When Depression Hides a Brain Tumor:
A Case of Glioblastoma
Glioblastoma (World Health Organization [WHO] grade IV glioma) is the most common and aggressive primary intrinsic brain neoplasm with a mean survival of 15 months.1,2 Whereas brain neoplasm characteristically causes focal neurologic disturbances, it is not uncommon for brain tumors to present with neurobehavioral changes in the absence of any localized signs or deficits. As both the disease and its treatment have a direct effect on brain functioning, patients commonly experience neurologic, cognitive, and psychiatric symptoms that greatly affect their daily life.3,4
Case Report
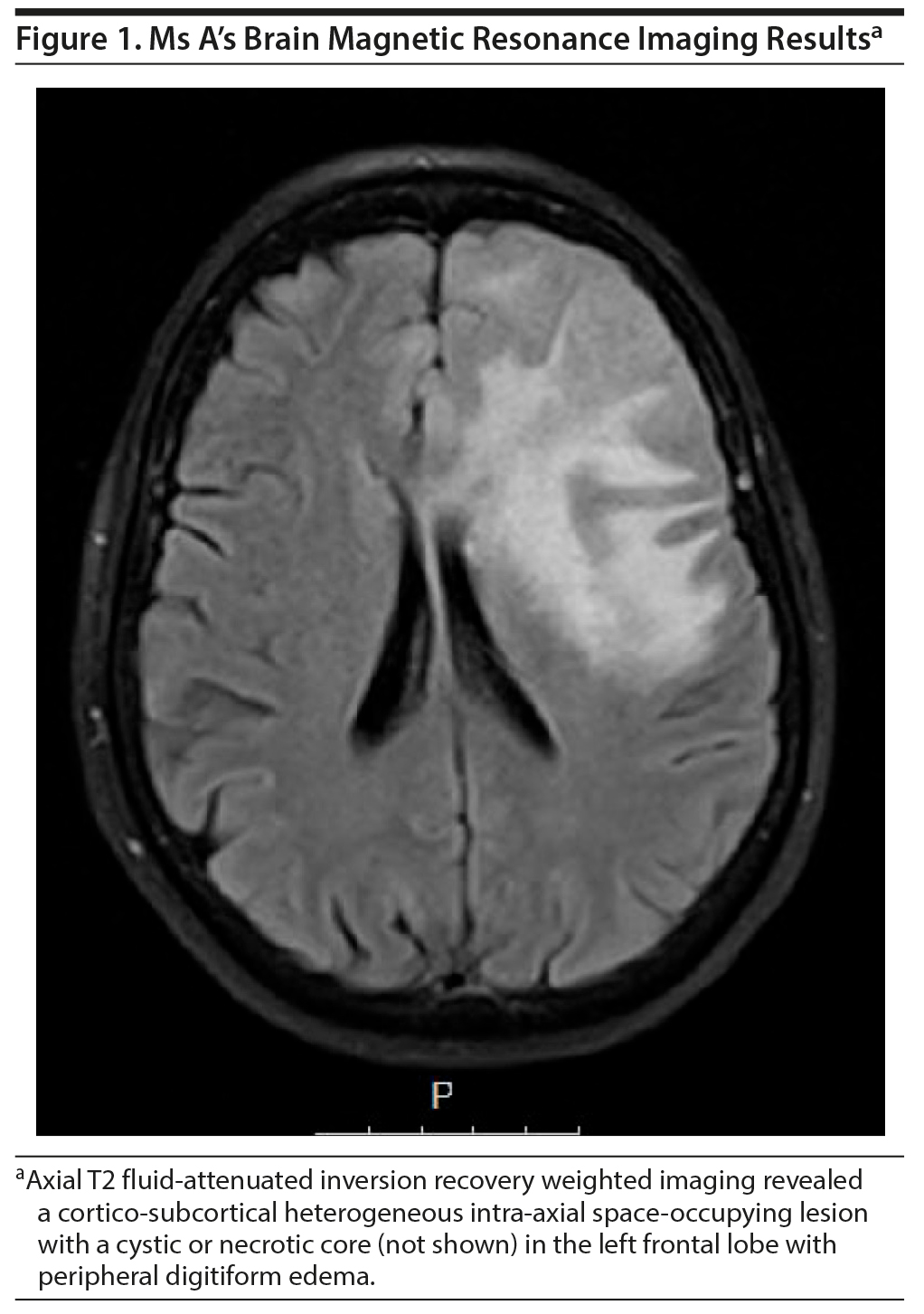
A 69-year-old white woman with a psychiatric history of intermittent and recurrent depression for 15 years has had a poor response to different trials of antidepressants. She maintained anhedonia, low energy, and insomnia. She had a previous suicide attempt 5 years prior. Twelve months before hospital admission, she developed depressed mood, apathy, and inability to care for herself; markedly decreased appetite; and sleep deprivation. Because she was unresponsive to appropriate antidepressant medication and presented with recent cognitive functioning impairment, including significant deterioration in memory, attention, verbal fluency, cognitive flexibility, and visual search, a protocol was followed to rule out an organic etiology, starting with the exclusion of the diagnosis of delirium. Her routine laboratory tests were within normal limits, and a brain computed tomography (CT) scan followed by brain magnetic resonance imaging (MRI) revealed a left frontal lobe mass (Figure 1). Surgical resection of the lesion was performed, and the biopsy indicated a glioblastoma IDH1 negative (WHO grade IV). The patient maintained depressive symptoms after surgery, even after optimization of the antidepressant therapy. However, she showed improvements in memory and a significant improvement in language functioning.
Discussion
In this case, a patient with an established diagnosis of chronic recurrent depression, a recent change in clinical presentation, and a significant aggravation of her general state presented with recent onset of de novo cognitive symptoms and functional impairment in daily activities coupled with persistent atypical psychiatric symptoms and a poor response to treatment. These changes led to the suspicion of organic etiology, including metabolic alterations, infectious and vascular diseases, tumors, autoimmune or neurodegenerative brain diseases, and other causes of rapidly progressing dementias.
