their perceived stress (eg, being in the hospital; dealing with pain, loss, anxiety, fear, loneliness). It is also useful to ask how the patient is feeling and to name some of the suspected emotions he or she could be experiencing. In some cases, taking a parental position of authority and nurturance could de-escalate the behavior. Some psychologists advocate for joining patients in their “child place” for alignment building. A behavior plan created by the multidisciplinary team caring for the patient (including nurses, physicians, social workers, and therapists) that outlines for the patient the expectations of the team and helps to create structure for the patient can prevent regression.
Pharmacologic interventions include use of antidepressants for patients with depression; benzodiazepines for patients with catatonia, anxiety, or fear; and antipsychotics for patients with psychosis, anxiety, or fear. In situations in which pain is the primary problem, aggressive pain management (with the help of pain specialists) can be useful. Electroconvulsive therapy can also be used to treat patients with depression (that is refractory to medications) or catatonia.
CASE VIGNETTE, CONTINUED
Ms A had a temper tantrum during her psychiatric evaluation (ie, a regressive behavior characterized by throwing pillows at her window and knocking down her IV pole, crying uncontrollably, hanging onto a stuffed animal for comfort, shouting and yelling at her interviewers). She was clearly distressed by her persecutory delusions and auditory hallucinations; this behavior was in addition to a long-standing history of dependent personality traits. She did not seem to have the ability to self-soothe or to cope with the stress of her psychosis or of being in the hospital; throwing a temper tantrum was Ms A’s method of communicating her distress to those around her. This behavior resulted in Ms A receiving a bevy of attention from her primary team. She responded well to reassurance by team members and to antipsychotic medications that targeted her psychosis.
CONCLUSION
Regression entails retreating to an earlier developmental form of function (emotionally, socially, and behaviorally) in times of stress. Inpatient hospitalization is a source of stress for many patients (like Ms A); hence, a variety of regressive behavior is displayed by patients in general hospital settings. The potential etiologies for regressive behavior are vast and can include serious medical, neurologic, or psychiatric conditions. Any clinician working with a patient who appears regressed should explore and evaluate the patient to rule out serious medical and psychiatric conditions and to inform treatment strategies. Ignoring regression usually exacerbates the behavior. Regression becomes a problem in hospitals when it is viewed as the only alternative to avoiding adult situations or stress. Although there is no evidenced-based literature on how to manage regression, several behavioral, pharmacologic, and nonpharmacologic interventions have proved useful in caring for patients with regressive behavior.
REFERENCES
1. Freud S, Strachey J. Introductory Lectures on Psychoanalysis. New York, NY: Norton; 1977.
2. Hooley JM, Wilson-Murphy M. Adult attachment to transitional objects and borderline personality disorder. J Pers Disord. 2012;26(2):179–191. doi:10.1521/pedi.2012.26.2.179 PubMed
3. Guinjoan SM, Ross DR, Perinot L, et al. The use of transitional objects in self-directed aggression by patients with borderline personality disorder, anorexia nervosa, or bulimia nervosa. J Am Acad Psychoanal. 2001;29(3):457–467. doi:10.1521/jaap.29.3.457.17299 PubMed
4. Potegal M, Carlson G, Margulies D, et al. Rages or temper tantrums? the behavioral organization, temporal characteristics, and clinical significance of angry-agitated outbursts in child psychiatry inpatients. Child Psychiatry Hum Dev. 2009;40(4):621–636. doi:10.1007/s10578-009-0148-7 PubMed
5. Gold J, Shera D, Clarkson B Jr. Private psychiatric hospitalization of children: predictors of length of stay. J Am Acad Child Adolesc Psychiatry. 1993;32(1):135–143. doi:10.1097/00004583-199301000-00020 PubMed
6. Jung CG, Read H, Fordham M, et al. The Collected Works of CG Jung.
New York, NY: Pantheon Books; 1953.