This case illustrates the need for prompt assessment when the clinical presentation changes or is unusual. It is impossible to know when the patient’s tumor started to grow, but a prompt brain CT followed by a brain MRI could have helped to detect the mass earlier.
Gliomas cause symptoms by invading into and creating pressure in nearby normal brain tissue. The most common symptoms include cognitive changes, headache, and seizures. Significantly, neurocognitive status is a predictor of survival in the older population of newly diagnosed high-grade glioma patients.5 Also, it is known that depression is a considerable hidden morbidity among patients with glioma6: it has been described in 2.5%-15.4% of primary brain tumors and was found in 44% of all patients with primary and metastatic brain tumor.7 Depression was associated with functional impairment, cognitive dysfunction, reduced quality of life, and reduced survival.8 Mood issues can be attributed to side effects of treatment, biochemical changes in the brain,9 changes in cytokine levels,10 elevated intracranial pressure, or the location of the tumor.
Most brain tumors present with specific neurologic signs due to mass effect; however, in rare cases they may present primarily with psychiatric symptoms.11 Frontal cortex lesions—lesions in the parietal association cortex and paralimbic structures—have been associated with mood changes.3,11 Iatrogenic causes include neurochemical imbalance and the direct destructive effect of glioma or surgery on critical emotional pathways.6 In terms of psychogenesis, depression may be seen in different stages (before, during, or after diagnosis and treatment). Patients with functional impairment or who were previously depressed are at higher risk of developing depression.8
This case represents an ambiguous psychiatric history as well as the progression of a disease in which the neuropsychiatric symptoms were the initial manifestations of a primary brain tumor. Depression can persist after glioblastoma treatment, affecting patient quality of life. Early detection is important, and we emphasize the importance of considering neuroimaging studies in patients presenting atypical clinical presentations or with de novo cognitive symptoms.
Published online: November 14, 2019.
Potential conflicts of interest: None.
Funding/support: None.
Patient consent: Consent was obtained from the patient’s legal guardian to publish the case report and brain scan.
REFERENCES
1.Hanif F, Muzaffar K, Perveen K, et al. Glioblastoma multiforme: a review of its epidemiology and pathogenesis through clinical presentation and treatment. Asian Pac J Cancer Prev. 2017;18(1):3-9. PubMed
2.Thakkar JP, Dolecek TA, Horbinski C, et al. Epidemiologic and molecular prognostic review of glioblastoma. Cancer Epidemiol Biomarkers Prev. 2014;23(10):1985-1996. PubMed CrossRef
3.Boele FW, Rooney AG, Grant R, et al. Psychiatric symptoms in glioma patients: from diagnosis to management. Neuropsychiatr Dis Treat. 2015;11:1413-1420. PubMed CrossRef
4.Mukand JA, Blackinton DD, Crincoli MG, et al. Incidence of neurologic deficits and rehabilitation of patients with brain tumors. Am J Phys Med Rehabil. 2001;80(5):346-350. PubMed CrossRef
5.Bosma I, Vos MJ, Heimans JJ, et al. The course of neurocognitive functioning in high-grade glioma patients. Neuro-oncol. 2007;9(1):53-62. PubMed CrossRef
6.Rooney AG, Brown PD, Reijneveld JC, et al. Depression in glioma: a primer for clinicians and researchers. J Neurol Neurosurg Psychiatry. 2014;85(2):230-235. PubMed CrossRef
7.Mainio A, Hakko H, Niemelä A, et al. Depression in relation to anxiety, obsessionality and phobia among neurosurgical patients with a primary brain tumor: a 1-year follow-up study. Clin Neurol Neurosurg. 2011;113(8):649-653. PubMed CrossRef
8.Rooney AG, Carson A, Grant R. Depression in cerebral glioma patients: a systematic review of observational studies. J Natl Cancer Inst. 2011;103(1):61-76. PubMed CrossRef
9.Starkweather AR, Sherwood P, Lyon DE, et al. A biobehavioral perspective on depressive symptoms in patients with cerebral astrocytoma. J Neurosci Nurs. 2011;43(1):17-28. PubMed CrossRef
10.Starkweather AR, Sherwood P, Lyon DE, et al. Depressive symptoms and cytokine levels in serum and tumor tissue in patients with an astrocytoma: a pilot study. BMC Res Notes. 2014;7(1):423. PubMed CrossRef
11.Madhusoodanan S, Ting MB, Farah T, et al. Psychiatric aspects of brain tumors: a review. World J Psychiatry. 2015;5(3):273-285. PubMed CrossRef
aDepartment of Psychiatry and Mental Health, Hospital Distrital de Santarém, Santarém, Portugal
bNeuroradiology Department, Centro Hospitalar e Universitסrio Lisboa Central, Lisbon, Portugal
cDepartment of Psychiatry, Hospital Santa Maria, Centro Hospitalar Lisboa Norte, Lisbon, Portugal
*Corresponding author: Liliana P. Ferreira, MD, Department of Psychiatry and Mental Health, Hospital Distrital de Santarém, EPE, Ave Bernardo Santareno 3737B, 2005-177 Santarém, Portugal ([email protected]).
Prim Care Companion CNS Disord 2019;21(6):19l02455
To cite: Ferreira LP, Pinheiro CF, Fernandes NA, et al. When depression hides a brain tumor: a case of glioblastoma. Prim Care Companion CNS Disord. 2019;21(6):19l02455.
To share: https://doi.org/10.4088/PCC.19l02455
© Copyright 2019 Physicians Postgraduate Press, Inc.
Enjoy free PDF downloads as part of your membership!
Save
Cite
Advertisement
GAM ID: sidebar-top