7. Balint M. The Basic Fault: Therapeutic Aspects of Regression. London, UK: Tavistock Publications; 1968.
8. Potegal M, Kosorok MR, Davidson RJ. Temper tantrums in young children: 2. tantrum duration and temporal organization. J Dev Behav Pediatr. 2003;24(3):148–154. doi:10.1097/00004703-200306000-00003 PubMed
9. Belden AC, Thomson NR, Luby JL. Temper tantrums in healthy versus depressed and disruptive preschoolers: defining tantrum behaviors associated with clinical problems. J Pediatr. 2008;152(1):117–122. doi:10.1016/j.jpeds.2007.06.030 PubMed
10. Potegal M, Davidson RJ. Temper tantrums in young children: 1. behavioral composition. J Dev Behav Pediatr. 2003;24(3):140–147. doi:10.1097/00004703-200306000-00002 PubMed
11. Daniels E, Mandleco B, Luthy KE. Assessment, management, and prevention of childhood temper tantrums. J Am Acad Nurse Pract. 2012;24(10):569–573. doi:10.1111/j.1745-7599.2012.00755.x PubMed
12. Potegal M, Kosorok MR, Davidson RJ. The time course of angry behavior in the temper tantrums of young children. Ann N Y Acad Sci. 1996;794:31–45. doi:10.1111/j.1749-6632.1996.tb32507.x PubMed
13. Fernald A. Intonation and communicative intent in mothers’ speech to infants: is the melody the message? Child Dev. 1989;60(6):1497–1510. doi:10.2307/1130938 PubMed
14. Bryant GA, Barrett HC. Recognizing intentions in infant-directed speech: evidence for universals. Psychol Sci. 2007;18(8):746–751. doi:10.1111/j.1467-9280.2007.01970.x PubMed
15. Liu HM, Tsao FM, Kuhl PK. Age-related changes in acoustic modifications of Mandarin maternal speech to preverbal infants and five-year-old children: a longitudinal study. J Child Lang. 2009;36(4):909–922. doi:10.1017/S030500090800929X PubMed
16. Barkow JH, Cosmides L, Tooby J. The Adapted Mind: Evolutionary Psychology and the Generation of Culture. New York, NY: Oxford University Press; 1992.
17. Harrison A, Hart C. Mental Health Care for Nurses: Applying Mental Health Skills in the General Hospital. Malden, MA: Blackwell Publishing; 2006.
18. Bourgeois J, Hales RE, Shahrokh NC. Study Guide to Psychosomatic Medicine. 1st ed. Washington, DC: American Psychiatric Pub; 2011.
19. O’Hara R, Mumenthaler MS, Davies H, et al. Cognitive status and behavioral problems in older hospitalized patients. Ann Gen Hosp Psychiatry. 2002;1(1):1. doi:10.1186/1475-2832-1-1 PubMed
20. Stern TA, Celano CM, Gross AF, et al. The assessment and management of agitation and delirium in the general hospital. Prim Care Companion J Clin Psychiatry. 2010;12(1):PCC.09r00938. doi:10.4088/pcc.09r00938yel PubMed
21. Servis M. Managing agitated patients in a general hospital. West J Med. 1996;164(3):257–258. PubMed
22. Blair RJ, Morris JS, Frith CD, et al. Dissociable neural responses to facial expressions of sadness and anger. Brain. 1999;122(pt 5):883–893. doi:10.1093/brain/122.5.883 PubMed
23. Stern TA, Herman JB; Massachusetts General Hospital Psychiatry Update and Board Preparation. New York, NY: McGraw-Hill; 2000.
24. Tandon R, Heckers S, Bustillo J, et al. Catatonia in DSM-5. Schizophr Res. 2013;150(1):26–30. doi:10.1016/j.schres.2013.04.034 PubMed
25. Parker GF. DSM-5 and psychotic and mood disorders. J Am Acad Psychiatry Law. 2014;42(2):182–190. PubMed
26. Stern TA, Herman JB, Slavin PL. MGH Guide to Psychiatry in Primary Care. New York, NY: McGraw-Hill, Health Professions Division; 1998.
27. Stern TA, Massachusetts General Hospital. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 1st ed. Philadelphia, PA: Mosby/Elsevier; 2008.
28. Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care. 2008;12(suppl 3):S3. doi:10.1186/cc6149 PubMed
29. Buberman V, Prudkov I, Sorkin Iu. Moiseĭ Izraĭlevich Sakharov (on his 70th birthday) [article in Russian]. Vestn Khir Im I I Grek. 1975;114(9):135. PubMed
30. Sachdev PS, Blacker D, Blazer DG, et al. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol. 2014;10(11):634–642. doi:10.1038/nrneurol.2014.181 PubMed
31. Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia:
a systematic review and meta-analysis. Alzheimers Dement. 2013;9(1):63–75, e2. doi:10.1016/j.jalz.2012.11.007 PubMed
32. Evans DA, Funkenstein HH, Albert MS, et al. Prevalence of Alzheimer’s disease in a community population of older persons: higher than previously reported. JAMA. 1989;262(18):2551–2556. doi:10.1001/jama.1989.03430180093036 PubMed
33. Mokhtari M, Aloulou H, Tiberghien T, et al. New trends to support independence in persons with mild dementia: a mini-review. Gerontology. 2012;58(6):554–563. doi:10.1159/000337827 PubMed
34. Arrighi HM, Gélinas I, McLaughlin TP, et al. Longitudinal changes in functional disability in Alzheimer’s disease patients. Int Psychogeriatr. 2013;25(6):929–937. doi:10.1017/S1041610212002360 PubMed
35. Marshall GA, Amariglio RE, Sperling RA, et al. Activities of daily living: where do they fit in the diagnosis of Alzheimer’s disease? Neurodegener Dis Manag. 2012;2(5):483–491. doi:10.2217/nmt.12.55 PubMed
36. Sierra M, David AS. Depersonalization: a selective impairment of
elf-awareness. Conscious Cogn. 2011;20(1):99–108. doi:10.1016/j.concog.2010.10.018 PubMed
37. Coons PM. The dissociative disorders: rarely considered and underdiagnosed. Psychiatr Clin North Am. 1998;21(3):637–648. doi:10.1016/S0193-953X(05)70028-9 PubMed
38. Stone MH. Management of borderline personality disorder: a review of psychotherapeutic approaches. World Psychiatry. 2006;5(1):15–20. PubMed
39. Tolpin M. Self-objects and oedipal objects: a crucial developmental distinction. Psychoanal Study Child. 1978;33:167–184. PubMed
40. Fareed A, Stout S, Casarella J, et al. Illicit opioid intoxication: diagnosis and treatment. Subst Abus. 2011;5:17–25. PubMed
LESSONS LEARNED AT THE INTERFACE
OF MEDICINE AND PSYCHIATRY
The Psychiatric Consultation Service at Massachusetts General Hospital (MGH) sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Dr Lokko is a third-year resident in the Massachusetts General Hospital/McLean Hospital Psychiatry Residency Training Program and a clinical fellow in psychiatry at Harvard Medical School, Boston, Massachusetts. Dr Stern is chief of the Avery D. Weisman Psychiatry Consultation Service at Massachusetts General Hospital and the Ned H. Cassem professor of psychiatry in the field of psychosomatic medicine/consultation at Harvard Medical School, Boston, Massachusetts.
Dr Stern is an employee of the Academy of Psychosomatic Medicine, has served on the speaker’s board of Reed Elsevier, is a stock shareholder in WiFiMD (Tablet PC), and has received royalties from Mosby/Elsevier and McGraw Hill. Dr Lokko reports no conflict of interest related to the subject of this article.
Prim Care Companion CNS Disord 2015;17(3):doi:10.4088/PCC.14f01761
© Copyright 2015 Physicians Postgraduate Press, Inc.
Submitted: December 08, 2014;
accepted February 02, 2015.
Published online: May 14, 2015.
Potential conflicts of interest: None reported.
Funding/support: None reported.
Corresponding author: Hermioni N. Lokko, MD, MPP, Department of Psychiatry, Massachusetts General Hospital and McLean Hospital, 15 Parkman St Wang ACC-812, Boston, MA 02114 ([email protected]).
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top